Case 50
Presentation
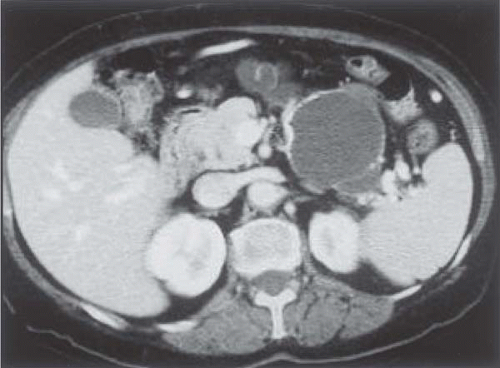
A 63-year-old woman with a past medical history significant for type 2 diabetes mellitus, cerebrovascular disease, hypertension, psoriasis, hysterectomy with oophorectomy (for uterine fibroids), and alcohol abuse presents to your office after she was seen by her primary medical doctor 1 month previously with right upper quadrant tenderness secondary to trauma. She denies any prior gastrointestinal or constitutional symptoms such as abdominal pain, nausea, vomiting, early satiety, diarrhea, constipation, anorexia, or weight loss. On abdominal examination, no organomegaly, masses, tenderness, or ascites are noted. Previous abdominal ultrasound shows a 5.5-cm cystic mass in the tail of the pancreas.
Differential Diagnosis
The differential diagnosis of a patient with a cystic pancreatic lesion includes pseudocyst, serous cystadenoma, mucinous cystic neoplasm, intraductal papillary mucinous neoplasm, cystic islet cell tumor, solid and cystic papillary (Hamoudi) tumor, and mucinous cystadenocarcinoma.
Discussion
Cystic pancreatic neoplasms are rare and account for only 1% of primary pancreatic malignancies and 50% to 60% of cystic lesions of the pancreas. The most common cystic lesions of the pancreas are pseudocysts, which usually are the result of gallstone-induced or alcohol-induced pancreatitis or trauma. Cystic pancreatic neoplasms occur at a median age of 50 to 60 years and with a female:male predominance of 9:1. Symptoms commonly encountered are vague, nonspecific abdominal pain, early satiety, nausea, and vomiting. In many patients no symptoms are evident, and lesions are initially identified as an incidental finding, as in the case being presented.
In the absence of pancreatitis, which otherwise might suggest a pseudocyst, benign lesions include serous cystadenoma and solid and cystic papillary (Hamoudi) tumors. Mucinous cystic neoplasms, intraductal papillary mucinous neoplasms, and cystic islet cell tumors are premalignant or malignant, whereas mucinous cystadenocarcinomas are malignant. A recent analysis from our institution (Medical College of Wisconsin) has shown that symptoms and age are predictors of neoplasia. The absence of gallstones on ultrasound, no prior history of alcoholic pancreatitis, and the calcifications make a pseudocyst unlikely. Although this patient is asymptomatic, her age (63 years) raises concerns about a premalignant or malignant cystic tumor.
Recommendation
Endoscopic ultrasound (EUS) with fine-needle aspiration is recommended for this patient.
Case Continued
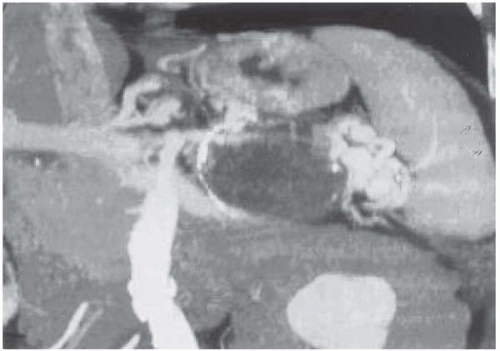
Possible further workup could include EUS with fine-needle aspiration (FNA), which may yield further information not only about the type of cyst, but also about the relationship of the pancreatic duct to the cystic lesion. In this patient, EUS shows a complex cystic mass in the tail of the pancreas with multiple irregular septations. The rest of the pancreas is sonographically normal with no pancreatic duct dilatation. FNA shows hypocellular smears with
monolayered groups of benign duct epithelium, rare histiocytes, and mucus/debris consistent with a mucinous cystic neoplasm.
monolayered groups of benign duct epithelium, rare histiocytes, and mucus/debris consistent with a mucinous cystic neoplasm.
Discussion
Noninvasive imaging techniques such as CT and magnetic resonance imaging (MRI) are unreliable to accurately distinguish among the different pancreatic cysts. As a result, many authorities recommend surgical removal, especially in patients who are younger and otherwise fit. Others have recommended percutaneous aspiration with fluid analysis. More recently, EUS with FNA has been suggested as a method to differentiate among benign, premalignant, and malignant lesions. However, percutaneous or endoscopic aspiration has the potential to spill malignant cells into the peritoneum with subsequent seeding and reduced survival. For this reason, as well as concerns about diagnostic accuracy, we do not recommend preoperative aspiration. Nevertheless, EUS was performed prior to referral in this patient. Endoscopic retrograde cholangiopancreatography (ERCP) and magnetic resonance cholangiopancreatography (MRCP) may be helpful in defining cyst and pancreatic duct anatomy. However, CT pancreatography and intraoperative ultrasound may be just as useful, less invasive, and potentially less expensive than ERCP.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree