Case 18
Presentation
A 58-year-old, slightly overweight man presents to your office after he is seen by his physician with symptoms of dysphagia. He has a 20-year history of gastroesophageal reflux disease (GERD), which was treated with proton-pump inhibitors. The patient reports that he has problems swallowing meats.
Case Continued
The pathology report shows goblet cells as a sign of intestinal metaplasia, that is, Barrett’s esophagus, and cells representing intestinal adenocarcinoma. Adenocarcinoma of the distal esophagus based on Barrett’s metaplasia is diagnosed.
Differential Diagnosis
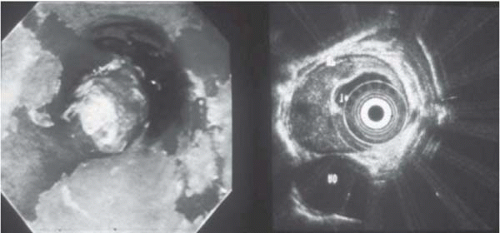
The differential diagnosis for dysphagia should first include malignant tumors of the oropharynx or esophagus followed by other causes such as compression by an enlarged goiter, benign esophageal tumors, achalasia of the esophagus, diverticula of the esophagus, and reflux disease complicated by strictures. If a patient presents with dysphagia, upper gastrointestinal (GI) endoscopy is mandatory
to exclude malignant disease. With the help of endosonography, early forms of tumor growth (i.e., cT1 categories) can be detected, and these patients can be offered endoscopic treatment or a limited surgical resection (see below).
to exclude malignant disease. With the help of endosonography, early forms of tumor growth (i.e., cT1 categories) can be detected, and these patients can be offered endoscopic treatment or a limited surgical resection (see below).
Discussion
The incidence of adenocarcinoma of the esophagus and gastroesophageal junction rose dramatically in the United States and other Western countries over the last decades of the 20th century. The increase has been particularly impressive in white men, in whom the incidence of adenocarcinoma of the esophagus has risen by more than 350% since the mid-1970s. The causes of this startling increase and its pattern are poorly understood, although intense work on risk factors and etiology has yielded some insights.
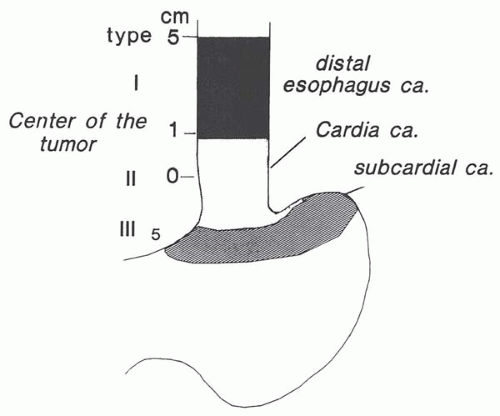
The transitional nature of the anatomic gastroesophageal (GE) junction has added further confusion to the understanding of this disease. Adenocarcinomas of the distal esophagus, GI-junction, and gastric cardia have all increased in incidence, and many studies have grouped tumors at these locations together. A consensus conference of the International Gastric Cancer Association and the International Society of Diseases of the Esophagus in 1998 defined adenocarcinomas of the GE junction as tumors that have their center within 5 cm proximal and distal to the anatomic cardia. Within this area, tumors are differentiated into the following three distinct entities.
Type 1: adenocarcinoma of the distal esophagus usually rising from an area with specialized intestinal metaplasia of the esophagus (Barrett’s esophagus); it may infiltrate the esophagogastric junction from above.
Type 2: True carcinoma of the cardia, arising from the cardiac epithelium or short segments of intestinal metaplasia at the GE junction. This entity is often referred to as “junctional carcinoma.”
Type 3: Subcardial gastric carcinomas that infiltrate the esophagogastric junction and the distal esophagus from below.
This differentiation is especially of importance for surgeons because these types lead to different resection strategies. Type 2 and type 3 tumors can mostly be operated by a transhiatal approach with total gastrectomy and resection of the distal esophagus. Type 1 tumors have to be operated with a thoracoabdominal approach. In these tumors, subtotal esophagectomy is mandatory.
Diagnosis and Recommendation
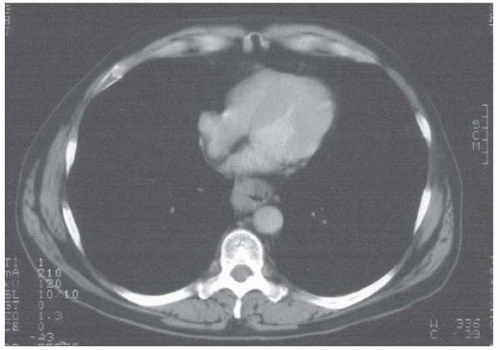
After histologic confirmation of adenocarcinoma of the distal esophagus, staging must be performed to exclude distant metastases. Staging consists of computed tomography (CT) scan of the neck, thorax, and abdomen to reveal lymphatic spread and/or metastatic disease. If distant metastases are found (e.g., liver, bone), surgery is not indicated in
these patients. The treatment for patients with adenocarcinoma of the GE junction is primarily palliative chemotherapy. In patients with severe dysphagia, insertion of a stent is appropriate.
these patients. The treatment for patients with adenocarcinoma of the GE junction is primarily palliative chemotherapy. In patients with severe dysphagia, insertion of a stent is appropriate.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree