Case 24
Presentation
A 56-year-old man with no significant past medical history presents to his primary care physician with symptoms of intermittent crampy abdominal pain, nausea, and diarrhea for a few weeks. He denies fever or chills. Physical examination reveals a mildly distended abdomen without any tenderness.
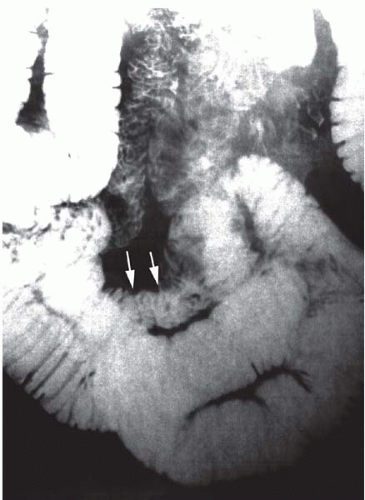
▪ Small Bowel Follow-Through With Barium Contrast
No masses or hernias are palpated. His stool is positive for occult blood. His hematocrit is 25%; other laboratory tests are unremarkable. An abdominal series reveals a mildly dilated stomach without evidence of free intraperitoneal air. Workup, including upper gastrointestinal (GI) endoscopy and colonoscopy, is negative. A small bowel follow-through is obtained.
Small Bowel Follow-Through Report
There is a 3-cm apple-core lesion on the proximal jejunum with high-grade obstruction, suggesting malignancy.
Differential Diagnosis
The differential diagnosis for this patient with a jejunal mass includes benign and malignant tumors of the small intestine, in addition to an inflammatory mass secondary to Crohn’s disease. The most common benign tumors of the small intestine are leiomyomas, adenomas, and lipomas. Malignant tumors of the small bowel include adenocarcinomas, gastrointestinal stromal tumors (GISTs), lymphomas, and carcinoid tumors. In addition, the small intestine is frequently affected by metastases from cancers originating at other sites. Melanoma, in particular, is associated with a propensity for metastasis to the small intestine. The small bowel follow-through suggests this patient has a malignant lesion, although the diagnosis can be confirmed only by pathology.
Discussion
Primary small bowel malignancies are rare, with an estimated incidence of 5,300 cases per year in the United States. They account for only 1% to 2% of all GI tract malignancies. Most small intestinal neoplasms are asymptomatic until they become large. Partial small-bowel obstruction, with associated symptoms of abdominal pain and distention, nausea, and vomiting, is the most common mode of presentation. Obstruction can be the result of
luminal narrowing, the tumor itself, or intussusception, with the tumor serving as the lead point. Bleeding, usually indolent, is the second most common mode of presentation. Physical examination may be unrevealing in the absence of small bowel obstruction. Up to 25% of patients with intestinal cancers are reported to have a palpable abdominal mass. Fecal occult blood tests may be positive. Jaundice secondary to biliary obstruction (in the case of duodenal tumors) or hepatic metastases may be present. Cachexia and ascites may be present with advanced disease.
luminal narrowing, the tumor itself, or intussusception, with the tumor serving as the lead point. Bleeding, usually indolent, is the second most common mode of presentation. Physical examination may be unrevealing in the absence of small bowel obstruction. Up to 25% of patients with intestinal cancers are reported to have a palpable abdominal mass. Fecal occult blood tests may be positive. Jaundice secondary to biliary obstruction (in the case of duodenal tumors) or hepatic metastases may be present. Cachexia and ascites may be present with advanced disease.
Because of the nonspecific symptoms associated with most small intestinal neoplasms, these lesions are rarely diagnosed preoperatively. CT scanning has a low sensitivity for detecting mucosal or intramural lesions in the small intestine, but can demonstrate large tumors and is useful in staging malignancies. Upper GI with small bowel follow-through examinations have reported sensitivities ranging from only 30% to 44% for the detection of small intestinal tumors. Enteroclysis is the test of choice for detecting small intestinal neoplasms, particularly those located in the distal small intestine, with a sensitivity of 90%. Angiography or radioisotope-tagged red blood cell (RBC) scans can be used to localize actively bleeding tumors. Tumors located in the duodenum can be biopsied during esophagogasroduodenoscopy (EGD); lesions located in the distal ileum can sometimes be reached during colonoscopy. Intraoperative enteroscopy can be used to localize tumors beyond the reach of standard endoscopic techniques.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree