Case 38
Presentation
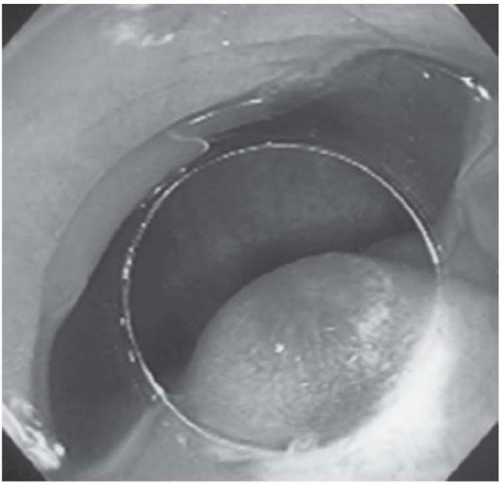
A 57-year-old man who has a past medical history of hypertension and hyperlipidemia presents to your office after he was seen by his primary medical doctor for symptoms of occasional anal bleeding and changes in defecation. He is a nonsmoker and has no constipation. On physical examination, there is neither ascites nor a palpable abdominal tumor. On digital rectal examination, a 5-cm firm tumor is palpable on the left side of the rectal wall and 3 cm from the anal verge. The tumor is not movable and appears to be covered by the intact mucosa. No apparent bleeding is noted.
Differential Diagnosis
The differential diagnosis for rectal submucosal masses in the adult include: mesenchymal tumors, lymphomas, submucosal extension of rectal and/or anal carcinomas, melanomas, and genitourological tumors. Mesenchymal cell tumors are mainly composed of gastrointestinal stromal tumor (GISTs), leiomyomas, and leiomyosarcomas. Submucosal extension of rectal or anal carcinoma is relatively frequent in the poorly differentiated type of rectal adenocarcinoma or anal squamous cell carcinoma, respectively, and sometimes accompanies an increase
in tumor markers, including carcinoembryonic antigen (CEA), cancer antigen (CA) 19-9, and squamous cell cancer (SCC). In this patient, CEA, CA 19-9, and SCC levels are within the normal range. Based on the location of the tumor, and with no increase in CEA and SCC, one must consider stromal tumor in the rectum to be the primary diagnosis. In radiographic evaluation of a pelvic mass, magnetic resonance imaging (MRI) is superior to computed tomography (CT) scan in discrimination of each structure. The biopsy of the rectal tumor is usually not difficult. Histologic examination is the most reliable test for submucosal tumors.
in tumor markers, including carcinoembryonic antigen (CEA), cancer antigen (CA) 19-9, and squamous cell cancer (SCC). In this patient, CEA, CA 19-9, and SCC levels are within the normal range. Based on the location of the tumor, and with no increase in CEA and SCC, one must consider stromal tumor in the rectum to be the primary diagnosis. In radiographic evaluation of a pelvic mass, magnetic resonance imaging (MRI) is superior to computed tomography (CT) scan in discrimination of each structure. The biopsy of the rectal tumor is usually not difficult. Histologic examination is the most reliable test for submucosal tumors.
Recommendation
CT scan of the pelvic region as well as a fine-needle biopsy.
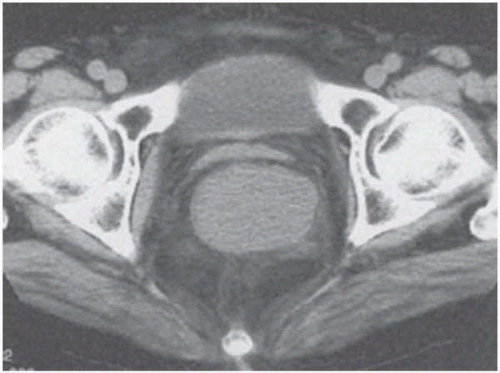
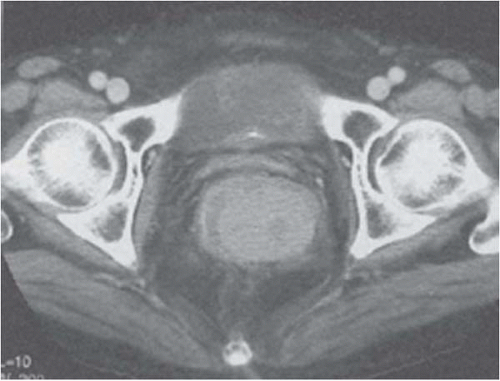
▪ CT Scan
CT Scan
A 5-cm, round, homogenously slightly enhancing mass with clear margin located on the left wall of the rectum. The tumor does not involve the bladder or prostatic gland.
Histopathology Report
Biopsy specimen reveals an epithelioid and spindle cell-type tumor with a few mitoses.
▪ Approach
Stromal tumors of the rectum are usually either GIST or leiomyosarcoma. The patient is offered an abdominoperineal resection (APR) of the rectum. In some cases, local excision or sphincter-sparing operations, including lower anterior resection (LAR), may be recommended if the tumor has adequate distance from the anal sphincter muscles. In this case, the lower border of the tumor is located just above the sphincter muscles. Complete resection by APR is expected in more than 90% of cases; after complete resection, there is an estimated 30% to 40% incidence of local recurrence or hepatic metastasis. The possibility of bladder and sexual dysfunction after APR is relatively less frequent than when performed for rectal or anal carcinoma because no lymph node dissection is required for a stromal tumor and the pelvic nerve plexus innervating to the bladder and penis can be preserved.
▪ Surgical Approach
It is critical to perform a complete tumor resection with a 1- to 2-cm margin. A lower abdominal incision is performed for mobilization of the rectum and preparation of the sigmoid colon for colostomy. Laparoscopic-assisted abdominal procedures may also substitute for an open laparotomy. A synchronous perineal incision and dissection is performed for en bloc resection of the anorectum. A single closed drain is placed in the pelvic cavity at the end of the operation; the drain is usually removed on the second or third postoperative day.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree