Case 54
Presentation
A 52-year-old woman presents for routine follow-up 3 years after right breast-conserving surgery and radiation therapy for a 2.5-cm invasive ductal carcinoma. Original pathology included an intermediate-grade tumor, all surgical margins were clear, estrogen and progesterone receptors were positive, and all lymph nodes were negative for metastatic disease.
▪ Clinical Photograph
Physical Examination Report
Physical examination reveals mild thickening of the breast and slight retraction in the area of wide local excision. There is no palpable mass. There is no lymphadenopathy in the axilla or supraclavicular area, and no other concerning features are found on physical examination. A diagnostic mammogram is obtained.
Differential Diagnosis
In general, mild thickening without a mass may be related to initial surgery and radiation therapy. Also,
scar tissue and radiation-associated fibrosis may present as mass-like regions that are difficult to distinguish from local recurrence. Fat necrosis from surgical trauma may present as a hard mass with skin dimpling and may occur under flaps following mastectomy and reconstruction. Changes in the physical examination occurring 1 to 2 years after initial surgical and radiation therapy must be viewed with suspicion.
scar tissue and radiation-associated fibrosis may present as mass-like regions that are difficult to distinguish from local recurrence. Fat necrosis from surgical trauma may present as a hard mass with skin dimpling and may occur under flaps following mastectomy and reconstruction. Changes in the physical examination occurring 1 to 2 years after initial surgical and radiation therapy must be viewed with suspicion.
Local recurrence, defined as any recurrence of cancer in the ipsilateral breast, chest wall, or skin, may present with minimal thickening or retraction at the site of prior surgery. Local recurrence should be distinguished from regional recurrence (i.e., axillary, internal mammary, or supraclavicular lymphadenopathy). Approximately one third of recurrent breast cancers are diagnosed by mammography alone. Physical examination may detect a suspicious mass, asymptomatic nodule, skin dimpling, or retraction, similar to the presentation of primary breast cancer in approximately two thirds of patients. Less commonly, diffuse breast thickening and increasing induration may be indicative of local recurrence and is easily confused with radiation-induced changes. Rarely, local recurrence may present as an area of nipple excoriation or Paget disease.
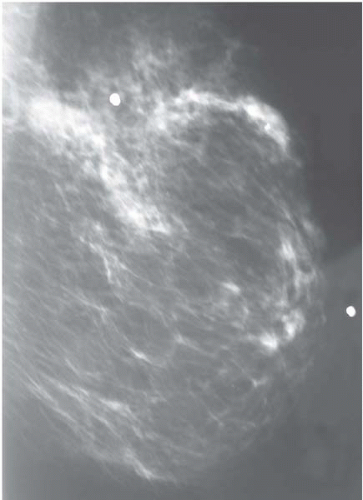
Mammography may note features similar to the original primary tumor including irregular or clustered microcalcifications, a spiculated mass, increased density, or distorted architecture. Fat necrosis and scarring may mimic a primary or recurrent breast cancer. Rarely, areas of well-circumscribed sclerosis can occur following radiation therapy. Certain histologies, such as infiltrative lobular breast cancer, can be mammographically occult.
Discussion
Because it is often difficult to interpret the physical examination and mammogram, suspicious findings should be histologically evaluated. Fine-needle aspiration and core biopsies have up to a 15% false-negative rate in this setting. Mammography-guided or ultrasound-guided and mammotome biopsies produce more accurate and larger specimens, respectively. However, it still may be difficult to distinguish radiation-induced atypia from malignancy. An open surgical biopsy may be required. An expert breast pathologist is very helpful in equivocal tissue diagnoses.
The National Cancer Institute (NCI) randomized control trial (RCT) comparing breast-conserving surgery (BCS) with mastectomy noted a 22% risk of local recurrence following BCS, axillary dissection, and adjuvant radiation therapy at a median follow-up of 18 years. Most patients with local recurrence were salvaged by mastectomy, and disease-free and overall survival were comparable in the two groups. The National Surgical Adjuvant Breast Project (NSABP) B-06 trial comparing modified radical mastectomy, lumpectomy, and lumpectomy plus radiation for breast cancer (4 cm or less) noted a 14.3% local recurrence rate following BCS and radiation at 20 years of follow-up. Local recurrence occurred in 39.2% of patients treated by lumpectomy alone. A similarly designed RCT from Europe in early-stage breast cancer (2 cm or less) noted an 8.8% local recurrence rate at 20 years following BCS and adjuvant radiation.
An overview of these RCTs confirms the risk of local recurrence is three times lower when radiation therapy is utilized in addition to BCS. Although radiotherapy is associated with a slightly lower breast cancer-specific death rate, overall survival is unchanged when comparing surgery with surgery plus radiation therapy.
Risk factors for local recurrence in various studies include multicentricity, increasing primary tumor size and grade, close or positive margins, an extensive intraductal carcinoma component, vascular or lymphatic invasion, increasing number of metastatic axillary lymph nodes, hormone receptor-negative tumors, younger patients (<45 years of age), and absence of adjuvant radiation therapy.
Case Continued
Mammogram-guided core biopsy confirms invasive breast cancer. Histology is the same as the primary breast cancer.
Diagnosis and Recommendation
Recurrent breast carcinoma. The patient should be restaged, which includes history and physical examination, chest x-ray, liver imaging, ultrasonography, and bone scan. There is no evidence of metastatic disease.
▪ Approach
Staging tests, including chest x-ray, liver ultrasound, and bone scan, have a low yield in stage I and II primary breast cancer. However, full staging is generally warranted in patients with locally recurrent breast cancer following BCS even though most will not have clinically detectable distant metastases at the time of diagnosis.
Locally recurrent breast cancer may have a devastating psychological impact. The recurrence is a visible reminder of failure to respond to therapy and has significant implications for prognosis. A holistic
approach is paramount. It is important to inform the patient adequately regarding optimal treatment and prognosis but also to maintain hope.
approach is paramount. It is important to inform the patient adequately regarding optimal treatment and prognosis but also to maintain hope.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree