19.1 Introduction
Cardiovascular disease is usually assumed to include coronary heart disease (CHD) [also referred to as coronary artery disease (CAD) or ischemic heart disease (IHD)], cerebrovascular disease and peripheral arterial disease. Inappropriate nutrition has most consistently been associated with CHD and this chapter therefore deals principally with the diet–CHD link. The association between diet and cerebrovascular disease will be considered briefly. Few data are available concerning the role of diet and peripheral arterial disease.
The basic pathological lesion underlying CHD is the atheromatous plaque which bulges on the inside of one or more of the coronary arteries that supply blood to the heart muscle (myocardium). In addition, a superimposed thrombus or clot may further occlude the artery. A variety of cells and lipids is involved in the pathogenesis of the atherosclerotic plaque and the arterial thrombus, including lipoproteins, cholesterol, triglycerides, platelets, monocytes, endothelial cells, fibroblasts and smooth-muscle cells. Nutrition can influence the development of CHD by modifying one or more of these factors. Two major clinical conditions are associated with these processes.
Angina pectoris is characterized by pain or discomfort in the chest that is brought on by exertion or stress, and which may radiate down the left arm and to the neck. It results from a reduction or temporary block to the blood flow through the coronary artery to the heart muscle. The pain usually passes with rest and seldom lasts for more than 15 min.
Coronary thrombosis, or myocardial infarction, results from prolonged total occlusion of the artery, which causes infarction or death of some of the heart muscle cells and is associated with prolonged, and usually excruciating, central chest pain. The terms coronary thrombosis and myocardial infarction are used to describe the same clinical condition, although they really describe pathological processes.
Standard epidemiological approaches including an examination of trends in rates over time, geographical variation, migrant studies, case–control and prospective studies, and clinical trials have been used to identify risk factors and their nutritional determinants. Such studies also provide the basis of recommendations that aim to reduce the risk of developing CHD in populations where rates are high or increasing. A population-based approach is essential since, in more than half of all fatal myocardial infarctions, death occurs in the first hour after the attack. Most CHD deaths, therefore, occur too rapidly for treatment to influence the prognosis.
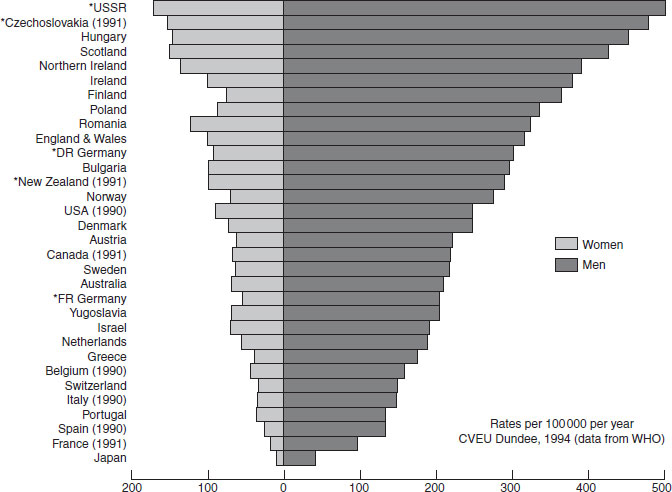
Figure 19.1 International differences in coronary heart disease rates. League table for 1992: mortality in men and women aged 40–69 years (Cardiovascular Epidemiology Unit, University of Dundee). *Former states. Reproduced with permission from Tunstall-Pedoe et al. (1999).
In most industrialized countries CHD is the most common single cause of death and a major cause of admission to hospital. However, mortality and hospital statistics appreciably underestimate the total morbidity resulting from CHD. Some cases of myocardial infarction, especially in older people, are not admitted to hospital and there are no statistics regarding the far greater number of people who are debilitated by angina pectoris even though they may not have suffered an acute myocardial infarction.
19.2 Epidemiology
There are marked international differences in the rate of occurrence of CHD. The lower rates in communities following their traditional lifestyle than in more affluent industrialized countries has long been recognised. However, Figure 19.1 shows that even among industrialized countries, mortality rates also vary considerably. Some of the variation between countries is undoubtedly due to differences in diagnostic practice and coding of death certificates, but numerous studies using comparable methods have confirmed that real differences exist in the frequency of the disease. In Europe there is an approximately four-fold difference between France, Spain and Portugal on the one hand, and such countries as Finland, Scotland and Northern Ireland on the other, but now, eastern European countries such as Hungary, former Czechoslovakia and the former USSR are in the worst position.
These international comparisons have played an important part in the search for causes. The experience of migrants suggests that these variations between countries are likely to be the result chiefly of environmental and behavioral differences. People who have migrated from a low-risk country (e.g. Japan) to a high-risk country (e.g. the USA) tend to have rates of CHD approaching those of the host country. There is also some evidence for the reverse: Finns living in Sweden have appreciably lower rates than those in their country of origin. In the UK, where CHD rates are appreciably higher in Scotland and Northern Ireland than in England, CHD risk depends on country of residence at the time of death rather than country of birth.
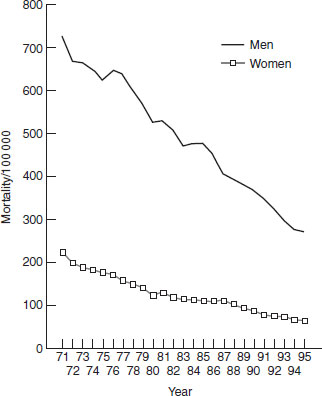
There have been major changes in the CHD rates of many countries. Among men these include the increase in many European countries, Australia and New Zealand during the period 1952–1967, and the continuing increase in eastern Europe during the later period of 1970–1985, whereas in nearly all Western European countries, North American and Oceania rates have shown an appreciable decline. Figure 19.2 shows the dramatic reduction in Finland, the country that had the highest CHD mortality rates in the world in the 1960s. In most countries except for eastern Europe, the rates in women have been declining. In general, the decline has been most marked in countries where the attempt to reduce cardiovascular risk factors has been most effective. These changes over a relatively short period encourage the belief that the disease is preventable if the causes can be found and modified. They certainly argue strongly against the suggestion that the powerful genetic factors involved in CHD are likely to negate the beneficial effect of environmental change. The hope is to reduce morbidity and mortality from CHD in those who are in the prime of life.
19.3 Correlations between coronary heart disease rates and food intake
Most of the early attempts to study dietary determinants of CHD rates were based on food or nutrient data derived from national food consumption data, the balance sheets of the Food and Agriculture Organization or, in the UK, more reliably, on household food surveys and on the national mortality statistics before 1970, during which time CHD was increasing (at least in men) in most affluent societies. The studies have either been cross-cultural comparisons at a single point in time, or an examination of increasing trends in relation to changing food consumption data in one or more countries. Positive associations with saturated fat, sucrose, animal protein and coffee, and negative correlations with flour (and other foods rich in polysaccharides) and vegetables are some of the best described. However, population food consumption data are notoriously unreliable (they are usually derived from local production figures, imports and exports, often with an incomplete account of quantities not utilized as food), and the accuracy with which mortality is recorded varies from country to country. Consequently, such data do not provide direct evidence concerning etiology, only clues for further research.
Figure 19.2 Age-adjusted cardiovascular mortality in men and women in Finland from 1972 to 1995. Source: Statistics Finland. Reproduced with permission from Pietinen et al. (2001). © Springer Publishing Company, Inc.
Other studies from the USA, the UK, Australia, New Zealand, Finland and Iceland have examined the downward trend of CHD rates in relation to dietary change. There are certainly associations between falling CHD rates apparent in these countries and changes in some foods and nutrients, but in view of the strong correlations (positive and negative) among different dietary constituents it is difficult to be sure which dietary factor is principally involved, or indeed whether dietary change is simply occurring in parallel with some other more important environmental factor, for example, increasing physical activity and reduction in cigarette smoking. The most recent estimate regarding the potential for lifestyle and diet modification to reduce CHD risk in the USA suggests that 82% [95% confidence interval (CI) 58 to 93%] of coronary events could be prevented by adhering to guidelines involving diet, exercise, body weight and abstinence from smoking.
19.4 Prospective observation of subjects for whom diet histories are available
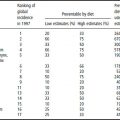
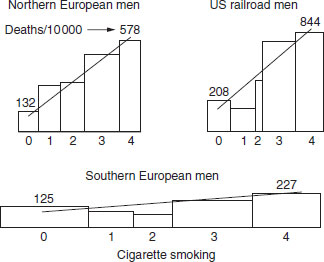
Measured food consumption by people in 16 defined cohorts in seven countries, and 10 year incidence rates of CHD deaths, form the basis for the correlations tested by Keys and coworkers in the classic Seven Country Study. The strongest correlation was noted between CHD and the percentage of energy derived from saturated fat (Figure 19.3). Weaker inverse associations were found between percentages of energy derived from monounsaturated and polyunsaturated fat and CHD. Total fat was not significantly correlated with CHD death. Of the other well-known risk factors for CHD investigated in this study, only cholesterol and blood pressure appeared to explain the geographical variation, leading to the suggestion that it is principally the nutrition-related factors that determine whether countries are likely to have high CHD rates. This study also provides evidence that the degree of risk conferred by factors not specifically related to nutrition is strongly influenced by nutrition-related factors. This is well illustrated by the more powerful relationship between cigarette smoking and CHD in the USA and northern Europe than in southern Europe. Saturated fat intake and mean cholesterol levels are higher in the USA and northern Europe than in southern Europe (Figure 19.4).
Figure 19.3 Data from the original Seven Country Study showing the association between coronary heart disease and dietary saturated fat content. B: Belgrade; C: Crevalcore; D: Dalmatia; E: East Finland; G: Corfu; J: Ushibuka, K: Crete; M: Montegiorgio; N: Zutphen; R: Rome; S: Slavonia; T: Tanushimaru; U: USA; V: Velika Krsna; W: West Finland; Z: Zrenjanin.
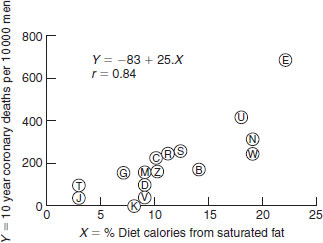
Figure 19.4 Different risks of smoking for coronary heart disease (CHD) in countries with different diets. The width of the bars is proportional to the number of men in each smoking class. Scales are the same for all three populations. The numbers above each bar indicate the number of CHD deaths per 10 000. The regression lines of death rate on smoking are shown. 0: never smoked; 1: exsmoker; 2: 2–10 cigarettes/day; 3: 10–19 cigarettes/day; 4: >20 cigarettes/day.
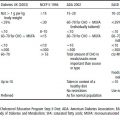
Several longitudinal studies have related reported intake of foods or nutrients to subsequent cardiovascular disease risk. Such studies have several potential methodological flaws, most notably the insensitivity of the instruments for measuring dietary intake in epidemiological studies and the inability of a single assessment to provide a representative indication of usual dietary practice. Despite these, and other causes of imprecision, a range of biologically plausible associations has been identified. Most consistent among the protective foods and nutrients are fish, whole-grain products, fruit and vegetables, nuts, garlic and moderate amounts of red wine, antioxidant nutrients (vitamins E and C, β-carotene and flavonoids), folic acid, nonstarch polysaccharides (dietary fiber) and several long-chain fatty acids (C18:2 n-6, C18:3 n-3, C20:5 n-3). In contrast, saturated fatty acids (SFA), trans-unsaturated fatty acids, dietary cholesterol and foods rich in these nutrients, as well as coffee, all appear to be associated with enhanced risk. While the data are not entirely consistent (e.g. in some studies the protective effect of antioxidant nutrients appears to be largely mediated via high dietary intakes, in others as a result of high intakes of supplements), the effects appear to be relatively strong. Table 19.1 summarizes the associations between dietary factors and CHD demonstrated in the Health Professionals, and Nurses, Studies carried out by the Harvard group.
Table 19.1 Associations between dietary factors and coronary heart disease: findings from the Nurses Health Study and Health Professionals Study
| Food or nutrient | Protective/deleterious effect |
| Saturated fat (SFA) | 5% en SFA vs 5% en CHO, RR = 1.17 (95% CI 0.97 to 1.41) |
| trans fat (TFA) | 2% en TFA vs 2% en CHO, RR = 1.93 (95% CI 1.43 to 2.61) |
| Monounsaturated fat (MUFA) | 5% en MUFA vs 5% en CHO, RR = 0.81 (95% CI 0.65 to 1.00) |
| Polyunsaturated fat (PUFA) | 5% en PUFA vs 5% en CHO, RR = 0.62 (95% CI 0.46 to 0.85) |
| α-Linolenic acid (ALA) | Highest vs lowest quintile of intake, RR = 0.52 (95% CI 0.30 to 0.90) |
| Fish n-3 fatty acids | Weekly compared with less than weekly fish intake for sudden death, RR = 0.48 (95% CI 0.24 to 0.96) |
| Nuts | Eaten more than five times per week vs with rare consumption, RR = 0.65 (95% CI 0.47 to 0.89) |
| Whole grains | Highest vs lowest quintile of intake, RR = 0.75 (p for trend = 0.01) |
| Dietary fiber | Each 10g increase in total fiber, RR = 0.81 (95% CI 0.66 to 0.99) |
| Carbohydrate | Highest vs lowest quintile glycemic loada, RR = 1.98 (95% CI 1.41 to 2.77) |
| Antioxidants and folate | High intakes of vitamin E and folate strongly protective. Less consistent associations with other antioxidants |
| Protein | Highest vs lowest quintile, RR = 0.74 (95% CI 0.59 to 0.94) |
aGlycemic load provides an indication of both amount of carbohydrate and glycemic index, i.e. the extent of blood glucose elevation produced by the carbohydrates consumed.
SFA: saturated fatty acids; TFA: trans unsaturated fatty acids; MUFA: monounsaturated fatty acids; PUFA: polyunsaturated fatty acids; en: total energy; CHO: carbohydrate; RR: relative risk; CI: confidence interval.
In addition to these individual foods and nutrients, certain dietary patterns appear to be associated with a low CHD risk. Vegetarians appear at lower risk of CHD than meat eaters, but it has not been clearly established which attributes of the vegetarian diet might be protective, since there are many aspects other than the absence of meat which characterize these diets. Moreover, vegetarians often adopt many other lifestyle attributes that may confound comparisons with omnivores. The “prudent pattern” (high intakes of vegetables, fruit, legumes, whole grains, fish and poultry) when consumed within the context of a Western diet also appears to be protective. There has also been much publicity surrounding the relatively low CHD rates associated with traditional regional and national dietary patterns (e.g. the Mediterranean diet and the Japanese diet).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree