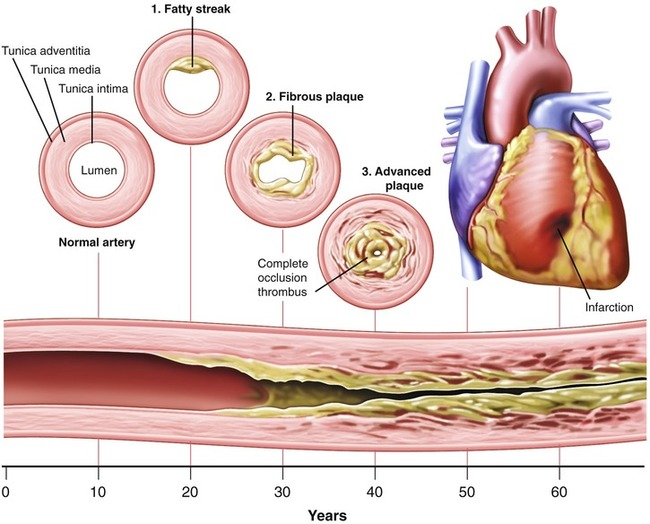
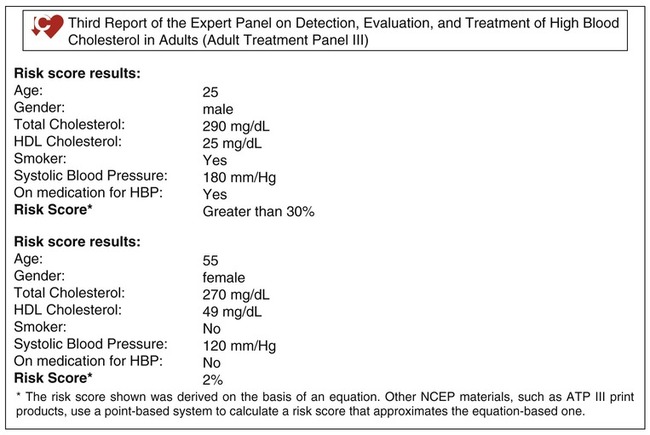
After completing this chapter, you should be able to: • Identify risk factors related to the development of cardiovascular disease. • Discuss medical nutrition therapy goals for cardiovascular disease and hypertension. • Discuss appropriate foods to prevent or manage cardiovascular disease. • Discuss the role of the nurse or other health care professional in the prevention and management of cardiovascular disease. Cardiovascular disease (CVD), often interchangeably described as coronary artery disease (CAD) or coronary heart disease (CHD), the latter being the more-inclusive term, remains the leading cause of death for Americans and around the world for both men and women. There are many lifestyle factors contributing to this. There are also many causal factors for CHD unrelated to diet and lifestyle, such as bacterial infections and genetic anomalies. Atherosclerosis (the condition of plaque buildup in the circulatory system—see Figure 7-1) is a complex disease that involves chronic inflammation. The role of stress continues to receive attention with regard to its effects on CVD. Our fast-paced lifestyle may be contributing to CVD. One study found that relaxation practice enhanced recovery from a heart attack and helped prevent a recurrence (van Dixhoorn and White, 2005). CVD relates to the heart and the entire vascular system. Therefore hypertension (high blood pressure), cerebrovascular accident (CVA), or, more commonly, stroke, and arteriosclerosis (hardening of the arteries) are all examples of CVD. A transient ischemic attack (TIA) is referred to as a ministroke. Thrombosis is the formation of clots. Clots can be stationary when attached to the walls of blood vessels but can later dislodge and plug a smaller blood vessel. The majority of individuals with diabetes mellitus die from a thrombosis. This is, in part, caused by the enhanced activation of platelets and clotting factors seen in diabetes. Fibrinogen levels, which are related to increased clotting, have been associated with mortality after incidence of heart attack and may serve as a marker for increased risk for recurrence (Coppola and colleagues, 2005). Atherosclerosis is a complex disease of the arteries; it is a form of arteriosclerosis. The passageways through the arteries become roughened and clogged with fatty deposits such that blood cannot flow freely, like clogged sink pipes (Figure 7-1). This is the form of heart disease described as ischemic. Atherosclerosis is thought to be a cause of coronary thrombosis, myocardial infarction (MI) (heart attack, or coronary), and CVA. Peripheral arterial disease (PAD) is a form of atherosclerosis and is associated with significant cardiovascular morbidity and mortality. PAD is defined as an ankle-brachial blood pressure index of less than 0.9 in either leg. As shown from the NHANES 1999 to 2004 data, PAD prevalence increases with age and is found in about 1 in 4 persons 80 years of age and older. Non-Hispanic black men and women and Mexican American women have a higher prevalence of PAD than non-Hispanic white men and women, with other risk factors being current or previous: smoking, diabetes mellitus, low kidney function, high-sensitivity C-reactive protein level greater than 3.0 mg/L, and uncontrolled hypertension, treated or not (Ostchega and colleagues, 2007). High-density–lipoprotein cholesterol (HDL-C), low-density–lipoprotein cholesterol (LDL-C), and very-low-density lipoprotein (VLDL) are all forms of cholesterol found in the blood. Lipids is the term used to describe all forms of fat found in the blood. Chylomicrons are another form of lipoprotein. VLDL is the main carrier of triglycerides (a type of blood fat) synthesized in the body. Hypercholesterolemia refers to elevated total cholesterol level but is usually a result of high serum LDL-C. Hyperlipidemia is the term generally used to describe a combination of high levels of LDL-C and triglycerides. Dyslipidemia, as discussed in Chapter 5, refers to low levels of HDL-C but usually coexists with elevated triglycerides. LDL-C is often referred to as “bad cholesterol.” It is well recognized that a high level of LDL-C induces atherosclerosis and is a strong risk factor for heart disease. The majority of cholesterol medications are aimed at lowering LDL-C. Diet can have a strong influence, but it can take at least 3 months for an impact to be seen. Unfortunately, not everyone responds to changes in the diet. However, because there are no adverse health outcomes with medical nutrition therapy (MNT), this is advised as the primary strategy before use of medications (Table 7-1). Table 7-1 Medical Nutrition Therapy for Lipoprotein Management HDL-C, High-density–lipoprotein cholesterol; LDL-C, low-density–lipoprotein cholesterol. It was as recently as the early 1990s that elevated triglyceride levels started being recognized as a contributor to CVD, although controversy still exists as to its role in CVD. In recent years the American Heart Association (AHA) lowered the definition of high fasting triglyceride level from 200 to 150 mg/dL. This was a result of the realization that the higher the fasting triglyceride level, the greater the rise of postprandial triglycerides. It has been shown among women that triglyceride levels, in either fasting or fed states, correlated with known cardiac risk factors and indicators of insulin resistance. However, elevated triglyceride levels measured 2 to 4 hours postprandially had the strongest association with cardiovascular events (Bansal and colleagues, 2007). Arterial stiffness has been noted in women with elevated triglyceride levels and CVD (Le and colleagues, 2005). Total cholesterol level should be less than 200 mg/dL. The National Cholesterol Education Program (NCEP) indicates the goal for LDL-C is less than 130 mg/dL for moderately high-risk persons (two or more risk factors and a 10-year risk for CHD of 10% to 20%—see Figure 7-2). The NCEP III guidelines state that in very high-risk patients a LDL-C level of less than 70 mg/dL is a reasonable goal, regardless of age (Aronow, 2006). Triglyceride levels are advised to be less than 150 mg/dL, and HDL greater than 40 mg/dL for men and 50 mg/dL for women, with the goal being greater than 60 mg/dL to best help prevent CVD. However, triglyceride levels greater than 100 mg/dL have been linked with high C-reactive protein (CRP) levels, suggesting that fasting triglyceride levels under 100 mg/dL may further reduce CVD risk (Ahmad and colleagues, 2005). On the other hand, low levels of total cholesterol less than 160 mg/dL, referred to as hypocholesterolemia, can be an indicator of poor health. Lipid metabolism is known to be altered in many acute diseases. There are many potential causes of decreased serum cholesterol levels. Malabsorption is one factor, and this is likely the factor behind hypocholesterolemia with the active phase of Crohn’s disease. There may also be altered synthesis of cholesterol (Hrabovský and colleagues, 2007). In solid tumors and those of the blood, hypocholesterolemia may be due to increased use of cholesterol by cancer cells (Yavasoglu and colleagues, 2008). Hypocholesterolemia has been implicated in genetically based violent behavior (Edgar and colleagues, 2007). Low levels of cholesterol have been found to help predict mortality in critically ill surgical patients. Promotion of higher levels of cholesterol is advised for the management of critical illness (Bonville and colleagues, 2004). The guidelines of the NCEP now recommend that adults 20 years of age and older have their total cholesterol and HDL-C levels measured. If the total cholesterol is 200 mg/dL or more, or the HDL is less than 40 mg/dL, a complete lipoprotein profile is advised (including the LDL-C and triglyceride levels). In assessing risk for CHD it has been noted that total cholesterol level, blood pressure, and body mass index (BMI) showed average levels significantly higher during the winter months (Ulmer and colleagues, 2004). This is likely due, in part, to decreased production of vitamin D from a cholesterol-based hormone with reduced sunlight. Goals for MNT and use of medications vary depending on the differing levels of these lipids and risk factors. There is debate on goals and treatment for the elder population, in part due to limited research verifying the benefit of cholesterol-lowering medications. Polypharmacy, with excess prescription of medications, continues to be a potential problem especially for the elder population (see Chapter 13). Before the use of lipid-lowering medications, referral to a registered dietitian is advised by the AHA, unless the individual is at very high risk for an MI or CVA. • Elevated LDL-C (especially with small LDL particle size) • Hypertension: blood pressure of greater than or equal to 140/90 mm Hg or on antihypertensive medication • Low HDL-C (less than 40 mg/dL for men; less than 50 mg/dL for women) • Family history of premature CHD • CVD in male first-degree relative younger than 55 years • CVD in female first-degree relative younger than 65 years • Age (men 45 years of age or older; women 55 years or older) • Multiple metabolic risk factors (insulin resistance or metabolic syndrome) Monounsaturated fats, such as found with nut intake (see Figure 2-4), have been associated with reduced CHD risk. In addition to cholesterol-lowering properties, almonds have been shown to lower oxidized LDL concentrations. Antioxidant activity provides an additional possible mechanism, in addition to lowering cholesterol, that may account for the reduction in CHD risk with nut consumption (Jenkins and colleagues, 2008). Obesity is one of the risk factors for atherosclerosis and is related to LDL oxidation. It was found that with moderate kcalorie restriction, along with regular physical activity, in obese adolescents there was reduced lipid oxidation and improved body weight and composition (Lazzer and colleagues, 2005). As described in Chapter 5, the metabolic or insulin resistance syndrome is a diagnosis made by health correlations. The primary correlations are central obesity, hypertension, dyslipidemia, and type 2 diabetes, all of which are all risk factors for CHD. Having several of these health conditions is believed to further increase risk for CHD, and intensified risk management to lower risk is advised. Some of the causes of CHD as found with the metabolic syndrome include the following: The inflammatory marker CRP, as discussed in Chapter 5, is a risk factor for CVD. An approach in primary prevention is to measure CRP only among those at intermediate risk as defined by the Framingham risk score (see Figure 7-2). In secondary prevention, the potential utility of CRP is less certain (Corrado and Novo, 2007). Elevated CRP levels have been found with advanced atherosclerosis in adolescents and young adults (Zieske and colleagues, 2005). Adult Asian Indians have significantly higher CRP levels than do persons with European heritage (Misra, 2004). This may explain the higher risk for CVD in Asian Indians even when there is a normal HDL-C level. High levels of CRP and blood glucose are found in conjunction and jointly contribute to cardiovascular risk in men with type 2 diabetes (Bahceci and colleagues, 2005). Inflammation associated with periodontal disease is associated with development of early atherosclerotic carotid lesions (Soder and colleagues, 2005). A high level of homocysteine, a sulfur-containing amino acid, is often considered an important risk factor for CVD, including stroke. Hyperhomocysteinemia has been implicated in plaque formation found in atherosclerosis and is associated with hypertension (Curgunlu and colleagues, 2005). Elevated levels of homocysteine and nitric oxide (a substance related to epithelial function) were found in persons who required coronary artery bypass surgery and among their children (Pac and colleagues, 2005). However, more recent data suggest that homocysteine is a marker, and not the cause, of CVD (Wierzbicki, 2007). Although diabetes is a risk factor for CHD, a high-normal level of blood glucose is also a risk factor. Fasting glucose levels are associated with many cardiovascular risk factors, and a glucose level less than 75 mg/dL is associated with the lowest prevalence (Gupta and colleagues, 2007). Based on data from 1-hour plasma glucose challenge, it appears that maintaining normal glucose levels early in life may reduce later health care problems in older age (Liu and colleagues, 2005). Treatment of dyslipidemia, as found with the metabolic syndrome, has been effective in reducing CVD (Ginsberg, Zhang, and Hernandez-Ono, 2005). Not surprisingly, low levels of HDL found in adolescents are predictive of dyslipidemia in adulthood (Magnussen and colleagues, 2008). Vitamin D deficiency is being linked with the metabolic syndrome. Low 25(OH)D levels have been associated with the cardiovascular disease risk factors of hypertension, obesity, diabetes mellitus, and the metabolic syndrome, as well as cardiovascular disease events including stroke and congestive heart failure (Michos and Melamed, 2008). A postprandial state characterized by abnormally increased levels of glucose and lipids (postprandial dysmetabolism) is an independent predictor of future cardiovascular events, even in nondiabetic subjects. Suppressing the postprandial spikes in glucose and lipids improves inflammation and endothelial function and appears to help prevent atherosclerosis (O’Keefe and Bell, 2007). Hypertensive patients with high plasma insulin levels or metabolic syndrome have a greater occurrence of left ventricular hypertrophy, which appears related to hyperinsulinemia (Sharma and colleagues, 2007). This is attributed to altered metabolism. Low iron states in premenopausal women appear to be protective against CHD (Ozdemir and colleagues, 2007). The Increased CHD after menopause, when risk approaches that observed in men of similar age, may be due to higher levels of iron. However, this phenomenon is more likely in women with central obesity, or apple shape, and other factors of the metabolic syndrome. It has been observed that carrying excess body fat in the thighs (pear shape) rather than in the abdominal region helps protect against cardiovascular disease and diabetes in obese postmenopausal women (Aasen, Fagertun, and Halse, 2008; Faloia and colleagues, 2009). Women who have menstrual irregularities often have indicators of insulin resistance, and it may be hormonal changes that increase risk of CVD among women. Increased menstrual cycle length between menstruation greater than 30 days has been implicated in increased risk of CVD with a trend toward higher LDL-C level and dyslipidemia (Rubba and colleagues, 2008). Women who are insulin sensitive have lower triglyceride and higher HDL-C levels. The triglyceride to HDL-C ratio is a predictor for glucose disposal rates (Karelis and colleagues, 2007). The metabolic syndrome may occur in 40% of postmenopausal women. Menopause promotes the development of central obesity among women. Hormonal replacement therapy has been found to worsen insulin resistance among women with the metabolic syndrome, although in general it is thought to increase insulin sensitivity (Lobo, 2008). • Females are at greater risk for early carotid atherosclerosis (Iglseder and colleagues, 2005). • Among Asian Indians, risk factors for CVD were found even with an HDL-C greater than 40 mg/dL (Superko and colleagues, 2005). • In Asian males the individual components of hyperlipidemia and hypertension were equivalent or better predictors of CVD than being diagnosed with the metabolic syndrome (Sone and colleagues, 2005). • Middle-age and older adults are at risk for arteriosclerosis with arteries losing their flexibility (S Li and colleagues, 2005). • Men with hypertension remain at a high risk for stroke, heart attack, and mortality from CHD, even with medically controlled blood pressure (Almgren et al., 2005). Persons with a relatively rare form of familial hypercholesterolemia cannot remove LDL-C from their systems. These individuals have dangerously high LDL-C levels that are resistant to MNT and medications. It has been noted that these individuals benefit from physical removal of blood LDL through medical procedures (Sachais and colleagues, 2005). Such individuals need to avoid even moderate intake of cholesterol such as found in egg yolks, shellfish, and organ meats. Genetic risk of metabolic syndrome also is associated with dyslipidemia. There are a variety of risk factors for stroke, including hypertension, diabetes, obesity, and lack of physical activity. Research related to stroke risk and the metabolic syndrome indicates that individuals with CVD, especially women, are at high risk for ischemic stroke or TIA (Koren-Morag, Goldbourt, and Tanne, 2005). Trans fatty acids increase risk of stroke. Protection from stroke occurs with omega-3 fatty acids and other unsaturated fats, including oleic, linolenic, and arachidonic fatty acids (see Chapter 2 for food sources—Table 2-5). The unsaturated fats appear protective in women but appear to increase risk of ischemic stroke in men (Monteiro and Vaz Almeid, 2007). Another benefit of omega-3 fats as found in fish oil includes increasing the size of LDL particles, making them more fluffy and less likely to adhere to the lining of vascular walls. A high glycemic load along with a higher intake of fatty meats has been found to increase stroke risk. A diet low in fruits, vegetables, fish, and whole grains is associated with increased risk of stroke (Fung and colleagues, 2004). High glycemic load is related to high postprandial insulin production and, along with reduced antioxidant vitamins with low intake of high-fiber plant-based foods, likely has an enhanced risk of atherosclerosis. Following stroke or TIA there is increased risk of future incidents. Riboflavin deficiency has been found to be common after stroke. Supplementation of vitamin B2 may be beneficial after CVA due to reduced oxidative damage and consequent cerebral edema (Gariballa and Ullegaddi, 2007). In obese, insulin-resistant persons, a calorie-restricted diet resulting in 10% to 15% weight loss and that is moderately lower in carbohydrate (40%) and higher in unsaturated fat has been found to be as effective as the traditional low-fat diet (60% carbohydrate) in producing weight loss. This approach also is more effective in lowering triglyceride and insulin levels and increasing HDL-C levels and the size of LDL particles (McLaughlin and colleagues, 2006). Approximately a 20-lb weight loss has been shown to lower fasting and postprandial triglyceride levels along with improving endothelial function and lowering inflammation. This was compared with the intake of 1 g/day of fish oil supplement alone, which reduced only postprandial triglyceride levels (Plat and colleagues, 2007). The triglyceride response to a high-carbohydrate meal has been found to increase immediately after a meal and 6 hours later. Weight reduction helps to lower the second postprandial triglyceride rise (Dallongeville and colleagues, 2007). Medical nutrition therapy (MNT) with a focus on the Dietary Approaches to Stop Hypertension (DASH) diet (see later section), as provided by a registered dietitian in a physician’s office, has been shown to promote an average of 5% weight loss in under a 2-year period. Over 80% of these individuals maintained the weight loss over a 30-month period. With the weight loss, lipids improved with an average drop of about 9% in LDL-C level, 35% in triglyceride level, and increase of HDL-C level of almost 10%. Blood pressure further improved (Welty and colleagues, 2007). In a study of individuals with Class I obesity there was a 3% weight loss over a 3-month period with lifestyle modification (exercise of at least 60 minutes three times a week) and a 1500-kcal diet with about 50% carbohydrate and 25% fat. There was significant improvement in anthropometric and cardiovascular risk factors (De Luis and colleagues, 2008). In one study, preschoolers were assessed for CVD risk initially and at follow-up 4 years later. Increasing BMI, waist circumference, and intake of sucrose at follow-up was found to lower HDL-C level and increase triglyceride levels. It was found that as intake of monounsaturated fat and dietary fiber increased there was a resulting reduction in total cholesterol level among the children (Williams and Strobino, 2008). There still remains controversy regarding cholesterol intake for heart health. Research shows conflicting outcomes. Data from free-living populations show that egg intake generally does not cause higher cholesterol levels. The most recent AHA guidelines no longer specifically advise limiting egg intake (Kritchevsky, 2004). However, the ATP III guidelines still advocate reduced cholesterol intake with a goal of less than 200 mg of cholesterol daily. This essentially limits egg, shellfish, and organ-meat intake. The yolk of a medium-sized egg is estimated to contain about 225 mg of cholesterol. Three ounces of beef liver contains over 400 mg of cholesterol. Canada does not have a specific guideline on cholesterol intake because of the evidence suggesting a closer link between saturated and trans fatty acid intake and increased endogenous production of cholesterol. For most healthy individuals, synthesis of cholesterol by the liver adjusts to the level of dietary cholesterol intake. One study found that with a restricted carbohydrate intake an additional 640 mg of cholesterol from eggs had an antiinflammatory effect with increased HDL-C. This finding may be due to the cholesterol itself or possibly due to the antioxidant lutein content of egg yolk, which helps lower an inflammatory response (Ratliff and colleagues, 2008). As with much of nutrition, individualized guidance should be advocated. Choline, for example, with the highest dietary sources being liver and eggs, has been shown to reduce homocysteine levels (Olthof and colleagues, 2005). Individuals who want to include whole eggs and liver in the diet because of taste preference and/or positive health associations should have their serum cholesterol levels assessed to ensure tolerance. Research outcomes of two studies further indicate the need for individualization. The first study found that in men, consumption of two or more eggs daily was not related to total cholesterol level as compared with a lower intake of eggs; for women, there was an association. Women who limit their intake to one to two eggs weekly had significantly lower cholesterol levels than those with daily consumption (Nakamura and colleagues, 2004). Among persons with insulin resistance, a high-cholesterol diet did not promote an increase in inflammation as indicated by CRP levels or non–HDL-C levels, but it did have an adverse effect among insulin-sensitive individuals (Tannock and colleagues, 2005). Generally, if LDL-C is at the very high risk level of over 200 mg/dL, cholesterol intake should be limited to under 200 mg daily average. If LDL is at a more moderately low risk level (Table 7-2), cholesterol intake can be more moderate as per food label guidelines at 300 mg daily. Table 7-2 ATP III Guidelines for Therapeutic Lifestyle Changes (TLC) Diet ATP III, Adult Treatment Panel III, LDL, low-density lipoprotein. From National Heart, Lung, and Blood Institute: Adult Treatment Panel guidelines for therapeutic lifestyle changes (TLC) diet, Washington, DC, 2001, National Institutes of Health. There is strong evidence that the type of fat rather than the total amount of fat is most important in preventing CVD. Low-fat diets have been advocated because this is one simple strategy to lower intake of saturated and trans fats. However, this can be confusing to the consumer who may assume that carbohydrates may be included freely in the diet with a low-fat diet, which would have an adverse effect on individuals with the metabolic syndrome. It also has been found that a very low-fat diet with 10% fat increased fasting triglyceride level and the total cholesterol to HDL-C ratio, whereas a moderate fat intake of 35% lowered triglyceride level and the total cholesterol to HDL-C ratio. This adverse impact of a very low-fat diet was found even in healthy, endurance-trained runners (Larson-Meyer and colleagues, 2008). As reviewed in Chapter 2, there are many forms of fatty acids. Some are beneficial to cholesterol levels and heart disease and others have adverse effects. In moderation, all may be included. Research continues on the impact of specific fatty acids. Although saturated fat is generally advised to be reduced in the prevention and management of CVD, a low intake of certain fats in butter has been found to be detrimental. This includes lauric acid from dairy products, with low intake being associated with acute MI. It is advised that recommendations on fatty acid intake should aim for both an upper and lower limit (Lopes and colleagues, 2007). Although saturated fat intake should be lowered to reduce risk of CVD, food sources are not always as clear. Among the 12 major milk fatty acids, only 3 (lauric, myristic, and palmitic—see Table 2-5) have been associated with raising total serum cholesterol levels. However, their individual effects are variable regarding impact on LDL-C and HDL-C (German and Dillard, 2006). Moderate supply of myristic acid (see Table 2-5) at less than 2% of total kcalories with the recommended intake of alpha-linolenic acid from canola oil at about 1% of total kcalories contributes to improved cholesterol removal from tissues into HDL-C, dependent on enzyme activity (Vaysse-Boué and colleagues, 2007). Although red meat is thought of as being high in saturated fat, it was found that lean red meat, trimmed of visible fat, did not increase cholesterol levels or risk of thrombosis (D Li and colleagues, 2005). A fast-food meal of a burger and fries was found to have more myristic (C14:0), palmitic (C16:0), stearic (C18:0), and trans fatty acids (C18:1) than an organic beef meal. LDL-C decreased more with the organic beef meal, which had lesser amounts of saturated and trans fatty acids, than in the fast-food beef meal (Bray and colleagues, 2007). It is now recognized that trans fatty acids act as saturated fats do in the body and have been linked with inflammation in women (Mozaffarian and colleagues, 2004). As reviewed in Chapter 2, hydrogenated fats are referred to as trans fatty acids. In the last 10 years or so, the adverse health effect of hydrogenated fats has been recognized. One explanation for the increased CVD associated with trans fatty acids is that they decrease HDL-C level (Dyerberg and colleagues, 2004). In January 2006, listing of the estimated amount of trans fatty acids on the Nutrition Facts section of food labels became mandatory; the listing can be found under saturated fats. As the percentage of kcalories from trans fatty acids increases, there is a linear impact on increasing LDL-C levels in relation to reducing HDL-C levels. There appears to be no safe level of intake of trans fatty acids, and they have double the adverse impact of saturated fats (Ascherio, 2006). The unsaturated fats in general are helpful for reducing LDL-C levels. In the 1970s only polyunsaturated fats (see Figure 2-4), as primarily found in seed and vegetable oils, were promoted as a means to normalize hypercholesterolemia. Although this was effective, the unintended effect was that HDL-C levels also were reduced with a high intake of polyunsaturated fats. Excess intake of the polyunsaturated type of fat found in seed oils, linoleic acid (see Table 2-5), has been shown to oxidize LDL-C and increase risk of clot formation (Khor, 2004). Further research has found monounsaturated fats lower LDL-C levels but are protective to the HDL-C levels, the desired effect. The form of polyunsaturated fats known as the omega-3 fatty acids do have beneficial effects and generally are advised. Diets rich in eicosapentaenoic acid (EPA), an omega-3 fatty acid, are associated with decreased arterial stiffness; adding EPA to a high-fat meal results in acute changes in vascular tone, independent of changes in oxidative stress (Hall and colleagues, 2008). For vegans or others who do not consume fatty fish, it is advised to increase intake of alpha-linolenic acid and decrease linoleic acid to promote the endogenous production of these longer chain n-3 polyunsaturated fatty acids (Griffin, 2008). Omega-3 fats are known to reduce blood levels of triglycerides and therefore are recommended in the control of CVD. These fats also reduce the inflammation process of the body and tend to reduce the clotting time of the blood. A study looking at changes in triglyceride levels with fish consumption found that triglycerides fell almost 30% with intake of fish and almost 40% with both fish consumption and weight loss. Furthermore, one form of HDL-C, HDL2, increased by about 25% (Mori and colleagues, 1999). Fish intake has been found to help prevent worsening of atherosclerosis in women (Erkkila and colleagues, 2004).
Cardiovascular Disease
INTRODUCTION
WHAT ARE THE TYPES AND RISK FACTORS OF CARDIOVASCULAR DISEASE?
ATHEROSCLEROSIS
LIPOPROTEINS
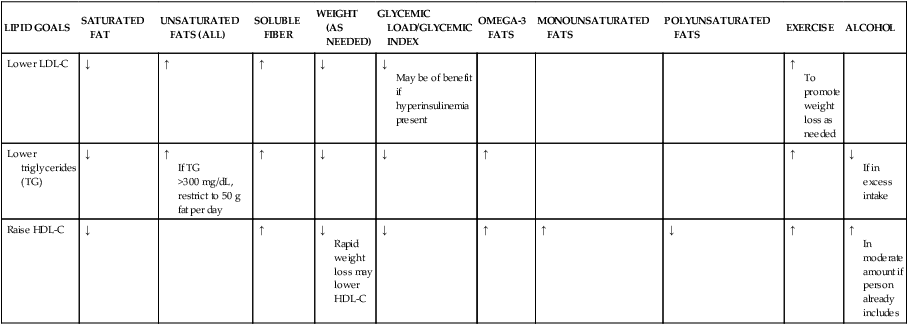
LIPID GOALS
SATURATED FAT
UNSATURATED FATS (ALL)
SOLUBLE FIBER
WEIGHT (AS NEEDED)
GLYCEMIC LOAD/GLYCEMIC INDEX
OMEGA-3 FATS
MONOUNSATURATED FATS
POLYUNSATURATED FATS
EXERCISE
ALCOHOL
Lower LDL-C
↓
↑
↑
↓
↓
May be of benefit if hyperinsulinemia present
↑
To promote weight loss as needed
Lower triglycerides (TG)
↓
↑
If TG >300 mg/dL, restrict to 50 g fat per day
↑
↓
↓
↑
↑
↓
If in excess intake
Raise HDL-C
↓
↑
↓
Rapid weight loss may lower HDL-C
↓
↑
↑
↓
↑
↑
In moderate amount if person already includes
GOALS FOR BLOOD CHOLESTEROL LEVELS
RISK FACTORS FOR CORONARY HEART DISEASE
Oxidation of LDL-C
Metabolic or Insulin Resistance Syndrome and Its Relation to Cardiovascular Disease
Gender Differences in Risk Factors for Cardiovascular Disease
Genetic Reasons
RISK FACTORS AND PREVENTION STRATEGIES FOR STROKES
WHAT IS THE IMPACT OF DIET ON THE PREVENTION AND TREATMENT OF LIPID DISORDERS?
WEIGHT MANAGEMENT
CHOLESTEROL INTAKE
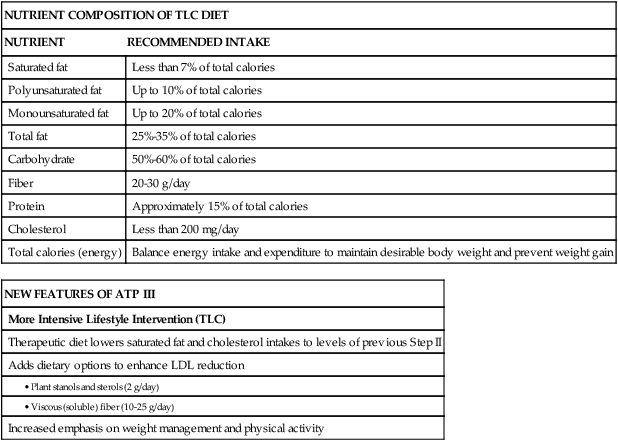
NUTRIENT COMPOSITION OF TLC DIET
NUTRIENT
RECOMMENDED INTAKE
Saturated fat
Less than 7% of total calories
Polyunsaturated fat
Up to 10% of total calories
Monounsaturated fat
Up to 20% of total calories
Total fat
25%-35% of total calories
Carbohydrate
50%-60% of total calories
Fiber
20-30 g/day
Protein
Approximately 15% of total calories
Cholesterol
Less than 200 mg/day
Total calories (energy)
Balance energy intake and expenditure to maintain desirable body weight and prevent weight gain
NEW FEATURES OF ATP III
More Intensive Lifestyle Intervention (TLC)
Therapeutic diet lowers saturated fat and cholesterol intakes to levels of previous Step II
Adds dietary options to enhance LDL reduction
Increased emphasis on weight management and physical activity
DIETARY FATS
SATURATED AND TRANS FATTY ACIDS
UNSATURATED FATS
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Cardiovascular Disease