Case 69
Presentation
A 45-year-old woman presented to her dermatologist after noticing a suspicious lesion on her left thigh. An excisional biopsy performed in the office demonstrated a 1.8-mm superficial spreading melanoma with ulceration. The patient now presents to your office for definitive surgical management. On physical examination, there is a well-healed longitudinal scar on the right thigh and a palpable 1.5-cm, mobile, firm lymph node in the left groin.
Differential Diagnosis
Any patients diagnosed with invasive melanoma should undergo a thorough physical examination, paying particular attention to the regional draining lymph node basins. Approximately 5% of patients will present with clinically apparent regional lymph node involvement at the time of diagnosis. Still others develop palpable lymphadenopathy months or years after excision of a primary melanoma, while occasional patients present with nodal metastasis in the absence of a detectable primary tumor. Regional lymph nodes may become enlarged due to infection, inflammation, or reactive hyperplasia, particularly after a biopsy of the primary tumor has been performed. However, any palpable nodes that are larger than 1 to 1.5 cm in size, hard, or fixed to adjacent structures must be considered suspicious for metastatic involvement. Metastatic nodal involvement can be reliably verified in most cases with a fine-needle aspiration biopsy. Excisional biopsy should be reserved for situations in which the node is clinically suspicious but the aspiration biopsy is negative or indeterminate, because the complications of an open biopsy (including seroma, infection, and scarring) can interfere with the performance of a subsequent lymph node dissection. If an excisional biopsy is performed, it is important to orient the incision so that it can be readily re-excised during the complete lymph node dissection if the node proves to be involved with tumor.
Diagnosis
Fine-needle aspiration biopsy confirms the presence of metastatic melanoma.
▪ Approach
Unfortunately, once melanoma has spread to the lymph nodes, there is a steep drop-off in survival. The 5-year survival rate for patients with node-positive melanoma (American Joint Committee on Cancer [AJCC] stage III) is 49%, and declines to 37% at 10 years. Not all stage III melanoma patients, however, have the same outlook: 5-year survival rates range from 13% for patients with a combination of poor risk factors (ulceration, high regional lymph node burden) to 69% for patients with a more favorable profile. It is imperative to keep in mind that node-positive melanoma is a potentially curable disease, and an aggressive surgical approach is warranted. A patient such as this one, with biopsy-proven palpable nodal involvement, should undergo wide local excision of the primary tumor and complete lymph node dissection if there is no radiologic evidence of distant metastasis.
In the presence of metastatic disease, however, the value of regional node dissection is limited, and should be restricted to selected patients with present or impending symptoms from their nodal disease. Metastatic workup should be performed to evaluate any patient presenting with clinical stage III disease. The most important part of this workup is a detailed history and physical examination. The history should include a thorough review of symptoms, focusing on symptoms consistent with metastatic disease, including any neurologic symptoms from possible brain metastases. The presence of any unusual symptoms should prompt the appropriate imaging and, where appropriate, histologic confirmation. The physical examination should include a careful search for in-transit metastases, distant skin or subcutaneous metastases, or lymphadenopathy outside of the regional basin(s).
In addition to the history and physical examination, all patients with stage III disease should have a chest radiograph and a serum lactate dehydrogenase (LDH) level measurement. Patients with abnormalities on chest x-ray or an elevated LDH level should undergo a further search for metastatic disease. This should consist of a computed tomography (CT) scan of the chest, abdomen, and pelvis and magnetic resonance imaging (MRI) or CT of the brain. The use of positron-emission tomography (PET) scanning has also been advocated; the value of this technique is discussed in more detail subsequently.
More controversial is the extent of further imaging studies required in the asymptomatic patient with a normal chest x-ray and LDH level. When the chest x-ray is normal, a chest CT scan adds little value. CT scan or MRI of the brain is not routinely necessary in asymptomatic patients. For patients such as the present case with palpable inguinal adenopathy, a CT of the abdomen and pelvis will not only evaluate for the presence of intra-abdominal metastasis, but can also identify enlarged pelvic lymph nodes that might convert a superficial inguinal node dissection to a superficial and deep dissection. For patients with palpable axillary or cervical lymph nodes, the added value of further imaging is less clear.
Whole-body PET scanning has emerged as a potentially valuable tool for preoperative evaluation of melanoma patients. In patients with stage III disease, PET scanning has been reported to be superior to CT scans, upstaging patients to stage IV (and hence altering therapy) in 16% to 28% of cases. Combination PET/CT scans are now becoming available and may ultimately prove to be superior to either modality alone, although prospective studies are currently ongoing. Unfortunately, others have not found PET scanning to be reliable, with high false-positive rates. It is important to remember that both CT scans and PET scans can have false-positive findings; histologic confirmation of an abnormal lesion should be obtained whenever feasible before concluding a patient has stage IV melanoma and abandoning a surgical approach.
Recommendation
Chest x-ray, LDH measurement, and CT scan of the abdomen and pelvis are recommended. Further imaging should be done only if positive findings are encountered.
Case Continued
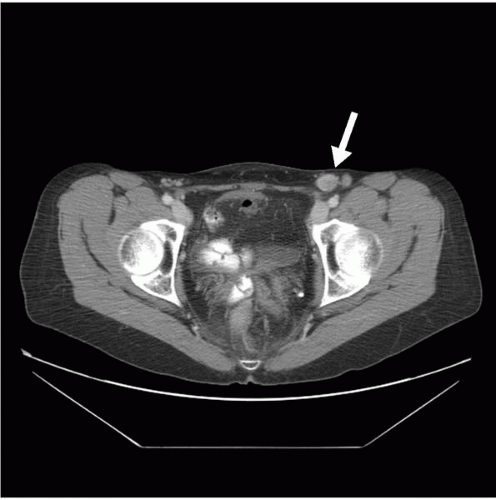
The patient is asymptomatic and physical examination shows no evidence of metastatic disease. The chest x-ray and LDH level are also normal. A CT scan of the abdomen and pelvis shows no areas suspicious for metastatic disease and no enlarged pelvic lymph nodes. However, the metastatic inguinal lymph node was visualized.
▪ Abdomen/Pelvis CT Scan
Abdomen/Pelvis CT Scan Report
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree