Case 11
Presentation
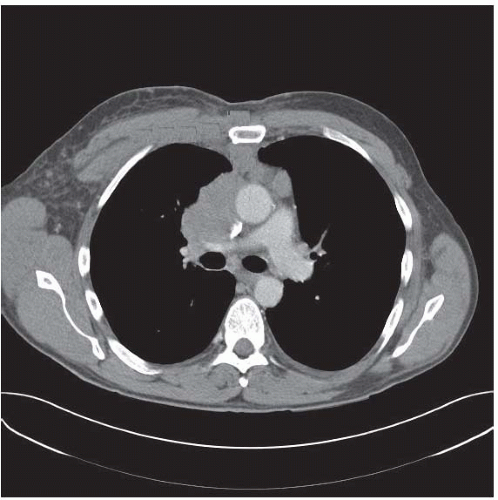
A 51-year-old man with no significant past medical history presents to his primary care physician with a 3-week history of facial swelling, lightheadedness, dizziness, and cough. The symptoms are worse when he is supine. He has only a 5-pack-year smoking history, having quit 15 years prior to presentation. The primary physician orders a computed tomography (CT) scan of the chest, and 1 week later, late on a Friday afternoon, the patient presents for evaluation.
On examination there is significant facial swelling (confirmed by the spouse), supraclavicular fullness, and dilated superficial veins on his anterior chest wall. He relates that he has noted blurring of his vision over the last 3 days and increasing shortness of breath. He can no longer tolerate lying flat. There is no palpable adenopathy and his lungs are clear. He specifically denies fevers, chills, night sweats, and weight loss.
Differential Diagnosis
The differential diagnosis of an anterior mediastinal mass depends somewhat on the age of the patient. In the adult, one must consider thymoma, lymphoma, teratoma, substernal goiter, malignant germ cell tumor, thymic carcinoma, and metastatic disease from a distant primary lesion, such as testicular cancer in men. Metastatic disease from a primary lung cancer does not commonly occur in the anterior mediastinum, but may be seen with small cell lung cancer. In this patient, either invasive thymoma or lymphoma would be the most likely diagnosis with lymphoma occurring more commonly.
Diagnosis
The patient has acute superior vena caval (SVC) syndrome and requires immediate tissue diagnosis followed by the initiation of treatment. Our suspicion is lymphoma, most likely of the non-Hodgkin’s type.
▪ Approach
This patient had not had anything by mouth in the preceding 8 hours, so he was immediately taken to the operating room for an incisional biopsy. With this presentation, and especially with the invasive nature of this lesion, we did not consider an excisional procedure. Because of the SVC syndrome, it is most advantageous to proceed with the diagnostic procedure in an urgent fashion so that definitive treatment may be initiated promptly. With the high likelihood of lymphoma, we felt it was not prudent to attempt needle biopsy because it is critically important to obtain enough tissue to adequately phenotype the lymphoma, which includes flow cytometry.
▪ Surgical Approach
Our intent was to obtain enough material for a definitive diagnosis. This requires the cooperation of
the pathologist, ideally the hematopathologist, who should be present to ascertain whether adequate diagnostic material has been obtained. Even with a large mass, this may sometimes be difficult, especially in the more fibrous lesions where there is very little cellularity. Entering the anterior mediastinum via a parasternal approach allows us to stay extrapleural, that is, out of the pleural space. This is particularly important if the lesion proves to be a thymoma, where pleural spread is known to occur, and thus we avoid violating the pleural space. The bulk of this lesion occurred to the right of the sternum, and therefore we selected a right parasternal approach. Noting the position of the lesion relative to the sternomanubrial joint on the CT scan, we elected to approach the lesion via the third interspace, a procedure known as anterior mediastinotomy (as distinct from median sternotomy).
the pathologist, ideally the hematopathologist, who should be present to ascertain whether adequate diagnostic material has been obtained. Even with a large mass, this may sometimes be difficult, especially in the more fibrous lesions where there is very little cellularity. Entering the anterior mediastinum via a parasternal approach allows us to stay extrapleural, that is, out of the pleural space. This is particularly important if the lesion proves to be a thymoma, where pleural spread is known to occur, and thus we avoid violating the pleural space. The bulk of this lesion occurred to the right of the sternum, and therefore we selected a right parasternal approach. Noting the position of the lesion relative to the sternomanubrial joint on the CT scan, we elected to approach the lesion via the third interspace, a procedure known as anterior mediastinotomy (as distinct from median sternotomy).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree