Cardiovascular Disorders: Introduction
Physiological Changes
In using data on physiological changes of the cardiovascular system, it is important to recognize the selection criteria of the population studied. Because the prevalence of coronary artery disease in asymptomatic individuals may be 50% in the eighth and ninth decades of life, screening to exclude occult cardiovascular disease may modify findings.
In a population screened for occult coronary artery disease, there is no change in cardiac output at rest over the third to eighth decades (Gerstenblith, Renlund, and Lakatta, 1987) (Table 11–1). There is a slight decrease in heart rate and a compensatory slight increase in stroke volume. This is in contrast to studies in unscreened individuals, where cardiac output falls from the second to the ninth decades. Consistent with the principle of decreased responsiveness to stress in aging, during maximal exercise, other changes are manifest even in the screened population (Table 11–2). Heart rate response to exercise is decreased in older adults compared to younger individuals, reflecting a diminished β-adrenergic responsiveness in aging. Cardiac output is decreased slightly. Cardiac output is maintained by increasing cardiac volumes—increasing end-diastolic and end-systolic volumes. With this increase in workload and the work of pumping blood against less-compliant arteries and a higher blood pressure, cardiac hypertrophy occurs even in the screened elderly population.
Unscreened for occult CAD | Screened for occult CAD | |
|---|---|---|
Heart rate | − | − |
Stroke volume | − − | + |
Stroke volume index | − − | 0 |
Cardiac output | − − | 0 |
Cardiac index | − − | 0 |
Peripheral vascular resistance | + + | 0 |
Peak systolic blood pressure | + + | + + |
Diastolic pressure | 0 | 0 |
Compared with 30-year-olds | |
|---|---|
Heart rate | − − |
End-diastolic volume | + + |
Stroke volume | + + |
Cardiac output | − |
End-systolic volume | + + |
Ejection fraction | − − |
Total peripheral vascular resistance | 0 |
Systolic blood pressure | 0 |
Because myocardial reserve mechanisms are used to maintain normal function in aging, older persons are more vulnerable to developing dysfunction when disease is superimposed.
Diastolic dysfunction—retarded left ventricular filling and higher left ventricular diastolic pressure—is present both at rest and during exercise in older persons. Older persons are more dependent on atrial contraction, as opposed to ventricular relaxation, for left ventricular filling, and thus are more likely to develop heart failure if atrial fibrillation ensues. Heart failure may occur in the absence of systolic dysfunction or valvular disease.
Hypertension
Hypertension is the major risk factor for stroke, heart failure, and coronary artery disease in older adults; all are important contributors to mortality and functional disability. Because hypertension is remediable and its control may reduce the incidence of coronary heart disease and stroke, increased efforts at detection and treatment of high blood pressure are indicated.
Hypertension is defined as a systolic blood pressure of 140 mm Hg or greater and/or a diastolic blood pressure of 90 mm Hg or greater. Isolated systolic hypertension is defined as a systolic pressure of 140 mm Hg or greater with a diastolic pressure of less than 90 mm Hg. With these definitions, as many as 67% of individuals older than age 60 may be hypertensive (Ostchega et al., 2007).
Despite the high prevalence of hypertension in older adults, it should not be considered a normal consequence of aging. Hypertension is the major risk factor for cardiovascular disease in older adults, and that risk increases with each decade. Both elevation of systolic blood pressure and pulse pressure are better predicators of adverse events than diastolic pressure. This is particularly relevant to older individuals, in whom isolated systolic hypertension predominates and may be present in 90% of hypertensive patients over the age of 80 (reviewed in Chobanian, 2007).
The diagnosis should be made on serial blood pressures. In patients with labile hypertension, blood pressure should be averaged to make the diagnosis, because these patients are at no less risk than those patients with stable hypertension. The history and physical examination should be directed toward assessing the duration, severity, treatment, and complications of the hypertension (Table 11–3). Atherosclerosis may interfere with occlusion of the brachial artery by a blood pressure cuff, leading to erroneously elevated blood pressure determinations, or “pseudohypertension.” Such an effect can be determined by the Osler maneuver. The cuff pressure is raised above systolic blood pressure. If the radial artery remains palpable at this pressure, significant atherosclerosis is probably present and may account for a 10- to 15-mm Hg pressure error. Standing blood pressure should also be determined. Initial laboratory evaluation should include urinalysis; complete blood cell count; measurements of blood electrolytes and calcium, estimated glomerular filtration rate, fasting glucose, and lipids; and 12-lead electrocardiogram (ECG). Although not all hypertension experts agree, the recent guidelines from the United Kingdom’s National Institute for Health and Clinical Excellence (NICE) recommend using ambulatory blood pressure monitoring to confirm the diagnosis of hypertension (Krause et al., 2011).
History Duration Severity Treatment Complications Other risk factors Physical examination Blood pressure, including Osler maneuver and standing determinations Weight Funduscopic, vascular, and cardiac examination for end-organ damage Abdominal bruit Neurological examination for focal deficits Laboratory tests Urinalysis Electrolytes Estimated glomerular filtration rate Calcium Thyrotropin (TSH) Chest radiograph Electrocardiogram |
Secondary forms of hypertension are uncommon in older adults but should be considered in treatment-resistant patients and in those with diastolic pressures greater than 115 mm Hg (Table 11–4). Pheochromocytoma is uncommon in older adults and is particularly unusual in those older than age 75. Atherosclerotic renovascular hypertension and primary hyperaldosteronism may occur more frequently in older persons. With the use of automated calcium determinations, the frequency of diagnosis of primary hyperparathyroidism is increasing, particularly in postmenopausal women. Because there is a causal link between this disorder and hypertension, the diagnosis and treatment of hyperparathyroidism may ameliorate the elevated blood pressure.
Estrogen therapy in the postmenopausal woman may be associated with hypertension. Such an association can be assessed by withdrawing estrogen therapy for several months and following the blood pressure response.
The issue of treatment of systolic/diastolic or isolated systolic hypertension in older individuals has been resolved. Multiple large trials have demonstrated that treating hypertension in older adults decreases morbidity and mortality from coronary artery disease and stroke (reviewed in Joint National Committee, 2004; for NICE guidance, see Krause et al., 2011). Although there has been concern about the hazard of treating individuals with cerebrovascular disease, the evidence suggests that the presence of cerebrovascular disease is an indication for, rather than a contraindication to, hypertensive therapy.
Some of the treatment trials that have included individuals up to 84 years suggest that there should be no age cutoff above which high blood pressure is not treated. A study specifically directed to hypertensive patients (systolic blood pressure of 160 mm Hg or more) age 80 years or older demonstrated a 30% reduction in the rate of fatal and nonfatal stroke, a 21% reduction in the rate of death from any cause, a 23% reduction in the rate of death from cardiovascular causes, and a 64% reduction in the rate of heart failure (Beckett et al., 2008). Relatively healthy older persons at any age should be treated unless they have severe comorbid disease that will clearly limit their life expectancy or unless the toxicity of treatment is so great that it outweighs potential benefits. The treatment goal for uncomplicated hypertension is a blood pressure less than 140/90 mm Hg. Despite the NICE guidance, controversies on management and treatment blood pressure goals persist (Godlee, 2012). Cardiovascular outcomes may not be improved with blood pressures below 130/85 mm Hg. Systolic blood pressures below 120 mm Hg may be associated with increased all-cause mortality in those age 85 and older (Molander et al., 2008), and higher blood pressure is associated with better cognitive function in those over 85 (Euser et al., 2009).
Guidance from the American College of Cardiology and the American Heart Association (AHA) for the treatment of hypertension in older adults has recently been published (Aronow et al., 2011). Lifestyle changes are not easily accomplished but should be attempted, including maintaining ideal body weight, limiting dietary sodium intake, eating fruits and vegetables and low-fat dairy products, reducing saturated and total fats, and engaging in aerobic exercise. Foods rich in potassium, calcium, and magnesium should be consumed. Excess sodium intake and potassium deficit have adverse effects on arterial pressure and should be reversed as part of the management of all hypertensive patients (Adrogué and Madias, 2007). Other risk factors, such as smoking, dyslipidemia, and diabetes mellitus, should also be modified.
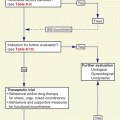
If dietary measures fail to control blood pressure, drug therapy should be considered. Physiological and pathologic changes of aging should be considered in individualizing the therapy. Changes in volumes of distribution and hepatic and renal metabolism may alter pharmacokinetics (see Chapter 14). Changes in vessel elasticity and baroreceptor sensitivity may alter responses to posture and drug-induced falls in blood pressure.
Thiazide diuretics are usually the initial step in therapy, especially in older patients with isolated systolic hypertension. They are well tolerated, are relatively inexpensive, and can be given once a day (Table 11–5). Many older hypertensive patients can be treated with diuretics as the only medication. Low-dose thiazides, for example, 12.5 to 25 mg of chlorthalidone, are efficacious in lowering blood pressure, while minimizing metabolic side effects. Many experts prefer chlorthalidone over hydrochlorothiazide as a better antihypertensive. Higher doses have a minimal additional effect on blood pressure with a more marked effect on hypokalemia. Thiazides are contraindicated in patients with gout. Postural hypotension is uncommon, but serum potassium should be monitored. Diabetics may have increased requirements for insulin or oral hypoglycemic agents.
Advantages | Adverse effects |
|---|---|
Well tolerated No central nervous system side effects Relatively inexpensive Infrequent dosing Good response rate Orthostatic hypotension uncommon Can be used in conjunction with other agents Effective in advanced age Effective in systolic hypertension | Hypokalemia Volume depletion Hyponatremia Hyperglycemia Hyperuricemia Impotence |
Although β-blockers are also recommended as initial-step therapy, several meta-analyses have called this strategy into question (reviewed in Panjrath and Messerli, 2006). These meta-analyses indicate that traditional β-blockers do have efficacy in lowering blood pressure but are not known to be effective in preventing coronary artery disease, cardiovascular mortality, or all-cause mortality in older adults. When compared to each other, thiazides are superior to β-blockers in older adults (MRC Working Party, 1992). In the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), thiazides were superior to angiotensin-converting enzyme (ACE) inhibitors in reducing cardiovascular disease, stroke, and heart failure (ALLHAT Collaborative Research Group, 2002). However, another trial suggests that ACE inhibitors are superior in older subjects, particularly men, in reducing cardiovascular events and mortality, but not stroke (Wing et al., 2003). β-Blocking agents may be used as the initial drug when another indication for their use exists, such as coronary heart disease, myocardial infarction (MI), heart failure, tachyarrhythmias, or essential tremor.
If thiazides alone do not control blood pressure, a second agent is added (Table 11–6) or a thiazide is added if one of the other agents has failed. The choice should be individualized and usually selected from among β-blockers, calcium channel antagonists, ACE inhibitors, or angiotensin-receptor blockers (ARBs) (The Medical Letter, 2001). β-Blockers are indicated for treatment of angina, heart failure, previous MI, and tachyarrhythmias in association with hypertension. These agents are contraindicated in patients with cardiac conduction deficits, bradyarrhythmias, and reactive airways disease. The more water-soluble β-blockers may be well suited for the geriatric population because they enter the central nervous system less readily and thus have fewer of the central nervous system side effects such as somnolence and depression; this would be a particular advantage in older adults. However, if cardiac output is decreased, renal perfusion and glomerular filtration rate may be affected. One concern with β-blockers is the production of bradycardia with reduced cardiac output. One simple test to monitor for this side effect is the patient’s response to mild exercise after each dosage increase; a failure to increase pulse by at least 10 beats per minute is an indication to reduce the dosage. If a patient is to be taken off a β-blocking agent, withdrawal should be done slowly over a period of several days to avoid rebound of original symptoms.
Agent* | Advantages | Disadvantages |
|---|---|---|
β-Blockers | Useful in angina, previous myocardial infarction, heart failure Water-soluble agents have fewer central nervous system side effects Must be withdrawn slowly in presence of coronary artery disease | Contraindicated in cardiac conduction defects and reactive airways disease May cause bronchospasm, bradycardia, impaired peripheral circulation, fatigue, and decreased exercise tolerance |
Calcium channel blockers | Peripheral vasodilator Coronary blood flow maintained Potency increased with age or in systolic hypertension | Headaches Sodium retention Negative inotropic effect Conduction abnormality |
Angiotensin-converting enzyme inhibitors | Preload and afterload reduction | Hyperkalemia |
Use in congestive heart failure, diabetes mellitus, other nephropathy with proteinuria | Hypotension Decreased renal function Cough Angioedema | |
Angiotensin-receptor antagonists | Use in angiotensin-converting enzyme inhibitor–induced cough, congestive heart failure, diabetes mellitus, other nephropathy with proteinuria | Hyperkalemia Angioedema (rare) |
Clonidine | Increased renal perfusion | Somnolence, depression Dry mouth, constipation Rarely, withdrawal hypertensive crisis |
α-Blockers | Useful in benign prostatic hypertrophy | Orthostatic hypotension |
Hydralazine | May be useful in systolic hypertension | Reflex tachycardia, aggravation of angina Lupus-like syndrome at high dosage |
Eplerenone | Aldosterone-receptor antagonist Fewer side effects than spironolactone and avoidance of gynecomastia | Hyperkalemia Contraindicated in renal insufficiency (creatinine >2.0) and in the presence of albuminuria |
Calcium channel antagonists are peripheral vasodilators with the advantage of maintaining coronary blood flow. These agents appear to have increased potency with age, possibly as a result of the decreased reflex tachycardia and myocardial contractility in older adults as compared with younger individuals. Headache, sodium retention, negative inotropic effects—especially in combination with β-blockers—and conduction abnormalities may limit their use. Calcium channel antagonists are effective in reducing stroke incidence in older patients with isolated systolic hypertension (Staessen et al., 1997). However, these drugs do not significantly reduce the risk of heart failure (Blood Pressure Lowering Treatment Trialists’ Collaboration, 2000).
ACE inhibitors are effective and well tolerated for treatment of hypertension. They are both preload and afterload reducers and thus are particularly useful in the face of congestive heart failure. They prolong survival in patients with heart failure or left ventricular dysfunction after an MI. Long-acting agents may have an advantage in adherence. Renal function, which may deteriorate on administration of these agents, must be monitored carefully. These agents may also induce hyperkalemia and should generally not be used with a potassium-sparing diuretic. Older adults are also more vulnerable to the hypotensive effects of these drugs.
ARBs are effective in lowering blood pressure without causing cough. They and ACE inhibitors are appropriate initial therapy in patients with diabetes mellitus, renal disease, or congestive heart failure (August, 2003). ARBs are superior to β-blockers in the treatment of patients with isolated systolic hypertension and left ventricular hypertrophy (Kjeldsen et al., 2002).
Clonidine may cause somnolence and depression, but it increases renal perfusion. The clonidine transdermal patch may lessen some of these adverse effects. However, local skin reactions may occur in about 15% of users. The once-per-week application of the patch may be an asset in improving adherence.
The major side effect of α-blockers is orthostatic hypotension; this is especially problematic with initial doses of prazosin. Newer agents with lesser hypotensive effects are now being used to treat symptomatic benign prostatic hypertrophy. In ALLHAT, the α-blocker arm was stopped early because of a higher incidence of congestive heart failure. Consequently, α-blockers are not recommended as monotherapy for hypertension.
Although hydralazine is usually a third-step drug, it may occasionally be used as a second-step drug in older adults because reflex tachycardia rarely occurs. If used with diuretics alone, it should be initiated in low doses, which should be increased slowly. It should not be used in the absence of a β-blocker if coronary artery disease is present.
A newer available agent is eplerenone, an aldosterone-receptor antagonist. It has a better side effect profile than spironolactone, particularly the avoidance of gynecomastia in men, but needs to be used with caution in patients with renal insufficiency and microalbuminuria, and potassium must be monitored for development of hyperkalemia.
With the newer, more effective agents, drug-resistant hypertension is unusual. In such cases, drug adherence should be monitored and sodium intake assessed. If such factors are not contributing to drug resistance, secondary causes of hypertension should be considered, especially renovascular disease and primary hyperaldosteronism.
Stroke and Transient Ischemic Attacks
Although the incidence of stroke is declining, it is still a major medical problem affecting approximately 50,000 individuals in the United States every year. It is the third leading cause of death and is also a major cause of morbidity, long-term disability, and hospital admissions. Stroke is clearly a disease of older adults; approximately 75% of strokes occur in those older than age 65. The incidence of stroke rises steeply with age, being 10 times greater in the 75- to 84-year-old age group than in the 55- to 64-year-old age group.
Table 11–7 lists the types and outcomes of stroke. In cerebral infarct, thrombosis, usually arteriosclerotic, is the most common cause, with embolization from an ulcerated plaque or myocardial thrombosis being less frequent causes. Table 11–8 lists outcomes for survivors.
Table 11–9 lists the modifiable risk factors for ischemic stroke. Hypertension is the major risk factor. Systolic hypertension is associated with a three- to fivefold increased risk for stroke. Hypertension accelerates the formation of atheromatous plaques and damages the integrity of vessel walls, predisposing to thrombotic occlusion and cerebral infarction. Hypertension also promotes growth of microaneurysms in segments of small intracranial arteries. Those lesions are sites of intracranial hemorrhage and lacunar infarcts.