Case 48
Presentation
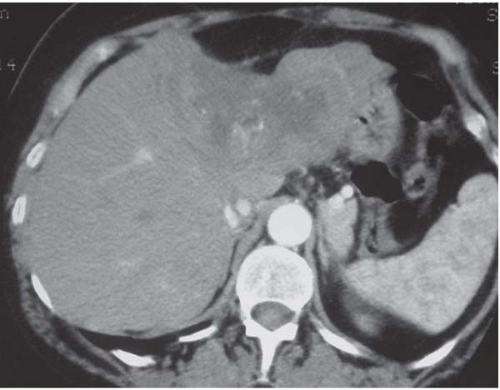
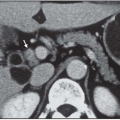
The patient is a 60-year-old white woman who presents with abdominal pain. The computed tomography (CT) scan shows a tumor of the anatomical left lobe that extends to segment IV. The left branch of the portal vein is not seen and the right branch of the portal vein is well visualized, suggesting an arteriovenous fistula. There are no retroperitoneal or intraperitoneal lymph nodes, with no evidence of a gastric or colonic primary tumor. Serum transaminases and gamma glutamyl transpeptidase are normal. The other liver tests are normal. Percutaneous transhepatic biopsy reveals a strongly mucosecretory adenocarcinoma of the liver.
Differential Diagnosis
Case Continued
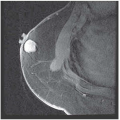
Immunohistochemistry is in favor of intrahepatic cholangiocarcinoma, because of positive cytokeratin 7 and negative cytokeratin 20 and carcinoembryonic antigen (CEA).
Diagnosis and Recommendation
The diagnosis is intrahepatic cholangiocarcinoma. The patient has no major comorbid conditions and therefore is judged to be suitable for surgery.
▪ Approach
Cholangiocarcinoma is known to have a poor prognosis. Though some may treat these tumors with chemotherapy alone, the mainstay of ensuring cure is surgical resection. In high-risk patients, such as those with large tumors, consideration can be given to treating the patient initially with neoadjuvant chemotherapy.
Case Continued
The patient received preoperative chemotherapy with six cycles of 5-fluorouracil (5-FU) and cisplatin with good tolerance.
▪ CT Scan
CT Scan Report
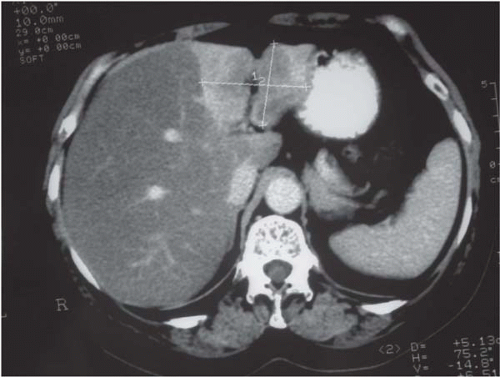
The postchemotherapy CT scan performed showed tumor regression. The tumor measures 8 × 6 cm; by comparison, on the previous scan it measured 12 × 7 cm. Liver retraction in front of the tumor is noted, a good sign of downstaging. The right liver is hypotrophic with the same steatosis as on the left, probably related to chemotherapy.
▪ Surgical Approach
The abdomen is explored through a bilateral subcostal incision, and careful exploration is performed to
exclude peritoneal and lymph node metastases. The extent of the tumor is assessed by palpation and confirmed with intraoperative liver ultrasonography. The lesser omentum is opened and a vessel loop is placed around the porta hepatis in preparation for a subsequent Pringle maneuver. The liver is mobilized by division of the falciform and the left triangular ligament while avoiding injury to the phrenic vein. The confluence of the middle and left hepatic vein with the suprahepatic vena cava is exposed, and a vessel loop is secured around the left hepatic vein. The portal triad is clamped and a hepatotomy is made at the hilum in segment IV and caudate lobe, allowing isolation of the left hepatic pedicle, which is transected with a linear stapler. The liver parenchyma is transected and the left hepatic vein is divided when encountered.
exclude peritoneal and lymph node metastases. The extent of the tumor is assessed by palpation and confirmed with intraoperative liver ultrasonography. The lesser omentum is opened and a vessel loop is placed around the porta hepatis in preparation for a subsequent Pringle maneuver. The liver is mobilized by division of the falciform and the left triangular ligament while avoiding injury to the phrenic vein. The confluence of the middle and left hepatic vein with the suprahepatic vena cava is exposed, and a vessel loop is secured around the left hepatic vein. The portal triad is clamped and a hepatotomy is made at the hilum in segment IV and caudate lobe, allowing isolation of the left hepatic pedicle, which is transected with a linear stapler. The liver parenchyma is transected and the left hepatic vein is divided when encountered.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree