Case 13
Presentation
A 45-year-old businessman, who is otherwise healthy, and who is a nonsmoker, presents to his local physician with the complaint of a new mass in his upper thigh. Over the last 6 months, the patient had noted that there was a dull pain in his right medial thigh, and noted a mass that was nontender. Physical examination reveals a 4.5 × 6.0-cm mass in the medial aspect of his right thigh, which moved with the underlying muscle. There was no inguinal adenopathy.
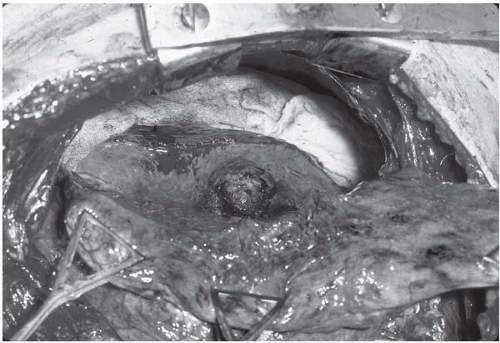
Magnetic resonance imaging (MRI) of the thigh revealed a well-circumscribed mass within the musculature, which is bright on the T2-weighted gadolinium image. The patient is referred to a surgical oncologist who performs a percutaneous core biopsy of the mass. The biopsy reveals a high-grade synovial sarcoma with 2+ necrosis. A computed tomography (CT) scan of the chest is performed, which reveals no nodules. A limb-sparing resection of the mass is performed after preoperative chemotherapy and radiation therapy. The pathology examination reveals 99% necrosis of the mass, and the margins of the resection are free of tumor. The patient had a 3-month period of rehabilitation and then returned to work.
The patient is seen in follow-up by his surgeon and medical oncology team every 3 months after the resection. At each follow-up visit, a CT scan of the chest is performed as well as examination of the primary site. All chest CT scans were free of disease until 18 months after surgery.
Differential Diagnosis
Given the prior history of a stage III high-grade sarcoma, which has an approximately 50% incidence of developing metastases over the next 18 months, the presence of a solitary pulmonary nodule most likely represents metastatic sarcoma. Nevertheless, despite the absence of a history of smoking, the possibility of a new primary lung cancer, such as bronchoalveolar carcinoma, should also be considered. The presence of a benign granuloma is also a possibility, though unlikely, because the previous CT scans were normal.
Discussion
The development of a new pulmonary nodule in a patient with a previous history of a high-grade extremity sarcoma is an ominous sign, and pulmonary metastases must be considered. This patient had never been a smoker, so the possibility of a new lung cancer is remote. Moreover, the appearance of the nodule with smooth edges, nonspiculated, is more compatible with a pulmonary metastasis than a bronchogenic lung cancer. The chance of this new nodule being a metastasis in a sarcoma patient approaches 90%. The time course for the development of pulmonary metastases after successful sarcoma resection is usually within the first 2 years after the management of the primary lesion. Sequential CT scanning at intervals of 3 months for a period of 2 to 3 years is the recommended surveillance for such patients, because it has been shown that CT is much more sensitive in detecting pulmonary metastases than plain chest radiograph. With newer generation CT scanners with multiple detectors, it is possible to detect nodules as small as 2 mm, and performing CT scanning with 5-mm cuts can be a useful test to quantitate the number of nodules bilaterally. It is unnecessary to perform further radiologic workup, except for an evaluation of the primary site, because the natural history of extremity sarcomas is usually metastasis to the lung, as opposed to bone, liver, or brain metastases. The most efficacious manner to evaluate the primary site is with an MRI of the resected bed. This is an important study because the management of the pulmonary metastasis may involve a metastasectomy, and this would be contraindicated if the primary site demonstrated a local recurrence.
Patients with sarcomas are frequently treated with chemotherapies containing doxorubicin, and it has been demonstrated that doses above 400 mg/m2 can be associated with cardiac events, most notably impaired responses to exercise with decreases in ejection fraction. Patients treated with this chemotherapy as part of the regimen should have a stress multiple-gated acquisition (MUGA) scan or equivalent exercise scan to define whether there is any contraindication to thoracotomy.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree