Case 49
Presentation
A 67-year-old woman with no relevant past history has experienced vague epigastric discomfort and anorexia for the last several weeks. She now presents with jaundice, acholic stools, and dark urine. A 15-pound weight loss is documented. Physical examination shows scleral icterus. There is no palpable abdominal mass or evidence of ascites. Total bilirubin is elevated at 9 mg/dL.
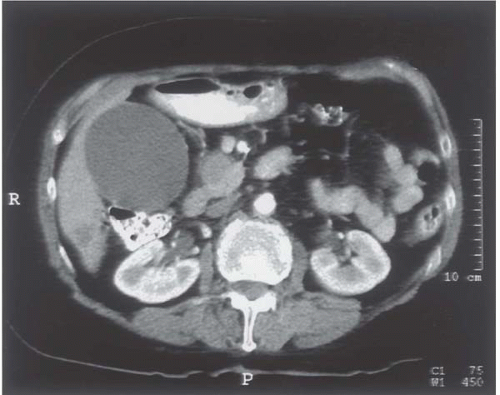
▪ Abdominal X-Ray
Abdominal X-Ray Report
The gallbladder is markedly dilated, representing distal bile duct obstruction. A 3-cm mass is seen in the head of the pancreas. There is no evidence of liver metastases, and the major visceral vessels (superior mesenteric vein, portal vein, superior mesenteric artery, and hepatic artery) are not involved.
Differential Diagnosis
The diagnosis for obstructive jaundice (as diagnosed by the obstructed biliary tree on computed tomography [CT]) includes periampullary cancer (pancreatic, distal bile duct, ampullary, or duodenal carcinoma), common bile duct stone, and benign distal bile duct
stricture, usually due to chronic pancreatitis. Other pancreatic neoplasms, such as cystic neoplasms or islet cell tumors, may also uncommonly present with jaundice. The clinical scenario presented is classic for cancer of the head of the pancreas.
stricture, usually due to chronic pancreatitis. Other pancreatic neoplasms, such as cystic neoplasms or islet cell tumors, may also uncommonly present with jaundice. The clinical scenario presented is classic for cancer of the head of the pancreas.
Discussion
The extent of further workup necessary at this time is variable. Many surgeons would proceed with an operation to potentially resect the tumor without further evaluation, based on a high-quality contrast-enhanced spiral CT scan. Endoscopic retrograde cholangiopan-creaticography (ERCP) with or without endostent placement may be advisable if the level of jaundice is high or if a delay in definitive surgery is anticipated. Endoscopic ultrasound can be used to further assess the local extent of disease (vascular invasion, lymph node involvement) and can successfully obtain a cytologic diagnosis by fine-needle aspiration in a high percentage of patients. A preoperative tissue diagnosis is not required prior to surgery, although it can be useful, especially if neoadjuvant chemoradiation is planned. Finally, many surgeons will perform a prelaparotomy diagnostic laparoscopy because of a 10% to 15% incidence of detecting unsuspected small liver or peritoneal metastases.
Diagnosis and Recommendation
This patient has potentially resectable pancreatic carcinoma. She should undergo appropriate preoperative medical evaluation in preparation for pancreaticoduodenectomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree