Case 59
Presentation
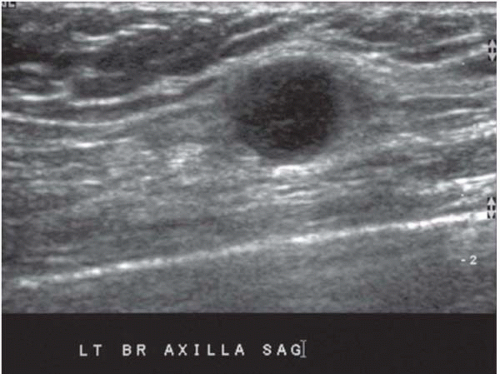
A 39-year-old woman with a family history of breast cancer presents to your office with pain in the left arm after physical activity and a tender nodule in her left axilla of 10 days’ duration. Her family history is positive for breast cancer with her mother and a paternal aunt diagnosed at a postmenopausal age. There is no family history of ovarian cancer. On examination, two left axillary masses, one measuring 1 cm and the other high in the axilla measuring 2.5 cm, are palpated. There are no breast abnormalities. Prior to her presenting to your office, she had undergone a bilateral diagnostic mammogram, an ultrasound of the left axilla, a core biopsy of the axillary mass, and a metastatic workup. Bilateral mammogram showed dense breast parenchyma with no mammographic evidence of malignancy and the ultrasound findings are shown below.
▪ Ultrasound
Ultrasonography Report
Ultrasound of the left axilla reveals two lesions in the axilla: a 3.3-cm ovoid hypoechoic lesion, highly vascular and with a shallow fatty cleft, and an additional adjacent 1.3-cm hypoechoic lesion. Both lesions are interpreted as lymph nodes. The impression is that these lymph nodes are most consistent with reactive adenopathy; however, malignancy cannot be excluded.
Case Continued
Biopsy of the lymph node revealed metastatic adenocarcinoma.
Differential Diagnosis
The most likely primary tumor site for metastatic adenocarcinoma to the axilla in a woman is the breast. Other potential primary tumor sites include the gastrointestinal and genital tracts and, in a smoker, the lung. A metastatic workup targeting these areas should be based on clinical findings. Serum tumor markers may be helpful in elucidating the primary tumor site.
Discussion
Occult breast cancer presenting with axillary adenopathy is infrequent and constitutes 1% of all breast cancers. In the woman presenting with axillary metastasis from an adenocarcinoma, the most likely primary site is the breast. The breasts should be evaluated by mammography as the initial diagnostic test. Other imaging modalities, such as ultrasound and magnetic resonance imaging (MRI), are also potentially useful for finding the primary breast lesion. MRI with a dedicated breast coil can identify the primary breast cancer in 75% to 80% of patients presenting with axillary adenopathy without mammographic findings, and is most useful in the patient with dense breast parenchyma. Ultrasound can also be helpful in identifying the primary breast tumor; like MRI, it is most useful in patients with dense breast parenchyma. However, breast ultrasound can be operator dependent. If a primary tumor cannot be identified in the breast,
then an appropriate metastatic workup can be performed to identify the primary lesion and may include a colonoscopy, gastroscopy, and computed tomography (CT) scans of the chest, abdomen, and pelvis.
then an appropriate metastatic workup can be performed to identify the primary lesion and may include a colonoscopy, gastroscopy, and computed tomography (CT) scans of the chest, abdomen, and pelvis.
Tissue to document the etiology of the adenopathy can be obtained easily with fine-needle aspiration cytology (FNAC) or core needle biopsy. FNAC is the easier technique to perform and can be done with or without sonographic guidance. In addition to verifying the presence of metastatic adenocarcinoma, immunohistochemical evaluation of the biopsy specimen for hormone-receptor status or markers associated with certain primary tumor sites may also be requested. Serum tumor markers may be obtained for these patients, but are not sufficiently specific for any particular organ site.
Recommendation
MRI of the breast and whole breast ultrasound.
Case Continued
The breast MRI did not reveal any specific abnormality.
▪ Ultrasonogram
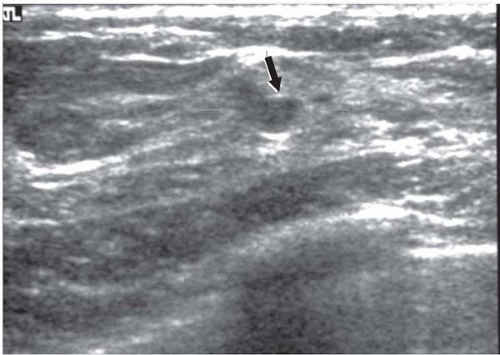 Figure 59.2
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|