Cardiovascular Disease
1 University of Texas Southwestern Medical Center, Dallas, TX
2 Jefferson Medical College, Philadelphia, PA
Introduction
According to the National Center for Health Statistics and the American Heart Association (AHA), about one-third of Americans (32 percent) have cardiovascular disease (CVD), accounting for 1 of every 3 deaths in the United States. Approximately 34 percent of the deaths from CVD occurred in people before they reached 75 years of age. Nutrition plays a key role in the prevention and treatment of various types of cardiovascular disease, particularly the most common forms in the American population – coronary heart disease (CHD) and hypertension. Updated 2013 guidelines for assessment of CV risk, lifestyle modifications to reduce CV risk, and management of blood cholesterol, overweight and obesity in adults have been developed by the American College of Cardiology (ACC) and the AHA Task Force on Practice Guidelines. Advising patients to consume a healthy diet, exercise regularly, maintain desired body weight, avoid smoking, and drink alcohol in moderation are critical to reducing CV risk.
Evidence Base for Diet and Heart Disease
Strong evidence indicates that diet, largely through its effect on serum lipids, influences the incidence of heart disease. Intake of saturated fat increases low-density lipoprotein cholesterol (LDL-C) levels, thereby increasing the risk for CHD. Large-scale clinical trials have conclusively shown that reducing serum LDL-C levels reduces the number of acute cardiac events and deaths from CHD both in patients with existing disease and those at risk due to elevated lipids. Angiographic studies have demonstrated that LDL-C reduction slows the progression of atherosclerosis in patients with known disease. Atherosclerosis is now viewed, not simply as the deposition of lipid in the artery, but as a complex inflammatory response to damage to the endothelial lining of arteries.
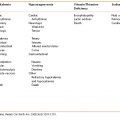
Dietary Lipids
An understanding of the basic biochemistry of fat and fatty acids is needed to address the role of dietary fat in the prevention and treatment of heart disease. Dietary fats are composed chiefly of three fatty acids attached to a glycerol molecule. All fats are a combination of saturated, monounsaturated, and polyunsaturated fatty acids. Fat is the most calorically dense nutrient, supplying 9 calories/g. Therefore, a diet high in fat is generally high in calories. Reducing total fat intake and adhering to an exercise program can help an individual lose weight. A summary of dietary recommendations based on CVD risk factors are summarized in Table 6-1.
Table 6-1 Summary of Lifestyle Recommendations Based on CVD Risk Factors
Source: Lisa Hark, PhD, RD and Fran Burke, MS, RD, 2014. Used with permission.
| Risk Factor | Recommendation |
|---|---|
| Elevated LDL-C | ↓ Saturated fat, ↓ soluble fiber, weight loss, Avoid trans fat |
| Low HDL-C | ↑ Exercise, weight loss |
| Diabetes and insulin resistance | Weight loss, ↓ blood pressure, ↓ carbohydrates, ↑ exercise |
| Elevated triglycerides | ↑ Fish oils, weight loss, ↓ alcohol, ↓ carbohydrates |
| Obesity (BMI >30) | Weight loss, ↑ exercise, ↓ portion sizes |
| Hypertension | ↓ Sodium, ↑ fruits and vegetables, ↓ alcohol, weight loss, ↑ exercise |
| Metabolic syndrome | Weight loss, ↑exercise, customized recommendations for total fat, carbohydrate and calorie intake |
Saturated Fats
Saturated fats are fatty acids with no double bonds. With the exception of palm and coconut oil, foods high in saturated fat are solid at room temperature and are primarily from animal sources.
Major Contributors of Saturated Fat
- Meats/Poultry: brisket, regular ground beef, sausages, hot dogs, sausage, bacon, fatty luncheon meats (pastrami, corned beef, salami, tongue), pâté, spare ribs, lamb, lard, poultry skin, chicken fat, beef fat and fried foods.
- Dairy Products: butter, stick margarine, coffee creamer, whole milk, 2% milk, heavy cream, half-and-half, whipped cream, full-fat yogurt, whole milk cottage and ricotta cheeses, ice cream, hard cheeses, cream cheese, and sour cream.
- Breads/Snacks: potato chips, croissants, butter or sweet rolls, quick breads, and biscuits.
- Desserts/Sweets: donuts, cakes, candy, pies, pastries, and cookies.
The ACC/AHA report suggests that given the current average intake of saturated fat at 11 percent, it would be beneficial to decrease saturated fat intake to 5 to 6 percent of calories for those who need to lower LDL-C levels.
Saturated fatty acids, when contrasted with unsaturated fatty acids, decrease synthesis and activity of LDL-C receptors, promoting an increase in serum LDL-C, thereby contributing to atherogenesis. An increase of 1 mg/dL in serum LDL-C increases CHD risk by 1 percent. A meta-analysis of dietary studies concluded that for every 1 percent increase in calories from saturated fat, serum LDL-C increases approximately 2 percent. Consuming a diet rich in vegetables, fruits, low-fat dairy products, poultry, fish, beans, legumes, nuts, whole grains, and vegetable oils; and limited in sweets, sugar-sweetened beverages, and red meat can help patients lower their saturated fat intake.
Polyunsaturated Fats
Two major categories of polyunsaturated fats (PUFA) are omega-3 and omega-6 fatty acids. Vegetable oils such as corn, canola, sunflower, safflower, cottonseed, peanut, and soybean contain omega-6 fatty acids. Omega-6 fatty acid (linoleic acid), an essential fatty acid, cannot be synthesized by the body and is required in the diet. Arachidonic acid, which is synthesized from linoleic acid, is the major omega-6 fatty acid found in cell membranes and the precursor of prostaglandins. The Dietary Reference Intake for linoleic acid is an Adequate Intake of 17 g/day for men and 12 g/day for women. Substitution of dietary sources of PUFA for saturated fat lowers LDL-C and reduces risk for CHD.
Omega-3 fatty acids include the very long chain eicosapentanoic acid (EPA) and docosahexenoic acid (DHA), as well as the 18-carbon alpha-linolenic acid, another essential fatty acid. The long-chain omega-3 fatty acids decrease serum triglycerides, platelet aggregation, and inflammation, and may therefore provide cardiac benefits. Dietary sources are listed in Appendix M and include canola oil, walnuts, flax seed, chia seeds, salmon, sardines, tuna, and herring. Epidemiologic studies suggest that healthy individuals who consume 7 ounces of fish per week are 30 to 40 percent less likely to die from a cardiac event than those who do not regularly consume fish. The AHA recommends consumption of fish at least twice a week to reduce CVD risk.
In patients with heart disease, some studies indicate a benefit of omega-3 fatty acids. Clinical trials suggest an intake of approximately 1 g/day of EPA/DHA can reduce death from cardiac events. Other studies indicate a trend toward less restenosis after angioplasty for patients receiving omega-3 dietary supplements. Doses of 3 to 4 g/day can be prescribed to lower serum triglyceride in hypertriglyceridemic patients. Although omega-3 fatty acids lower triglycerides, they also slightly increase LDL-C. As research continues, it is appropriate to encourage a dietary pattern that incorporates omega-3 fatty acids, especially from fatty fish, but the benefit of oral supplements is less definitive.
The role of fish oil supplements is more controversial. High doses (3 to 4 g/day) have a definite role in treating hypertriglyceridemia, but the potential for CV benefits and other uses are not clear. One gram of fish oil daily failed to reduce heart disease deaths in an Italian population with multiple CVD risk factors. This dose is low in relation to what might be recommended (1 to 3 g/day) and the population studied already was on a diet higher in monounsaturated fats than the typical United States diet. Therefore, it is difficult to draw firm conclusions about the potential effectiveness of fish oil for CVD prevention from this negative result.
Monounsaturated Fats
Monounsaturated fats (MUFA) contain one double bond; oleic acid is the most common dietary form. Oils high in oleic acid include canola and olive oil. Other dietary sources of MUFA include avocados, almonds, pistachios, peanuts, and pecans. Epidemiologic and clinical evidence from the Mediterranean region, report a lower incidence of CHD when a diet high in MUFA from olive oil is consumed. Shorter-term clinical trials of a Mediterranean style diet have shown improvement in a number of risk factors, including lowering serum triglyceride. Substitution of oleic acid for saturated fatty acids reduces LDL-C levels. A diet high in MUFA lowers LDL-C and serum triglycerides without lowering high-density lipoprotein cholesterol (HDL-C). Provision of some calories from MUFA, which might otherwise be provided from carbohydrate, can lower LDL-C without lowering HDL-C or raising triglyceride levels.
When a reduction in saturated fat intake is recommended to reduce LDL-C, favorable effects on lipid profiles are greater when saturated fat is replaced by polyunsaturated fatty acids, followed by monounsaturated fatty acids, and then carbohydrates. Substitution of saturated fat with whole grains is preferable to refined carbohydrates.
Trans Fatty Acids
Hydrogenation – the addition of hydrogen atoms to an unsaturated fat – can change a fatty acid double bond from a cis to trans configuration. The major source of trans fatty acids is partially hydrogenated vegetable oils found in coffee creamers, canned frosting, microwave popcorn, and some foods served in restaurants. Food manufacturers have used this process to prolong the shelf-life of foods such as crackers, cookies, potato chips, and puddings. Randomized clinical trials indicate that trans fatty acids raise LDL-C levels when compared with naturally occurring cis fatty acids; they also decrease HDL-C levels. The structural similarity of trans fat to saturated fat may explain the detrimental effects. Although margarines contain trans fatty acids, use of a soft or liquid margarine maintains a lower LDL-C than does a comparable diet containing butter (a source of saturated fat and cholesterol). Trans-free tub margarines can be recommended. Recent changes in the formulations of fats used in baked goods and frying oils have reduced the trans fat intake in the United States.
The Institute of Medicine has concluded that there is no safe level for consumption of trans fats and a Food and Drug Administration (FDA) regulation will ban all artificial trans fats from the American food supply. This recommendation aims to save thousands of lives and potentially billions of dollars in medical and economic costs a year. The FDA’s proposal aims to eliminate a loophole that allowed manufacturers to label their products as containing zero grams of trans fats per serving if they contain less than half a gram.
Dietary Cholesterol
Although saturated fat and trans fats are perhaps the major dietary factor responsible for raising serum LDL-C levels, a high intake of cholesterol in the diet can also increase serum LDL-C. Animal foods are sources of cholesterol, with the highest being egg yolk and organ meats. Meat and dairy sources of saturated fat, such as cheese, cream, and fatty meats, also contain substantial amounts of cholesterol.
Hyperlipidemia
Hyperlipidemia, the clinical term used to describe elevated cholesterol, LDL-C, or triglyceride levels, increases the risk of atherosclerosis. An estimated 31.9 million adults 20 years of age and older have total serum cholesterol levels greater than 240 mg/dL, for a prevalence of 13.8 percent. When atherosclerosis proceeds to occlusion or rupture of a blood vessel, myocardial infarction, stroke, or peripheral vascular disease can result (depending upon the affected site). Various lipoproteins transport cholesterol and triglycerides in the blood. The majority of cholesterol is carried in the blood by LDL-C and transported into cells via LDL-C receptors. Low-density lipoproteins are the major atherogenic lipoproteins. In contrast, cholesterol carried by HDL-C represents cholesterol being released by cells. The majority of serum triglyceride is present in very low-density lipoproteins (VLDL). A fasting lipid profile of the patient’s LDL-C, HDL-C, and triglyceride levels is now recommended by the ACC/AHA Guidelines for assessing patient risk of CVD.
Secondary Causes of Hyperlipidemia
Note that hyperlipidemia may also be caused by some underlying “non-lipid” etiology rather than a primary disorder of lipid metabolism. Secondary causes of dyslipidemia include type 2 diabetes mellitus, hypothyroidism, excessive alcohol consumption, cholestatic liver diseases, nephrotic syndrome, chronic renal failure, cigarette smoking, obesity, and certain medications.
Assessment of the Hyperlipidemic Patient
The ACC and AHA collaborated with the National Heart, Lung, and Blood Institute (NHLBI) to develop clinical practice guidelines for assessment of CV risk, lifestyle modifications to reduce CV risk, and strategies for the management of blood cholesterol, overweight and obesity in adults which builds on the Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults – Adult Treatment Panel (ATP).
The clinical approach to the hyperlipidemic patient outlined in the ACC/AHA guidelines is built upon evidence from numerous randomized clinical trials. A heart healthy diet was an underlying principle within these trials. With the goal of reducing atherosclerotic events, moderate or high-intensity statin therapy is prescribed based on an algorithm that considers the patient’s LDL-C level, presence of atherosclerosis and/or diabetes, and in some patients, estimation of 10-year risk. While a heart healthy diet can lower LDL-C by about 10 percent, moderate-intensity statin therapy lowers LDL-C by 30 to 50 percent and high-intensity statin therapy lowers LDL-C by more than 50 percent. The treatment plan is based on an assessment of atherosclerotic cardiovascular disease (ASCVD) risk (defined as first occurrence non-fatal and fatal myocardial infarction (MI), and non-fatal and fatal stroke).
Assessing Risk
The updated guidelines recommend a comprehensive assessment of the estimated 10-year risk for an ASCVD event that includes both CHD and stroke. This is in contrast to the use of an estimated 10-year risk for hard CHD (defined as non-fatal MI and CHD death). This guideline recommends using the new Pooled Cohort Risk Assessment Equations developed by the Risk Assessment Work Group to estimate the 10-year ASCVD risk for the identification of candidates for statin therapy (http://my.americanheart.org/cvriskcalculator). These equations use age, smoking status, total cholesterol, HDL-C, and presence of hypertension and/or diabetes to estimate risk based on race and gender. They can be used to predict stroke as well as CHD events in non-Hispanic Caucasian and African–American women and men aged 40 to 79 years with or without diabetes who have LDL-C levels 70 to 189 mg/dL.
Metabolic Syndrome
Recent attention regarding risk for CHD has focused on a constellation of characteristics termed metabolic syndrome. Metabolic syndrome includes (1) insulin resistance, (2) pre-hypertension, (3) dyslipidemia that can include elevated serum triglycerides, low HDL-C, and small, dense LDL-C, (4) a prothombotic state, and (5) a proinflammatory state. Although measurement of insulin resistance can strengthen the diagnosis of metabolic syndrome, a series of simple measurements shown in Table 6-2 provide a reliable means of clinical identification of individuals at risk for metabolic syndrome. The presence of abdominal obesity is a valuable clue to metabolic syndrome. It can easily be assessed by measuring the patient’s waist circumference, which is described in detail in Chapter 1, Case 1.
Table 6-2 Diagnostic Criteria for Metabolic Syndrome
Source: ACC/AHA Guidelines. 2013. Used with permission.
| 3 or More of the Following 5 Criteria: | |
|---|---|
| Abdominal obesity | Waist circumference: Men > 40 inches Women > 35 inches |
| High blood pressure | BP ≥ 130/≥85 mm Hg or documented use of antihypertensive therapy |
| High fasting blood glucose (FBG) | FBG ≥ 100 mg/dL |
| High triglycerides | ≥ 150 mg/dL |
| Low HDL-C | Men < 40 mg/dL Women < 50 mg/dL |
The increasing prevalence of metabolic syndrome has amplified the importance of nutrition in CHD due to the potential for morbidity and mortality from heart disease. The association of obesity with the development of hypertension, type 2 diabetes, and consequent CVD further heightens the need for all healthcare workers to be educated in the role of nutrition in health promotion and disease prevention.
Medical Nutrition Therapy for Hyperlipidemia and Metabolic Syndrome
Diet and exercise are cornerstones of the effective treatment of hyperlipidemia and metabolic syndrome. The ACC/AHA guidelines for lifestyle modifications to reduce CV risk in adults emphasizes intake of:
- vegetables, fruits, and whole grains,
- low-fat dairy products, poultry, fish, legumes, non-tropical vegetable oils, and nuts,
- limit intake of sweets, sugar-sweetened beverages, and red meats.
The dietary pattern should provide appropriate calories while considering personal and cultural food preferences, and nutrition therapy for other medical conditions (including diabetes mellitus). This pattern can be achieved using the Dietary Approaches to Stop Hypertension (DASH) dietary pattern, the USDA My Plate (www.choosemyplate.gov), or the AHA/Therapeutic Lifestyle Changes Diet. Implementation of any of these patterns should include:
- reduction of percent of calories from saturated fat to 5 to 6 percent,
- reduction in percent of calories from trans fat.
(Dietary patterns that limit saturated fat to 5 to 6 percent of calories, generally provide total fat within the range of 25 to 30 percent of calories.)
Other therapeutic options that may be added for further LDL-C lowering include:
- intake of 2 g of plant stanol/sterol esters per day,
- increasing viscous fiber intake to 10 to 25 g/day.
For patients with hypertriglyceridemia, the proportion of dietary carbohydrate and fat can be shifted such that dietary fat is at the upper end of the allowed range, while calorie intake is adjusted for either weight loss or weight maintenance. Adopting lifestyle changes that incorporate new long-term dietary habits demands an investment of time and family support. Referral to a registered dietitian for medical nutrition therapy allows for a comprehensive assessment of nutritional status, development of negotiated, tailored behavior change goals, and strategies to achieve these goals. The dietitian can assist patients with problem areas such as portion size, eating out, and tips for food purchasing and preparation. Continued reinforcement and monitoring of behavior change by healthcare professionals is important for achieving and maintaining lifestyle changes. Many lipid centers have dietitians on staff who routinely counsel patients and work closely with the healthcare team.
Other Nutritional Components
Stanol/Sterol Esters
Plant sterols and their chemically modified counterpart, plant stanols, have been esterified and incorporated into a growing number of products, such as margarine, yogurt, and orange juice. Consuming 2 tablespoons/day of sterol-fortified spread can provide 2 to 3 g of sterol/stanol esters per day and lower LDL-C levels by 7 to 15 percent. In the gastrointestinal tract, sterol/stanol esters compete with cholesterol for incorporation into micelles and thus absorption. Two possible concerns regarding use of plant sterol/stanol fortified margarines are: (1) caloric adjustment to maintain energy balance if margarine use is increased; (2) adequate intake of fruits and vegetables to compensate for the reduced absorption of dietary carotenoids.
Dietary Fiber
Inclusion of viscous or soluble fiber in the diet can decrease LDL-C levels. Based on evidence from a meta-analysis of over 50 clinical trials, ACC/AHA recommends inclusion of at least 5 to 10 g/day of viscous fiber, with the option of greater intakes in the range of 10 to 25 g/day. The 5 to 10 g/day has been shown to reduce LDL-C by about 5 percent. The hypocholesterolemic effect of soluble fiber results from its ability to form a gel-like substance in the gut, which binds and removes bile acids from the body through the stool before they are reabsorbed. Hepatic conversion of cholesterol into new bile acids reduces serum cholesterol. Total fiber intake is recommended at 25 to 35 g/day. Dietary sources of soluble and total fiber are shown in Table 6-3.
Table 6-3 Food Sources of Soluble and Total Fiber
Source: Wahida Karmally, DrPH, RD, CDE, CLS, FNLA. 2014. Used with permission.
| Food | Soluble Fiber (g) | Total Fiber (g) |
|---|---|---|
| Cereal grains (1/2 c) | ||
| Barley | 1 | 4 |
| Oatmeal | 1 | 2 |
| Oatbran | 1 | 3 |
| Seeds | ||
| Psyllium(1tbs) | 5 | 6 |
| Fruit (1 medium) | ||
| Apple | 1 | 4 |
| Bananas | 1 | 3 |
| Blackberries (1/2 c) | 1 | 4 |
| Pears | 2 | 4 |
| Prunes (1/4 c) | 1.5 | 3 |
| Food | Soluble Fiber (g) | Total Fiber (g) |
| Legumes (1/2 c cooked) | ||
| Black beans | 2 | 5.5 |
| Kidney beans | 3 | 6 |
| Lima beans | 3.5 | 6.5 |
| Lentils | 1 | 8 |
| Black eyed peas | 1 | 5.5 |
| Vegetables (1/2 c) | ||
| Broccoli | 1 | 1.5 |
| Brussel sprouts | 3 | 4.5 |
| Carrots | 1 | 2.5 |
Fruits and Vegetables
The evidence for inclusion of fruits and vegetables is summarized in a meta-analysis that concluded that each additional portion of fruit and vegetable consumed daily decreased the risk of CHD by 4 percent. Generous intake of fruits and vegetables is reflected in the DASH dietary pattern, as well as the Mediterranean diet. Practical advice to the patient is to cover half of the plate with fruits and non-starchy vegetables.
Supplemental Vitamins
Although supplementation with antioxidants and B vitamins was common in the 1990s as a strategy to reduce atherosclerosis, clinical trials did not demonstrate significant benefits. In fact, use of an antioxidant “cocktail” of vitamins C and E, beta-carotene, and selenium actually lowered the beneficial sub-fraction HDL2 cholesterol in patients receiving simvastatin and niacin treatment; it also reduced the stenosis lowering effect of the medical treatment. One meta-analysis of antioxidant supplementation trials reported a slight increase in mortality among subjects receiving vitamin A or E supplements. Beyond use of a daily multivitamin supplement, patients should be encouraged to obtain antioxidants and other vitamins from a diet rich in colorful fruits and vegetables and grains, rather than through supplements. It should be noted that that there is controversy regarding the benefits of even a daily multivitamin supplement.
Medical Nutrition Therapy for CHD (Chapter 6: Case 1)
Nutrition issues should be addressed with patients who have hyperlipidemia, CHD, or a family history of heart disease during most routine primary care visits. Attention to calorie balance is important for most patients primarily for weight control. Fostering control of caloric intake and encouraging increased physical activity are key to promoting weight maintenance and weight reduction. Weight reduction in overweight patients improves parameters associated with metabolic syndrome, including reducing LDL-C and triglycerides, increasing HDL-C, reducing blood pressure, and normalizing elevated serum glucose levels. In many cases, as little as 7 to 10 percent weight reduction alone can eliminate the need for drug therapy in this clinical syndrome.
Conversely, it is possible that the initiation of a lipid-lowering medication prompts patients to feel attention to diet is no longer needed. Failure to follow appropriate diet when drugs are used can limit their effectiveness or necessitate higher doses, increasing the potential for side effects. Therefore, health professionals should continue to emphasize the underlying benefit of a calorically balanced, low saturated fat diet when lipid-lowering drugs are used (Table 6-1).
Alcohol
In addition to the general lifestyle issues of diet and exercise, a specific issue often raised in patient conversations regarding heart disease is the consumption of alcohol. Alcohol, in relation to heart disease, has both positive and negative effects. A first step in advising patients regarding alcohol is to obtain an alcohol intake history. Although light-to-moderate intake of alcohol may reduce the risk of CHD, intake over 30 g/day (more than 2 drinks) is associated with an increased mortality due to hypertension, pancreatitis, hypertriglyceridemia, gastrointestinal malignancies, stroke, cardiomyopathy, cirrhosis, accidents, and breast cancer. Moderate alcohol intake is defined as no more than 2 drinks per day for men and 1 drink per day for women. A drink is defined as 5 ounces of wine, 1.5 ounces of 80-proof liquor, or 12 ounces of beer.
In terms of benefits, alcohol may have cardioprotective effects by increasing HDL-C levels and reducing LDL-C oxidation via the antioxidant polyphenols (catechin, quercetin, resveratrol). A CHD patient can continue to drink alcohol in moderation if free of other medical, psychiatric, or social problems. However, it is not appropriate to recommend alcohol intake to a non-drinker for its cardioprotective effect, as there are many other effective non-pharmacological therapies.
Reversing Heart Disease
The early promise of atherosclerotic plaque regression through intensive lifestyle modification and dietary manipulation does not seem to have been reproduced in subsequent lipid-lowering studies. On the other hand, statin drugs have also been shown to have effects on the vascular endothelium beyond lipid lowering. The potential mechanisms of plaque regression are under active investigation.
Hypertriglyceridemia
Evidence from epidemiological and controlled clinical trials has demonstrated that triglyceride levels are markedly affected by body weight status and body fat distribution. Data from National Health and Nutrition Examination Survey (NHANES) supports a relationship between body mass index (BMI) and triglyceride levels, whereby 80 percent of participants who were overweight and obese had triglyceride levels above 150 mg/dL. The Framingham Heart Study also confirmed this strong association of triglyceride levels with both subcutaneous abdominal adipose tissue and visceral adipose tissue in men and women (mean age 50 years). A consequence of excessive fat combined with impaired clearance or storage of triglycerides in subcutaneous fat is ectopic fat deposition in skeletal muscle, liver, and myocardium, which may result in insulin resistance, non-alcoholic fatty liver disease, and pericardial fat.
Medical Nutrition Therapy for Hypertriglyceridemia
Weight Reduction
There is strong evidence that weight loss, reducing simple carbohydrates at the expense of increasing dietary fiber, eliminating trans fats, restricting fructose and saturated fats, implementing a Mediterranean-style diet, and consuming marine-derived omega-3 PUFA can produce a marked triglyceride-lowering effect ranging between 20 and 50 percent. The AHA recommends 2 to 4 g/day of EPA plus DHA, provided as capsules under a physician’s care, for patients who need to lower their triglyceride level. This recommendation is based on a large body of evidence showing triglyceride-lowering effects of marine-derived omega-3 PUFA.
Dietary practices or factors that are associated with elevated triglyceride levels include excess body weight, especially visceral adiposity; simple carbohydrates, including added sugars and fructose; a high glycemic load; and alcohol. Studies show that multiple dietary interventions can result in additive triglyceride-lowering effects. The magnitude of decrease in triglycerides is directly related to the amount of weight loss. Meta-analyses have reported that for every kilogram of weight loss, triglyceride levels decrease 1.9 percent, or 1.5 mg/dL. A weight loss of 5 to 10 percent results in a 20 percent decrease in triglycerides, a 15 percent reduction in LDL-C, and an 8 to 10 percent increase in HDL-C. The magnitude of decrease in triglycerides is directly related to the amount of weight loss.
Reducing Fat and Carbohydrates
The relationship between percent of total fat intake and change in triglyceride and HDL-C concentrations was reported in a meta-analysis of 19 studies published by the Institute of Medicine. In this analysis comparing low-fat, high-carbohydrate diets versus higher-fat diets, for every 5 percent decrease in total fat, triglyceride level was predicted to increase by 6 percent and HDL-C to decrease by 2.2 percent. Epidemiological and clinical trial evidence suggests that the Mediterranean-style dietary pattern is associated with decreased triglyceride levels. In the Framingham Heart Study Offspring Cohort (n = 2730), subjects in the highest quintile for Mediterranean-style dietary pattern score had the lowest triglyceride levels (103 versus 114 mg/dL) over a 7-year follow-up. In addition, the lowest triglyceride levels were observed when added sugar represented 10 percent of total energy. Conversely, higher triglyceride levels (5 to 10 percent) were observed when added sugar represented a greater proportion of energy intake.
Physical Activity to Reduce the Risk of CVD
Regular physical activity is associated with reduced CVD with an inverse dose response. In essence, higher levels of activity are associated with lower rates of CVD. This reduction in CVD occurs at least in part through the effect of exercise on CV risk factors. The ACC/AHA Guidelines on Lifestyle conclude that both aerobic exercise and resistance training have benefits on the serum lipid profile, as well as decreasing blood pressure. Unfortunately, one-third of Americans report that they do not engage in any aerobic leisure-time physical activity. The ACC/AHA Lifestyle Guidelines advise adults to engage in aerobic physical activity to reduce LDL-C and non-HDL-C for at least 3 to 4 sessions a week, lasting on average 40 minutes per session, and involving moderate-to-vigorous intensity physical activity.
Hypertension (Chapter 6: Case 2)
Approximately 78 million United States adults currently have hypertension, defined as greater than 140/90 mm Hg. This represents 33 percent of United States adults 20 years of age and older. Hypertension affects men and women in nearly equal proportions and African–Americans have among the highest prevalence of hypertension (44 percent) in the world. Hypertension is a major risk factor for the development of CHD, cardiomyopathy, and stroke. National guidelines recommend pharmacological treatment of hypertension based on patient age. For patients older than 60 years, treat medically when systolic blood pressure is greater than 150 mm Hg or diastolic blood pressure greater than 90 mm Hg. For the general population younger than age 60 years, treat when systolic blood pressure is greater than 140 mm Hg or diastolic blood pressure greater than 90 mm Hg. Specific treatment goals vary with patient’s age and diagnosis of kidney disease or diabetes.
Diet and other lifestyle factors have enormous potential for the prevention and treatment of hypertension and in some cases can obviate the need for drug therapy or lower the dose required. This is particularly evident in patients with blood pressure in the range of 120/80 to 130/89 mm Hg. Nutritional factors that may contribute to the development of essential hypertension include obesity, high sodium intake, low potassium and calcium intake, and excessive alcohol consumption. The DASH trial, the subsequent DASH-sodium trials, the PREMIER study, and the 2013 AHA/ACC lifestyle guidelines to reduce cardiovascular risk all have substantiated the benefit of a comprehensive dietary approach in the prevention and treatment of hypertension.
The DASH diet, outlined in Table 6-4, provides for a substantial intake of potassium and calcium through the inclusion of fruits and vegetables and low-fat dairy products. In addition, meat portions are limited and nuts are used to provide magnesium and additional fiber. This rather plant-based diet also limits saturated fat making it appropriate for those needing to lower LDL-C. Based on clinical trials, the DASH diet reduced diastolic blood pressure by as much as 5 mm Hg, regardless of age, gender, ethnicity, or preexisting hypertension. The diet was more effective among African–American and hypertensive individuals. For patients with blood pressure in the range of 140/90 to 159/99 mm Hg, the diet lowered blood pressure similar to the effect of a single-agent anti-hypertensive therapy. Your Guide to Lowering Your Blood Pressure With DASH is available at http://www.nhlbi.nih.gov/health/public/heart/hbp/dash/new_dash.pdf.
Table 6-4 Dietary Approaches to Stop Hypertension (DASH Diet) Recommendations
Source: National Heart, Lung, and Blood Institute. Used with permission.
| Food Group | Daily Servings | Serving Sizes |
|---|---|---|
| Grains and grain products | 7–8 | 1 slice bread 1 cup dry whole grain cereal* ½ cup cooked rice, pasta, or cereal |
| Vegetables | 4–5 | 1 cup raw leafy vegetable ½ cup cooked vegetable 6 ounces low sodium vegetable juice |
| Fruits | 4–5 | 6 ounces fruit juice 1 medium fruit ¼ cup dried fruit ½ cup fresh, frozen, or canned fruit |
| Low-fat or fat-free dairy foods | 2–3 | 8 ounces milk 1 cup yogurt 1½ ounces cheese |
| Meats, poultry, and fish | 2 or less | 3 ounces cooked meats, poultry, or fish |
| Nuts, seeds, and dry beans | 4–5 per week |  cup or 1½ ounces unsalted nuts cup or 1½ ounces unsalted nuts2 Tbsp or ½ ounce unsalted seeds ½ cup cooked dry beans |
| Fats and oils† | 2–3 | 1 tsp soft margarine 1 Tbsp low fat mayonnaise 2 Tbsp light salad dressing 1 tsp vegetable oil |
| Sweets | 5 per week | 1 Tbsp sugar 1 Tbsp jelly or jam ½ ounce jelly beans 8 ounces lemonade |
This DASH eating plan is based on 2000 calories daily. The number of servings may vary from those listed depending on caloric needs.
*Serving sizes may vary between ½ and 1¼ cups.
†Fat content changes serving counts for fats and oils: 1 Tbsp of regular salad dressing equals ½ serving; 1 Tbsp of fat-free dressing equals 0 servings.
1. Following the advice to consume vegetables, fruits, and whole grains, low-fat dairy products, poultry, fish, legumes, non-tropical vegetable oils, and nuts within the DASH dietary pattern provides for reduced sodium intake compared to the average American diet. Patients with hypertension should also be advised to limit alcohol intake and work towards a healthy weight. Limiting sweets and sugar-sweetened beverages assists with weight management. 2. After the original trial, the DASH-sodium trial investigated the effect of the DASH diet combined with three different levels of sodium (3300 mg, 2400 mg, and 1500 mg). Reductions in blood pressure were proportional to the level of sodium restriction.
The high quality evidence from the DASH trials, as well as lower quality evidence of the benefits of the Mediterranean dietary pattern supports the benefit of frequent consumption of fruits and vegetables in reducing both hypertension and atherosclerosis. The benefit in lowering blood pressure has been demonstrated in those with and without hypertension, in men and women, in younger and older individuals, and in both African–Americans and non-African–Americans. This benefit is independent of weight or sodium intake. A wide variety of resources can assist in adaptation to personal and cultural preferences, including use of lacto-ovo vegetarian diets.
Obesity and Hypertension
Obesity is a major risk factor in the development of hypertension. It has been estimated that 60 percent of the hypertensive population are more than 20 percent overweight. A linear relationship exists between the degree of obesity and the severity of hypertension. The beneficial effect of weight reduction in hypertensive individuals has been clearly documented. Controlled dietary intervention trials estimate that a mean reduction in body weight of 20 pounds (9.2 kg) is associated with a 6.3 mm Hg reduction in systolic blood pressure and a 3.1 mm Hg reduction in diastolic blood pressure. The exact mechanism of obesity-induced hypertension is unclear, but increased cardiac output, sodium retention, and increased sympathetic activity in response to elevated insulin levels are all thought to be significant contributors. Weight reduction should be the primary goal for the overweight hypertensive patient, since even a 10 percent change in body weight is sufficient to reduce blood pressure. Therefore, weight management is an important component to control blood pressure.
Lower Dietary Sodium Intake
Population studies have repeatedly demonstrated a relationship of hypertension to higher sodium intakes. Strong evidence from clinical trials consistently indicates that lowering sodium intake reduces blood pressure. This benefit is seen in those with and without hypertension, in African–Americans and non-African–Americans, and across various age groups.
The National High Blood Pressure Education Program, the American Society of Hypertension, and the Dietary Guidelines for Americans set an upper limit of 2300 mg of sodium per day for the general adult population. For high-risk groups including African–Americans, individuals ≥ 51 years of age, and individuals with hypertension, diabetes, or chronic kidney disease, the recommendation is to further limit sodium to 1500 mg per day. The AHA currently encourages of the goal of 1500 mg/day for both hypertensive and healthy adults.
In regard to sodium and blood pressure, the AHA/ACC Lifestyle Guidelines recommend:
- no more than 2400 mg/day of sodium,
- further reduction of sodium intake to 1500 mg/day is encouraged,
- reduction of sodium intake by at least 1000 mg/day (that will lower BP, even if the desired daily sodium intake is not yet achieved),
- combination of lower sodium intake with the DASH dietary pattern.
Reducing sodium intake can be challenging for an individual because of the ubiquitous nature of sodium in the American food supply. The typical American diet contains approximately 4 to 8 g of sodium per day. Table salt and foods high in sodium – such as salted, smoked, canned, and highly processed foods – should be limited. Educational materials with strategies to help patients lower sodium intake are provided by several Federal and private sources. The use of convenience foods, fast foods, and eating out all frequently contribute to higher sodium intakes among Americans. Key questions for patients with hypertension are:
- Do you use a salt shaker at the table or in cooking?
- Do you read labels for sodium content? (recommend <400 mg/serving)
- How often do you eat canned, smoked, frozen, and processed foods?
In addition to individual lifestyle changes, changes in food manufacturing and processing are being implemented to reduce the sodium intake of Americans.
Both a healthy dietary pattern rich in fruits and vegetables and low fat protein sources as exemplified by DASH and a reduced sodium intake independently reduces blood pressure. However, the beneficial effect is even greater when these dietary changes are combined. In the 60 percent of United States adults with blood pressure above 120/80 mm Hg, simultaneously implementing both dietary recommendations can prevent and control HTN more than either intervention alone.
Increase Dietary Potassium Intake
Epidemiologic and observational studies have reported an inverse correlation between potassium intake and blood pressure, especially among African–Americans and individuals consuming a high-sodium diet. More recently, several small intervention studies have shown that potassium supplementation results in a modest hypotensive effect. Although the exact mechanism remains unclear, effects of potassium supplementation include natriuresis, inhibition of renin release, and decreased thromboxane production. For practical purposes, increasing dietary intake of potassium may have a beneficial effect on blood pressure. Foods high in potassium include oranges, orange juice, potatoes (especially with the skins), and bananas. To maintain a high potassium intake, the DASH diet includes 8 to 10 servings of fruits and vegetables daily. Certain diuretic therapy, specifically loop diuretics, frequently induces potassium wasting. Increasing dietary potassium intake in these patients may obviate the need for synthetic potassium supplements, which require close monitoring.
Increase Dietary Calcium Intake
Calcium intake may be lower among hypertensive patients than among normotensive individuals. Increased dietary intake may reduce the incidence of hypertension and calcium supplements may produce a hypotensive effect in some patients. Although dietary calcium has been correlated with blood pressure, calcium supplementation has not been shown to significantly lower blood pressure. On the other hand, the inclusion of low-fat dairy food within the framework of the DASH diet did provide additional blood pressure lowering, as outlined in Tables 6-4 and 6-5, which advise two to three servings per day of fat-free or low-fat dairy food. (See Appendices G and H: Dietary Sources of Calcium.)
Table 6-5 Diet and Lifestyle Interventions to Manage Hypertension
Source: Lisa Hark, PhD, RD and Fran Burke, MS, RD. 2014. Adapted from JNC-7.
| Modification | Recommendations | Systolic Blood Pressure Reduction |
|---|---|---|
| Weight reduction | Maintain healthy body weight (BMI 18.5–24.9) | 5–20 mm Hg for each 10 kg weight loss |
| Adopt DASH eating plan | Consume diet rich in fruits, vegetables, low-fat dairy products and low-saturated fat | 8–14 mm Hg |
| Dietary sodium reduction | Reduce sodium intake to 2300 mg/day | 2–8 mm Hg |
| Increase physical activity | Engage in regular aerobic physical activity such as walking 30 minutes at least 5 days a week | 4–9 mm Hg |
| Moderate alcohol intake | Limit alcohol to no more than 2 drinks/day for men and 1 drink/day for women | 2–4 mm Hg |
Reduce Alcohol Intake
Individuals who drink three or more alcoholic beverages per day account for 5 to 7 percent of those diagnosed with hypertension. Two or more drinks per day can lead to an increase in blood pressure. Although alcohol acts as a vasodilator, chronic alcohol ingestion is associated with increased formation of the vasoconstrictor thromboxane. Chronically increased levels of this prostaglandin metabolite may be partially responsible for the hypertensive effect of chronic alcohol ingestion. In controlled studies, reducing alcohol consumption in this population has been associated with a modest reduction in blood pressure.
Physical Activity Recommendations to Reduce Blood Pressure
As is true for other cardiovascular risk factors, adults with hypertension should engage in three to four aerobic activity sessions a week, lasting on average 40 minutes per session, and involving moderate-to-vigorous intensity physical activity.
Heart Failure
Heart failure (HF), which affects nearly 5 million adults in the United States, is characterized by decreased cardiac output, venous stasis, sodium and fluid retention, and malnutrition. Example of signs and symptom of heart failure include shortness of breath (dyspnea); persistent coughing or wheezing; buildup of excess fluid in body tissues (edema); tiredness, fatigue, decrease in exercise and activity; and lack of appetite or nausea.
Reduced function of the left ventricle and accompanying neuro-hormonal changes promote accumulation of sodium and water and shortness of breath, fatigue, and inactivity result. Attention to medical nutrition therapy in the management of patients with HF is critical. Close monitoring, which includes surveillance by the patient and his or her family, can lead to the detection of changes in body weight or clinical status early enough to allow the patient or a healthcare provider an opportunity to institute treatments that can prevent clinical deterioration.
Causes of Malnutrition in Heart Failure
Cardiac cachexia is the wasting and malnutrition seen in patients with long-standing HF. As myocardial function progressively deteriorates, patients present with the loss of adipose tissue and lean body mass secondary to poor nutritional intake and decreased activity. Upper-body and temporal wasting with lower-extremity edema are the hallmark features of this condition. The proposed mechanisms to explain cardiac cachexia include:
- impaired cellular oxygen supply,
- increased nutrient losses,
- increased nutritional requirements,
- decreased nutritional intake.
Impaired cellular oxygen supply Decreased cardiac output reduces oxygen delivery to cells, resulting in inefficient substrate oxidation and inadequate synthesis of high-energy intermediary metabolites.
Increased nutrient losses Hypoxemia and increased venous pressure causes bowel edema with subsequent fat and protein malabsorption. Decreased synthesis of hepatic bile salts and pancreatic enzymes caused by oxygen deprivation to the liver and pancreas may further contribute to this. Proteinuria, secondary to the reduced renal blood flow, is also a feature of HF.
Increased nutritional requirements Patients with HF have increased nutritional requirements due to a hypermetabolic state caused by the increased work required for breathing, the mechanical work of the heart, and oxygen consumption related to alterations in neuroendocrine activity. If additional calories are not ingested to meet these increased demands, weight loss ensues.
Decreased nutritional intake Factors that may result in an inadequate food intake in patients with HF include one or all of the following:
- hepatomegaly and ascites reduce functional gastric volume causing early satiety,
- dyspnea and fatigue induced by eating,
- unpalatable low-sodium diets,
- anorexia, nausea, or vomiting from medications used to treat CHF.
Medical Nutrition Therapy for Heart Failure
Medical nutrition therapy for patients with HF is aimed at controlling blood pressure, sodium and fluid retention, restoring and maintaining body weight, providing adequate energy, protein, vitamins, and minerals, and repletion of protein stores in patients who have lost lean body mass. Providing practical information about eating a well-balanced diet, high in fruits and vegetables and low in saturated fats is critically important.
Lower Dietary Sodium Intake
Patients with HF retain sodium and fluid and therefore, dietary sodium restriction is a cornerstone of treatment. The level of sodium restriction may be individualized according to the severity of the HF. It is recommended that patients with symptomatic HF reduce dietary sodium intake to 2 to 3 g (2000 to 3000 mg) per day. Fewer research studies are available on the benefit of sodium restriction in heart failure, but based on the available studies and the potential influence on several mechanisms involved in treatment of heart failure, The Academy of Nutrition and Dietetics Evidence Analysis Library recommends restricting sodium intake to 2 g/day. Sodium restriction supports the effectiveness of diuretic agents in achieving negative sodium balance. One-fourth or more of hospital re-admissions for patients with HF are due to non-adherence with dietary sodium advice. Patients need more than to be told “stay away from salt.” They need to be able to state their recommended level of dietary sodium, use values on nutrition labels to guide their intake, and distinguish between very high and high sources of sodium.
A study in an urban heart failure clinic linked knowledge of dietary sodium sources with consumption of fewer high sodium foods. Another report indicated that 1 hour of education before hospital discharge decreased likelihood of re-hospitalization by 35 percent and saved $2,823 per patient. Whether the patient is seen in the acute care or ambulatory setting, referral to a registered dietitian for assessment of their nutritional status and assistance in achieving the skills needed to manage a sodium restricted diet at home is appropriate for cost-effective management of HF. Salt substitutes are available to flavor foods, but many of them substitute potassium for sodium. Patients with renal failure or those taking potassium-sparing diuretics should avoid these products. (See Appendix I: Dietary Sources of High Sodium Foods.)
Lower Fluid Intake
Heart failure associated with dilutional hyponatremia may require restricting fluid intake to 1500 to 2000 mL/day. The fluid may be restricted slightly more in the hospital setting. Some suggest limiting daily fluid intake to an amount equal to the 24-hour urine output volume plus 500 mL. Traditional nutrition assessment parameters, such as actual body weight or weight change, may not accurately reflect nutritional status in HF patients. For example, cardiac cachexia may go undetected if body weight is normal or elevated because of sodium and water retention. In addition, serum protein levels, such as albumin, may be decreased secondary to either malnutrition or artificially as a result of dilution from fluid overload. When HF appears well controlled with no evidence of edema or ascites, along with low serum BNP (B-type natriuretic peptide) levels, increase in weight is more likely dry weight gain.
Adequate Calories and Increased Protein
Daily caloric intake should be adequate to promote weight gain (if needed) in patients with HF. Research indicates HF patients generally need higher calories than a healthy control subject, but research to date has not determined how many calories most HF patients need. Some practitioners estimate dietary calories at 1.5 times the basal energy expenditure. Another set of recommendations suggests 28 to 30 kcal/kg of ideal body weight for weight maintenance and 32 to 35 kcal/kg actual weight for the malnourished patient.
Provision of 1.5 g/kg per day of protein can promote anabolism and achieve positive nitrogen balance in patients with cardiac cachexia. High-protein, high-calorie supplements are often necessary to achieve this level of intake, especially when the patient has a poor appetite. Nutritional supplements, both liquid and pudding forms, are available and provide a high concentration of calories and protein in a relatively small volume. The sodium and fluid content of HF supplements must be considered in the total daily sodium and fluid allowance. Small, frequent meals may help HF patients achieve an adequate dietary intake. Patients who cannot meet their caloric and protein requirements orally may require enteral tube feeding (Chapter 12). Enteral feeding in a HF patient is precarious as it can result in overfeeding, which will aggravate the primary condition. Many patients with heart failure have obesity, which places additional strain on an already compromised heart.
Importance of Daily Weight Monitoring
Sudden weight gain or weight loss can be a sign of heart failure, worsening of the condition, and volume overload. Advise patients and their caregivers to measure body weight on a daily basis at the same time of day with similar clothing. Patients should track their weight and compare it to their “dry” weight without edema.
Other Nutrients and Supplements
Reduced food intake can reduce caloric intake and various nutrient levels. Thiamin deficiency has been noted more frequently among heart failure patients. Daily intake of a multivitamin can improve micronutrient status and reduce the possible detrimental effects of thiamine deficiency on the heart. Although a number of additional supplements have been tested, there is limited evidence of benefit to date. A few small trials have shown improved exercise tolerance and quality of life for heart failure patients receiving coenzyme Q10.
Alcohol Alcohol consumption should be limited in order to maintain blood pressure in target range or avoided if the patient has a history of alcoholic cardiomyopathy.
Smoking Cessation Smoking is considered a modifiable risk factor associated with heart failure; it is appropriate to recommend smoking cessation interventions, such as referral to a Quitline and/or pharmacological therapy.
Case 1 Disorders of Lipid Metabolism
Columbia University, New York, NY
JT is a 52-year-old Hispanic man who consults a new physician for a routine physical examination because his employer has recently changed their health insurance plan. He has not seen a physician for the past 3 years.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree