Case 29
Presentation
An 80-year-old woman presents to your office with a 4-month history of change in bowel habit: dark red blood per rectum following defecation. On several occasions, the patient noticed that the blood was mixed with the stool and was associated with mucus discharge. She has no tenesmus, fecal urgency, or weight loss, and no family history of colon cancer. She suffers from hypertension and is taking an oral anticoagulant for atrial fibrillation. On examination the abdomen is soft with no palpable masses. Rectal examination is unremarkable, rigid sigmoidoscopy shows normal rectal mucosa, and anoscopy reveals small first-degree hemorrhoids.
Differential Diagnosis
The differential diagnosis for bleeding per rectum in an adult includes hemorrhoidal disease, fissure-inano, inflammatory bowel disease, rectal or colonic polyp, large bowel malignancy, diverticular disease, and colonic angiodysplasia. In this patient, with symptoms of mixed altered blood and mucus per rectum, one must exclude colorectal malignancy and benign polyps.
Case Continued
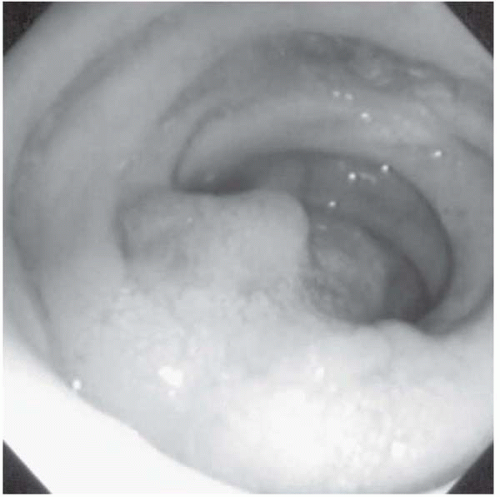
Following full bowel preparation and cessation of the oral anticoagulant 3 days prior to the procedure, an outpatient colonoscopy is performed. Good views are obtained to the cecum, which was identified by the presence of the ileocecal valve.
Case Continued
Using submucosal infiltration with India ink, the polyp base is elevated off the muscularis propria and snared in three pieces. The two additional polyps, measuring 4 mm each, in the proximal sigmoid colon are snared and retrieved.
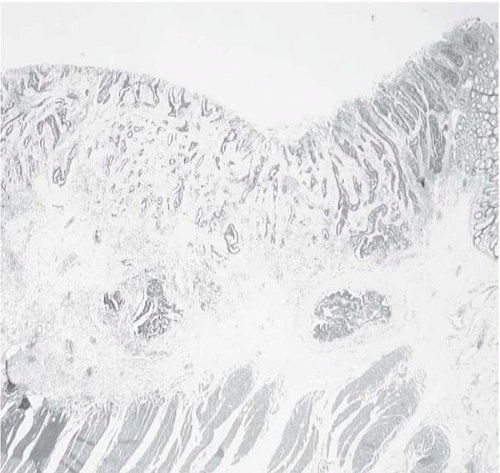
Histologic examination of the two smaller polyps reveals moderately dysplastic tubular adenomas. The larger lesion is a tubulovillous adenoma with a focus of moderately differentiated adenocarcinoma infiltrating into the submucosa, reaching within 1 mm of the deep resection margin. There is no evidence of lymphovascular or perineural invasion.
Recommendation
To determine disease stage, obtain a chest x-ray and computed tomography (CT) scans of the abdomen and pelvis. If the chest x-ray shows any abnormality, then further evaluation can be performed with CT scan of the chest.
Case Continued
In this patient, CT scans of the chest, abdomen, and pelvis are obtained to exclude evidence of metastatic disease. There was a small area of scarring in the left lung, the liver was normal, and there was no evidence of abdominal or pelvic lymphadenopathy.
▪ Approach
The risk of death, based on the patient’s comorbidity, for oncologic bowel resection is estimated to be on the order of 5%. The risk of lymph node metastases is calculated to be 7.2% based on the St. Mark’s Lymph Node Positivity model. The risk of residual tumor is thought to outweigh the risk of surgery, and the decision for open radical resection is made. Radiation therapy has no place in the treatment of early malignant colonic polyps, and the role of chemotherapy as an adjuvant treatment for endoscopically resected colonic polyps is doubtful. In patients with carcinoma near the margins, follow-up endoscopic examination every 6 months is necessary for at least 5 years.
▪ Surgical Approach
It is critical that the tumor is completely removed together with the regional lymph nodes up to the root of the inferior mesenteric artery. Under a general anesthetic, the patient is placed in the Lloyd Davies position to allow the distal rectum to be washed out prior to the anastomosis. The abdomen is entered through a lower midline incision and a complete exploration is performed to exclude liver metastases and locally advanced disease. The sigmoid, descending colon, and splenic flexure are mobilized along the “white line” of Toldt, in the plane anterior to the gonadal vessels and left ureter, which are identified and preserved. A sigmoid colectomy is performed by dividing the colon at the rectosigmoid junction and proximally at the level of the descending colon. A stapled end-to-end colorectal anastomosis is performed and tested under water by air insufflation through the rectum.
Case Continued
The patient has an uneventful recovery and is discharged home on the seventh postoperative day.
▪ Histopathology Slide
Histopathology Report
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree