Case 62
Presentation
A 69-year-old white man presents with a 6-month history of fatigue, early satiety, and an abdominal mass. On examination, there is a large, hard mass to the left of the midline. The inferior border of the mass is somewhat indistinct, suggesting that it extends into the pelvis. The primary physician performs an ultrasound scan, which demonstrates a large intra-abdominal mass occupying the left half of the abdomen and surrounding the kidney and the body and tail of the pancreas.
Differential Diagnosis
The clinical features and the ultrasound scan findings are highly suggestive of a retroperitoneal sarcoma. The differential diagnosis of a retroperitoneal tumor includes lymphoma, germ cell tumors, and undifferentiated carcinomas.
Discussion
Most tumors of the retroperitoneum are malignant. About one third are soft-tissue sarcomas. Soft-tissue sarcomas are rare tumors, with an annual incidence around 2 to 3 per 100,000. Overall, soft-tissue sarcomas comprise <1% of all malignant tumors, and they account for 2% of the total cancer-related mortality. About 15% of all patients with soft-tissue sarcomas present with disease arising in the retroperitoneum. Retroperitoneal sarcomas have a peak incidence in the fifth decade of life. In patients with retroperitoneal neoplasms, 82% are malignant, 18% are benign. Of those with malignancies, 40% are lymphomas or a variety of urogenital cancer, and 55% are sarcomas. Stated another way, nearly one half of all retroperitoneal solid neoplasms will prove to be soft-tissue sarcomas. Patients most frequently present with a nontender palpable mass (80% to 90%). They may give a history of increasing abdominal girth and frequently (40% to 70%) describe vague, poorly localized discomfort due to stretching of the peritoneum. One third of patients have some distal neurologic signs and symptoms from the mass effect, stretching or compression of the lumbar or pelvic nerve plexuses. Gastrointestinal symptoms of a partially obstructive nature, due to displacement or direct invasion by the expanding mass, are found in 10% to 15% of the patients.
The rarity of retroperitoneal sarcomas and their location make it common for these tumors to be misdiagnosed preoperatively. Most often, retroperitoneal sarcomas are diagnosed as ovarian malignancies, but other diagnoses are possible, including genital, urinary, and gastrointestinal tumors, adrenal tumors, and metastatic tumors. History of fever and night sweats with findings of generalized lymphadenopathy and elevated lactate dehydrogenase levels suggest lymphoma. In men, a testicle mass or mass with elevated beta-human chorionic gonadotrophin or alpha-fetoprotein levels suggests a germcell tumor.
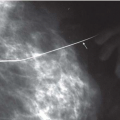
The most definitive radiographic study is a computed tomography (CT) scan of the abdomen and pelvis, because it will establish the retroperitoneal location of such tumors, and they are often heterogenous in appearance due to the presence of solid viable tumor intermixed with areas of necrosis and possible hemorrhage. The CT scan allows definition of the extent of the tumor and its relationships to the surrounding intra-abdominal organs, and particularly, the major vessels. Any discontinuous disease within the abdomen will also be revealed, and the liver can be assessed for the presence of metastases. A CT scan of the chest will disclose metastases that could influence future operative management. In situations where better definition of the tumor in relation to the spine and major vascular structures is necessary for operative planning, a magnetic resonance (MR) scan can be obtained. In addition, it has the advantage of providing an MR angiogram of the aorta and/or vena cava to evaluate displacement, encasement, thrombosis, and/or direct invasion. Any extension through this bowel perimeter can be determined for tumors in the paraspinal location.
Percutaneous CT or ultrasound-guided biopsy are most often unnecessary except for an unresectable tumor, or if the clinical presentation or CT scan findings do not support the diagnosis of a retroperitoneal sarcoma.
Recommendation
A CT scan of the chest, abdomen, and pelvis is recommended.
Case Continued
The patient undergoes a CT scan of the abdomen and pelvis. Prior to referral, a CT-guided biopsy requested by the primary physician establishes a diagnosis of a high-grade liposarcoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree