Case 55
Presentation
A 36-year-old multiparous Hispanic woman, 20-weeks pregnant, presents in clinic with a complaint of a persistent, tender left breast mass of 3 weeks’ duration. She is otherwise healthy, has no past history of breast problems and no family history of breast or ovarian cancer, and she previously successfully breast-fed her other children. Physical examination discloses a firm but not hard, slightly tender, mostly discrete 2.5 × 2-cm mass beginning 3 cm above the areolar margin without any overlying skin changes. The patient came with a recent bilateral mammogram, which showed only dense breast tissue without any obvious abnormalities, read as BIRADS 1. A targeted left breast ultrasound is obtained.
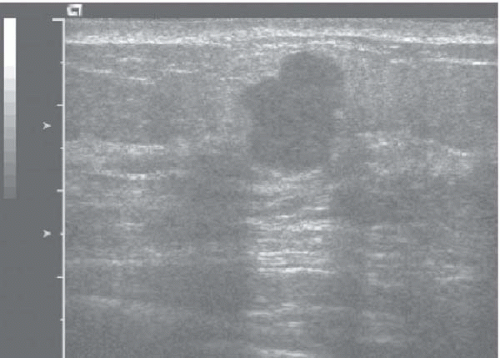
▪ Breast Ultrasonogram
Breast Ultrasonography Report
Ultrasound of the left breast reveals an 11 × 12 × 14-mm macrolobulated hypoechoic mass, taller than wide, with good through transmission but some increased blood flow at the edges, read as BIRADS 4.
Discussion
Mammography is both safe and useful in the evaluation of the breast in pregnant women. The radiation dose to the properly shielded fetus is only 0.01 rad, well below the accepted 5-rad limit. However, owing to the increased density of breast tissue in younger and pregnant women, mammography has a high false-negative rate in these settings, with reported sensitivities of only 64% or less in pregnant women. Conversely, ultrasound is 93% accurate for the evaluation of masses in pregnant women, and should be used in most cases, especially when the mammogram is normal during the evaluation of a suspicious mass. The safety of magnetic resonance imaging (MRI) of the breast is still being established in pregnant women; some radiologists recommend it not be used in the first trimester, but there are no consistent data for this.
Differential Diagnosis
The differential diagnosis includes cancer, fibroadenoma, lobular hyperplasia, lipoma, and (rarely) leukemia, lymphoma, sarcoma, neuroma, and tuberculosis. A cyst, including galactocele, seems less likely given the ultrasound result. Because the mass has persisted longer than 2 weeks, it requires further evaluation by completion of a modified triple test (addition of a needle biopsy to the clinical breast examination and ultrasound).
Case Continued
Fine-needle aspiration done in the clinic immediately following the ultrasound shows malignant cells (modified triple test score of 7). Alkaline phosphatase level is elevated, but a chest x-ray and
low-dose bone scan are normal. A subsequent core biopsy shows a high-grade invasive ductal cancer, estrogen-receptor and progesterone-receptor positive, and HER-2/neu negative.
low-dose bone scan are normal. A subsequent core biopsy shows a high-grade invasive ductal cancer, estrogen-receptor and progesterone-receptor positive, and HER-2/neu negative.
Discussion
Because of the tendency for delayed diagnosis of pregnancy-associated breast cancer, a high index of suspicion and an easy, rapid, “one-stop” method of evaluating suspicious masses in the pregnant patient are required. The modified triple test (MTT) is accurate (scores of 6 or more indicate cancer) and allows the clinician to move ahead quickly with a metastatic workup and treatment planning. Malignancies diagnosed by fine-needle aspiration as part of the MTT should be confirmed by core needle biopsy (which caries a small risk of milk fistula in lactating patients) or intraoperative frozen section.
As in nonpregnant patients, a primary metastatic workup (chest x-ray, alkaline phosphatase, and liver function tests) is usually sufficient for early stage breast cancer (stages I and IIA). Chest x-rays are safe throughout pregnancy, but alkaline phosphatase levels may be falsely elevated, so that a low-dose bone scan may be needed. Low-dose bone scans reduce the fetal radiation exposure by half (from 0.19 to 0.08 rad). For higher stage or symptomatic patients, MRI of the liver and/or brain should be added to the workup; MRI is superior to ultrasound for evaluation of the liver in pregnant patients. Gadolinium crosses the placenta and is a class C drug in pregnancy, meaning that it can potentially cause fetal abnormalities, and should be used only if the benefit justifies risk.
Diagnosis and Recommendation
Pregnancy-associated invasive breast cancer. Because this patient was already in her second trimester and was likely to be a candidate for chemotherapy, she is offered either mastectomy or lumpectomy and radiation. She chose the latter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree