Case 36
Presentation
The patient is a 38-year-old man who initially presented 8 years previously with rectal bleeding. He had a strong family history of colon cancer: both his paternal aunt and his paternal uncle had died of colon cancer, and his father had known colonic polyps. Physical examination was unremarkable. Colonoscopic evaluation revealed a sessile polyp at 15 cm; biopsies confirmed moderately to poorly differentiated adenocarcinoma. The patient underwent low anterior resection followed by adjuvant chemoradiation. Pathologic examination revealed one of six pericolonic nodes positive for adenocarcinoma (pathologic stage III; T3, N1, M0).
The patient did well for 7 years postoperatively, and then returned to his oncologist with a 6-month history of chronic sacral discomfort and sciatica-like pain in the left lower extremity. He denies any history of trauma to the back or lower extremities.
Differential Diagnosis
The differential diagnosis for sciatica includes spinal stenosis, herniated disc, cauda equina syndrome, and traumatic injury to the spine. Given the patient’s history of rectal cancer, recurrent rectal cancer (specifically, tumor involving the sacrum) must be foremost on the list of differential diagnoses. This suspicion is corroborated by the newly elevated carcinoembryonic antigen (CEA) level.
Case Continued
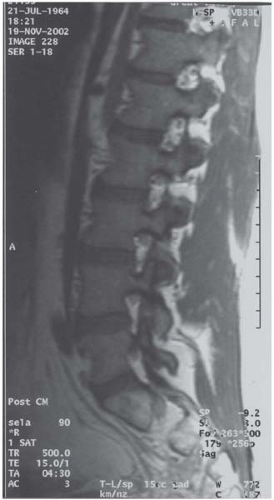
Physical examination reveals a robust young man. Abdominal examination is unremarkable except for a well-healed midline incision, and examination of the back and lower extremities is normal. The CEA level is 10.2 ng/mL (normal: <2.5 ng/mL). After treatment of his rectal cancer 7 years previously, the patient’s CEA level had been 1.3 ng/mL. Magnetic resonance imaging (MRI) of the lumbar spine and left hip are normal. Bone scan further confirms abnormal uptake in the area overlying the sacrum. Colonoscopy confirms an anastomotic recurrence at 15 cm; pathologic examination reveals moderately to poorly differentiated adenocarcinoma. In the interim, the patient’s CEA level has risen to 12.0 ng/mL.
Computed tomography (CT) scan of the abdomen and pelvis reveals a slight increase in soft tissue density in the retrorectal area, with loss of the normal fat plane between the rectum and the sacrum. There is no evidence of hepatic metastases or retroperitoneal/mesenteric adenopathy. On positron emission tomography (PET), there is a large area of intense, irregular 18F-labeled fluorodeoxyglucose uptake in the presacral area, correlating with the abnormal area on CT.
Diagnosis and Recommendation
A young, healthy man with locally advanced, recurrent rectal cancer. The patient’s performance status and general medical condition are excellent. There is no evidence of systemic metastatic disease.
Optimal treatment of locally recurrent rectal cancer is surgical resection. Imaging studies to fully assess the extent of local disease and to rule out metastatic disease should be performed prior to surgical intervention.
▪ Approach
Complete surgical resection, if possible, offers the best chance of long-term cure of recurrent rectal cancer. Resection will involve total pelvic exenteration with en bloc resection of the tumor and involved sacrum (abdominosacral resection, or ASR).
Case Continued
The patient is treated with a neoadjuvant chemotherapy regimen (5-fluorouracil, leucovorin, and irinotecan) to induce potential tumor shrinkage. He had received the maximum tolerable dose of external beam radiation therapy (EBRT) after his original low anterior resection; thus, further EBRT at this point is not a viable alternative.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree