Case 64
Presentation
This patient is a 16-year-old girl with a 3-month history of right shoulder pain. The pain is described as occurring intermittently throughout the day. It is not related to any specific activities and tends to be worse at night. There is no history of a traumatic injury to this extremity. Physical examination demonstrates a significant asymmetry when compared with the contralateral shoulder. The right shoulder has a soft-tissue mass adhered to the underlying humerus. It is easily palpable and minimally tender. There are some dilated veins in the skin overlying the right proximal humeral mass. There is no fever or other notable systemic symptoms such as anorexia or weight loss.
Recommendation
Routine blood tests should be performed, including alkaline phosphatase. Perform chest radiograph, anteroposterior (AP) and lateral radiographs of the right proximal humerus and shoulder girdle, bone scan, and computed tomography (CT) or magnetic resonance imaging (MRI) scan of the shoulder girdle. Biopsy should be done to establish tissue diagnosis.
Case Continued
Laboratory examinations including a complete blood cell count (CBC), blood urea nitrogen (BUN), and electrolytes (e.g., alkaline phosphatase, calcium, and phosphorous) are performed, and the alkaline phosphatase is the only result not within normal limit ranges. The reported value of the alkaline phosphatase was markedly high at 600 units. The patient’s white blood count was normal and the sedimentation rate was 18.
A posteroanterior (PA) chest radiograph is normal, but a lytic destructive lesion of the right proximal humerus is easily visualized. AP and lateral radiographs of the right proximal humerus and shoulder girdle show a large, destructive osteolytic and osteoblastic lesion of the proximal third of the humerus. Cortical destruction is observed in these studies. There is a significant soft-tissue component underlying the deltoid muscle, with evidence of extraosseous bone formation arising from the proximal humerus. There is marked periosteal elevation, though the joint space appears to be normal.
CT scans of the right humerus and shoulder girdle show a destructive lesion arising from the right proximal humerus, with a significant soft-tissue component under the deltoid muscle with extraosseous bone formation. The subchondral bone of the humerus is intact without any evidence of destruction or joint involvement by the soft-tissue mass.
MRI examination of the right shoulder girdle demonstrates extensive involvement of the intramedullary space, involving half of the proximal humerus. There is marked cortical destruction corresponding to the finding noted on the CT scan, but a large extraosseous component appears laterally, arising underneath the deltoid. The tumor also extends along the joint capsule. A right shoulder axillary angiogram is performed and demonstrates a hypervascular lesion arising from the right proximal humerus corresponding to the soft-tissue component and bony lesion. There is no obvious evidence of arterial involvement.
▪ Bone Scan
Bone Scan Report
The late phase of a three-phase bone scan shows increased radioisotopic uptake within the proximal right third to half of the proximal humerus, with normal uptake in the ipsilateral glenoid. There is no abnormal uptake in the remaining skeletal system. The most common differential in adolescence is a primary malignant tumor of bone (osteosarcoma vs Ewing sarcoma) or infection. The bone scan is a good study to determine the intraosseous extent of tumor within the medullary canal.
Case Continued
A biopsy is performed under CT guidance with a large needle trocar through a single stab wound through the anterior deltoid. Multiple cores are obtained through this puncture site. A frozen pathology section is obtained at the same time, which demonstrates viable spindle-cell tumor with evidence of osteoid formation. There is no evidence of round cells, giant cells, inflammatory cells, or infection.
Differential Diagnosis
The differential diagnosis of a destructive lesion of the long bones in an adolescent is very suspicious for a primary malignancy. The most common primary malignant bone tumors are osteosarcomas, Ewing sarcomas, and less often, chondrosarcomas or giant cell tumors. In the adolescent population, the most common malignant bone tumors include osteosarcomas and Ewing sarcomas. A finding of a large soft-tissue mass is characteristic of osteosarcomas. Approximately 95% of osteosarcomas are accompanied by an extraosseous mass. This patient’s history of pain is consistent with that of a primary bone tumor. Tumors arising from the skeletal system are often intermittently to excessively painful during the day, but are characteristically most painful at night. Night pain should be a strong warning for malignant bone pathology. It is rare for tumors arising from the bone to actually involve the neurovascular structures, as seen on the angiogram, but often the major vessels are displaced by the tumor mass itself. The alkaline phosphatase values were markedly elevated. This is a hallmark of, and a tumor marker for, osteosarcoma.
A large core needle biopsy harvested several cores (with CT guidance) through the anterior one third of the deltoid muscle. The soft-tissue component was biopsied, not the bone itself. A frozen section of one core showed high-grade spindle-cell sarcoma. The final pathology showed a highly malignant spindle-cell tumor with the tumor stroma making malignant osteoid.
Diagnosis
Osteosarcoma, stage IIB, arising in the right proximal humerus.
▪ Approach
Treatment of osteosarcoma requires a multimodality approach. This includes induction (preoperative) chemotherapy, surgical removal of the tumor by either a limb-sparing procedure or an amputation, and postoperative chemotherapy. Occasionally, the
chemotherapy regimen is modified postoperatively (tailoring), depending on the response of the tumor to the induction chemotherapy. The pathological response is determined by evaluating the amount of tumor necrosis by careful examination and study of the resected tumor mass by a standard pathological technique (i.e., Huvos). Approximately 90% to 95% of all osteosarcomas can today be removed via limb-sparing surgery instead of an amputation. The indications for amputation include massive tumors with neurovascular involvement, pathological fracture, infection, or the occurrence of a tumor in an extremely young (skeletally immature) child.
chemotherapy regimen is modified postoperatively (tailoring), depending on the response of the tumor to the induction chemotherapy. The pathological response is determined by evaluating the amount of tumor necrosis by careful examination and study of the resected tumor mass by a standard pathological technique (i.e., Huvos). Approximately 90% to 95% of all osteosarcomas can today be removed via limb-sparing surgery instead of an amputation. The indications for amputation include massive tumors with neurovascular involvement, pathological fracture, infection, or the occurrence of a tumor in an extremely young (skeletally immature) child.
The specific recommendation for this patient is induction chemotherapy followed by a limb-sparing surgical resection of the right proximal shoulder girdle. There are several different chemotherapy protocols. Typically, the induction phase lasts 12 to 16 weeks. The most common drugs used include doxorubicin (Adriamycin), cisplatin, ifosfamide, and high-dose methotrexate. The tumor is clearly resectable following induction chemotherapy as demonstrated by restaging studies, including repeat CT, MRI, and angiogram of the shoulder. The major nerves and vessels to the arm can be preserved, and the bony resection site can be reconstructed with a metallic endoprosthesis. A modular segmental prosthesis is presently being used for most patients with osteosarcomas. Following surgery and wound healing, patients with osteosarcomas are treated with postoperative chemotherapy for 6 to 12 months, depending upon various protocols.
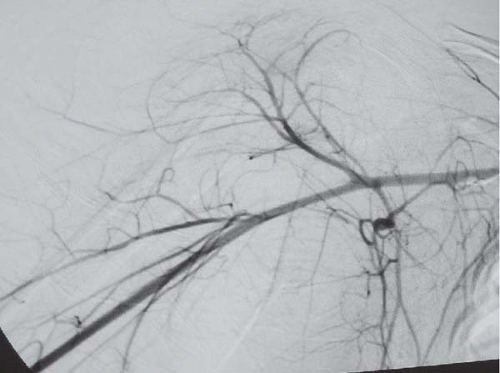
▪ Axillary Angiogram
Axillary Angiography Report
Angiogram (midarterial phase) is performed with the arm placed in the abduction position following induction chemotherapy. Note there is no uptake of contrast within the proximal humerus or the extraosseous component.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree