Case 10
Presentation
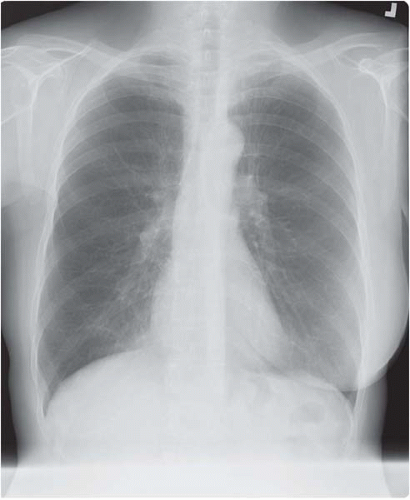
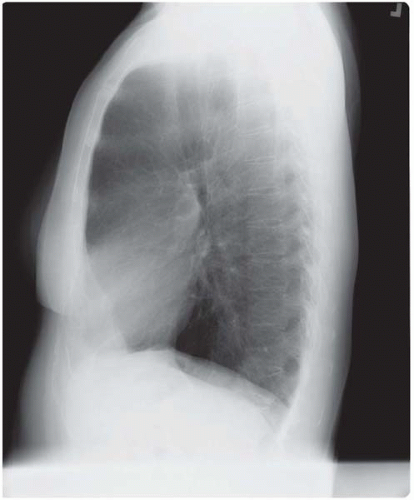
A 56-year-old woman is referred to you with left shoulder pain, which is radiating down her arm, that she has had for the last 6 months. She has been treated by an orthopaedist and a chiropractor without improvement. She works in an office and smoked one to two packs of cigarettes per day until 5 years ago. There is a family history of diabetes, lung cancer, and breast cancer. She has no other symptoms. Physical examination is unremarkable, including range of motion of her left shoulder and chest auscultation. She brings cervical spine films and shoulder radiographs from 5 months ago; they are normal. She also brings chest radiographs from 3 weeks ago.
Differential Diagnosis
This patient has a classic presentation of a Pancoast tumor, with pain radiating down the arm and a subtle, easily missed, abnormality on a chest radiograph. Often, numerous physicians treat patients with such presentations for many months before the possibility of a process arising from the chest is entertained. A Pancoast tumor is a lung cancer arising in the apex of the lung and involving structures of the apical chest wall. Patients may or may not have the classic Pancoast syndrome of pain, weakness, or numbness radiating down the arm as a result of brachial plexus involvement. Horner’s syndrome occurs in approximately 20% of patients with Pancoast tumors (also known as superior sulcus tumors). More than 95% of patients with Pancoast syndrome have non-small cell lung cancer (NSCLC). Less than 5% have small cell lung cancer (SCLC), or even more rarely, another malignancy or an infectious process. Adenocarcinomas account for approximately two thirds of reported cases of Pancoast tumors, and the remaining third are squamous cell with less than 10% large cell carcinomas.
As with all lung cancers, a computed tomography (CT) scan of the chest should be obtained to further characterize the primary lesion, as well as to assess the mediastinum for lymph-node enlargement and the liver and adrenal glands for possible asymptomatic distant metastases. If patient characteristics (risk factors for lung cancer such as smoking and family history), presentation (lack of symptoms suggestive of an infection, hematologic malignancy), and radiographic features (spiculated mass) are all consistent with lung cancer, then there is little question about the diagnosis in patients with a lesion suggestive of a Pancoast tumor. Cytologic confirmation of the diagnosis can be obtained by fine-needle aspiration (FNA) of the mass, which has a diagnostic success rate greater than 90%. Bronchoscopy and sputum cytology are low-yield tests.
Recommendation
CT scan, and FNA of the left apical mass.
Case Continued
A CT scan was normal except for a spiculated left apical mass, confirmed to be an adenocarcinoma by FNA.
Diagnosis
Non-small cell Pancoast tumor with Pancoast syndrome.
Discussion
As with all lung cancers, patients with a Pancoast tumor should first undergo a careful history and physical examination to look for signs of distant metastases. Imaging tests for distant metastases (brain CT, magnetic resonance imaging [MRI], bone scan, or whole-body positron-emission tomography [PET] scan) are not necessary in the presence of a negative clinical evaluation. However, patients should undergo further evaluation of possible mediastinal-node involvement by either mediastinoscopy or PET, even if the CT scan does not demonstrate nodal enlargement. N2 lymph-node involvement is present in approximately 20% of patients with Pancoast tumors, and is a poor prognostic factor. Tumor involvement in enlarged mediastinal or supraclavicular nodes must also be confirmed by cytology or biopsy because of a high false-positive rate.
In patients without mediastinal or distant metastatic disease, MRI should evaluate tumor resectability. This is the best imaging modality to evaluate the extent of tumor involvement of the brachial plexus and bony structures because of the ability to obtain high-quality coronal and sagittal MRI images.
Recommendation
In the absence of distant disease with a normal mediastinum on CT scan of the chest, the patient should undergo mediastinoscopy and an MRI of the left brachial plexus.
Case Continued
Mediastinoscopy is negative. MRI scan is obtained.
▪ MRI Scan
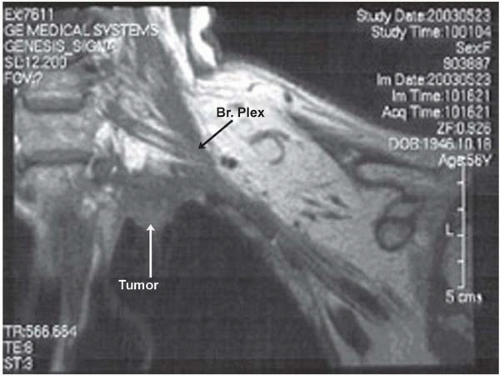 Figure 10.2A
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|