Case 26
Presentation
A 45-year-old white man presents with a 9-month history of central abdominal pain and an abdominal mass that has increased in size gradually over the past month. He denies changes in bowel habits or constitutional symptoms (i.e., weight loss, fatigue, fever, night sweats). On examination, there is an abdominal mass that is somewhat mobile. No generalized lymphadenopathy or testicular mass is felt.
Differential Diagnosis
Based on the clinical findings of a mobile abdominal mass, and with the computed tomography (CT) scan demonstrating a lobulated mass in proximity to the small bowel, this most likely represents a small bowel neoplasm. The abdominal mass is clearly delineated from the retroperitoneal structures; therefore, it is unlikely to be a retroperitoneal sarcoma. Though a large mesenteric cyst may present as a palpable abdominal mass, the solid nature on the CT scan would argue against this diagnosis. Given the clinical presentation and the accompanying imaging findings, a mesenchymal tumor of the small intestine is very likely.
Discussion
Leiomyomas, leiomyosarcomas, and gastrointestinal stromal tumors (GISTs) of the small intestine often enlarge with extraluminal orientation and thus may reach considerable, even palpable, size before causing symptoms. The mean duration of symptoms before diagnosis can be as long as 1 year. Unlike adenocarcinomas, these neoplasms tend to grow extrinsically and obstruct the small intestine late in their course. Obstruction occurs from external compression, and less commonly from circumferential growth, and very rarely from intussusception. A palpable abdominal mass may be evident in up to half of patients. Many of these tumors eventually outgrow their highly vascular blood supply, leading to central necrosis and occasional calcification that would be evident on a CT scan (although this was not present in the patient in this case). Due to their highly vascular nature and large size, ischemia within the tumor and areas of tumor necrosis are common, leading to hemorrhage in two thirds of patients, and intestinal perforation resulting in an acute abdomen in 10% of patients. The hemorrhage can be intra-abdominal, gastrointestinal, or within the tumor, leading to rapid enlargement in size.
Adenocarcinomas (accounting for 30% to 50% of all small bowel cancers) occur more frequently in the duodenum and the proximal jejunum. Adenocarcinomas almost always present with a slowly progressive intestinal obstruction; in contrast to leiomyosarcomas, a palpable mass or perforation is unusual. Primary carcinoid tumors (accounting for approximately 30% of small bowel tumors) are often 1 to 2 cm in size; however, when locally invasive, primary carcinoid tumors metastasize via regional lymph nodes and are often associated with fibrotic reaction that foreshortens the adjacent small bowel mesentery. This may cause kinking of the bowel and obstruction, or intestinal ischemia as a result of encasement of mesentery blood vessels.
Diagnosis and Recommendation
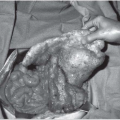
When the clinical features and imaging studies are suggestive of a small bowel GIST, an exploratory laparotomy is required for both diagnosis and treatment. In addition to the CT scan of the abdomen and pelvis, a radiograph or CT scan of the chest is obtained to exclude metastatic disease. Preoperative biopsy is unnecessary because it carries the theoretical risk of peritoneal seeding or tumor rupture; biopsy is indicated only for clearly unresectable disease, or when treatment would be altered (e.g., if the mass proved to be lymphoma or germ cell tumor).
▪ Approach
Surgery is the mainstay of the therapeutic approach to patients with nonmetastatic GISTs. These tumors are resectable in two thirds of cases, on average, but present a high recurrence rate (40% to 90%), an overall survival rate ranging from 28% to 43%, and a median survival time of 50 months. At present, adjuvant radiation therapy has no role, because it does not have any impact on the natural history of these tumors; furthermore, any benefit is outweighed by the toxicity to the intra-abdominal structures. Radiation should be reserved for palliation of pain and bleeding.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree