19. Cardiovascular disease
Katherine E. Paterson, Kenneth C-W. Wong, Hari K. Parthasarathy and Isma Rafiq
LEARNING OBJECTIVES
By the end of this chapter the reader will be able to:
• Understand the pathophysiology of cardiovascular disease (CVD) and the causal role of modifiable risk factors;
• Describe how nutritional interventions may complement medical management of CVD or risk factors;
• Evaluate the effectiveness of nutritional interventions in preventing and managing CVD;
• Implement practical dietetic strategies; and
• Critically appraise the role of omega-3 fatty acids in reducing cardiovascular mortality/morbidity.
Pathophysiology and risk factors
Introduction
Cardiovascular diseases encompass three main conditions: peripheral vascular disease, coronary heart disease and stroke. Whilst cardiovascular disease (CVD) has been the major cause of death and disability in developed countries for many years, its emergence as the major cause of death worldwide is a relatively recent statistic. It is estimated that 3.8 million men and 3.4 million women, worldwide, die each year from coronary heart disease (CHD) together with over five million total deaths from stroke. 1 Regional differences still occur with the highest incidence in countries where the main risk factors of hypertension, high plasma cholesterol, smoking, lack of physical activity and poor diet are prevalent. Whilst the incidence of CHD has declined in many developed countries, where various forms of intervention have been developed, the incidence in many emerging nations has increased dramatically during the past 30 years. For example, in the age range 35 to 75 the incidence has declined by over 40% in men and women in Sweden and the UK and by about 30% in the USA, whilst the incidence in Croatia has increased by over 60% in men and women and by about 40% overall in the Ukraine. 1
CVD remains the major cause of death in the United Kingdom, accounting for about 198,000 deaths a year, with nearly half attributed to CHD and about a quarter from stroke. CVD remains one of the major causes of premature death in both men and women. 2 Like many other developed nations, where various strategies have increased public awareness of the major risk factors, such as smoking, lack of exercise and poor diet, the UK has seen a significant decline in the incidence of CHD in the last ten years. For people under the age of 75, the incidence has declined by 40%. Whilst medical and surgical treatment has made a significant contribution to the improved statistics, it is estimated that some 58% of the mortality decline during the past 30 years is attributable to a reduction in major risk factors. 2 Encouraging though these global figures are, they mask a number of trends related to factors such as age, regional, socioeconomic and ethnic differences. 2
• The decline in the incidence of CHD is less marked in the younger age groups.
• The incidence of CHD remains higher and is declining less rapidly in the UK than in several other developed nations.
• Death rates from CHD are higher in Scotland and Northern England than in the rest of the UK. Premature death rates for men are 65% higher in Scotland than in south-west England and 112% higher for women.
• Premature deaths remain significantly higher in manual than in non-manual workers in both men (50%) and women (73%).
• Ethnic differences show a higher incidence of premature death in men (112%) and women (146%), living in the UK but born in South Asia, whilst for men born in the Caribbean and West Africa, but living in the UK, the incidence is lower than the national average. 3 Government and voluntary agencies have targeted all of the major risk factors for CVD, with particular emphasis on smoking, exercise and diet, with the aim of reducing the incidence of CVD.
The National Service Framework for Coronary Heart Disease set a series of standards to reduce the overall incidence of CHD in the population with a particular emphasis on addressing the regional, socioeconomic and ethnic inequalities outlined above. 4Table 19.1, collated by the British Heart Foundation, summarises the major targets that have been set in England, Scotland and Wales. 2 Despite the unequal decline in the incidence of CHD in the population, the rate of decline in recent years shows that the UK has already achieved many of its 2010 targets.
| aDepartment of Health. Our Healthier Nation. London: Department of Health, 1999. | |
| bDepartment of Health. National Standards, Local Action: Health and Social Care Standards and Planning Framework 2005/06 and 2007/08. London: Department of Health, 2004. | |
| cWelsh Assembly Government (2005). See Chief Medical Officer Wales website http://www.cmo.wales.gov.uk/content/work/health-gain-targets/the-targets-e.htm#chd | |
| dWelsh Assembly Government (2005). See Chief Medical Officer Wales website http://www.cmo.wales.gov.uk/content/work/health-gain-targets/the-targets-e.htm#olderpeople | |
| eScottish Executive (2008). Spending Review 2007, Scottish Government. The Scottish Executive: http://www.scotland.gov.uk/Publications/2007/11/30090722/34 and http://www.scotland.gov.uk/Publications/2007/12/11103453/6 | |
| fNew strategies for CVD in Northern Ireland are currently being developed by the Department of Health, Social Services and Public Safety. | |
| Reprinted from Allender S, Peto V, Scarborough P, Kaur A, Rayner M. Coronary Heart Statistics 2008. London: British Heart Foundation, 2008, with kind permission. Available at: http://www.heartstats.org | |
| Englanda,b | |
| CVD—target | To reduce the death rate from CHD, stroke and related diseases in people under 75 years by at least two-fifths by 2010—saving up to 200,000 lives in total |
| CVD—milestone | To reduce the death rate from CHD, stroke and related diseases in people under 75 years by at least one-quarter by 2005 |
| CVD—inequalities target | To reduce the inequalities gap in death rates from CHD, stroke and related diseases between the fifth of areas with the worst health and deprivation indicators and the population as a whole in people under 75 years by 40% by 2010 |
| Walesc,d | |
| CHD—health outcome target | To reduce CHD mortality in 65–74-year-olds from 600 per 100,000 in 2002 to 400 per 100,000 in 2012 |
| CHD—health inequality target | To improve CHD mortality in all groups and at the same time aim for a more rapid improvement in the most deprived groups |
| Stroke | To reduce stroke mortality in 65–74-year-olds by 20% by 2012 |
| Scotlande | |
| CHD—target | To reduce mortality rates from CHD among people under 75 years by 60% between 1995 and 2010, from the 1995 baseline of 124.6 to 49.8 per 100,000 population (standardised to the European Standard Population) |
| CHD—inequalities target | To reduce the death rate from coronary heart disease (CHD) of those aged under 75 years living in the most deprived 15% of areas in Scotland. Reduce mortality from CHD among the under 75s in deprived areas |
| Stroke—target | To reduce mortality rates from stroke among people under 75 years by 50% between 1995 and 2010, from the 1995 baseline of 37.5 to 18.8 per 100,000 population (standardised to the European Standard Population) |
| Northern Irelandf | |
| No target set | |
The emphasis of this chapter is clearly focused on diet as improvement in cardiovascular health in recent years has involved a series of initiatives to improve nutritional standards in the general population.
Pathogenesis of cardiovascular disease
CVD encompasses a group of diseases affecting the heart and cerebral and peripheral vasculature. The term can refer to any disease affecting these structures but is usually used to refer to those conditions that result from the development of atherosclerosis in the heart, resulting in CHD or ischaemic heart disease (IHD); in the brain, causing a cerebrovascular accident (CVA); or in peripheral blood vessels causing peripheral vascular disease (PVD). The leading cause of death involves the coronary blood vessels, resulting in the development of ischaemic conditions in the heart, which may cause a heart attack or myocardial infarction (MI).
It is widely accepted that atherosclerosis develops as a result of mild endothelial damage, causing an inflammatory response with recruitment of circulating monocytes. Atherogenic lipoproteins such as low density lipoproteins (LDL) then enter the subendothelial space, where they become oxidised. Together with subendothelial monocyte-derived macrophages and T lymphocytes, fatty streaks develop, one of the earliest pathological lesions in atherosclerosis. Oxidised lipids can be taken up by macrophages to form lipid-laden macrophages called ‘foam cells’. These foam cells in turn produce growth factors that promote cell proliferation, especially that of smooth muscle cells. Smooth muscle cells can also migrate from the muscular layers of the vessels (tunica media), ingest lipids and become foam cells themselves. Atherosclerosis occurs when these substances including the collagen secreted by smooth muscle cells, build up in the walls of arteries and form hard lesions called plaques. Besides lipid-laden cells, advanced plaques also contain extracellular cholesterol deposits released from dead cells. Calcified deposits can also develop between the muscular layers and the outer portion of the plaque, a result of intracellular microcalcification of smooth muscle cells and smooth muscle cell death. In addition, a fibrous cap usually forms between the endothelium and this lipid plaque. The overall result of all these processes is an atheromatous fibrolipid plaque, leading to narrowing and stiffening of arteries (though initially coronary arteries will enlarge in response to plaque formation in order to compensate). Note that arterial-associated macrophages can interact with high density lipoprotein (HDL) particles with transfer of cholesterol to the latter; this cholesterol will eventually be taken up by the liver. This is thought to be an important process limiting the progression of atheromatous plaques in peripheral arteries.
Figure 19.1 shows the mechanism for the development of thrombosis on plaques in two stages.
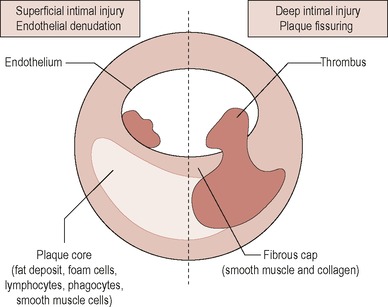 |
| Figure 19.1 • Reproduced from Kumar P and Clark M (eds), Clinical Medicine, 5e, 2002, with permission from Elsevier Ltd |
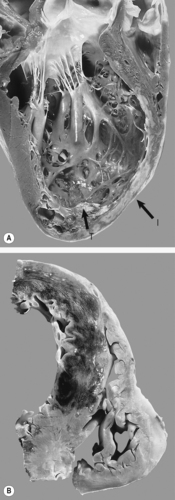
Atheromatous plaques are prone to rupture, leading to exposure of the prothrombotic contents (e.g. subendothelial collagen) of the plaque to circulating blood. Platelets start to aggregate and a thrombus develops, with subsequent partial or complete occlusion of the vessel. Some platelet-derived factors such as thromboxane A 2 can lead to localised vasospasm, which further limits blood flow. Severe limitation of blood flow can lead to an infarction in which the ischaemic conditions can lead to tissue damage and cellular death in the area(s) affected. When this happens in coronary arteries it results myocardial infarction or heart attack. Figure 19.2 shows an acute coronary thrombus.
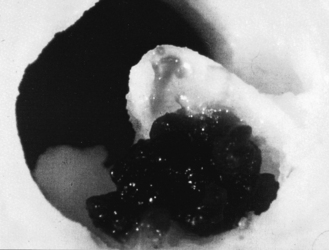 |
| Figure 19.2 • Reproduced from Kumar P and Clark M (eds), Clinical Medicine, 5e, 2002, with permission from Elsevier Ltd. |
Whilst IHD may result from a number of causes, such as coronary artery spasm, vasculitis affecting coronary arteries, severe anaemia or severe trauma, atherosclerosis remains the commonest cause and provides the focus for many of the nutritional targets and interventions detailed in this chapter.
Definitions and symptoms
Stroke may result from haemorrhage, due to the rupture of weakened blood vessels, but is commonly associated with ischaemic conditions resulting directly or indirectly from abnormal thrombotic states, in particular arteriosclerosis.
Stroke is defined by the World Health Organization as a clinical syndrome consisting of rapidly developing clinical signs of focal (or global in case of coma) disturbance of cerebral function lasting more than 24 hours. A transient ischaemic attack (TIA), often referred to as mini stroke, is caused by a temporary disturbance of blood supply to a restricted area of the brain, resulting in brief neurologic dysfunction that persists, by definition, for less than 24 hours. The form taken by a stroke and the symptoms displayed will depend on the blood vessels affected by the underlying event. The sudden onset of face weakness, arm drift and abnormal speech are the most common symptoms displayed. Since the vascular event will usually affect one side of the brain, the symptoms commonly affect one side of the body (please refer to Chapter 20 on Management of Stroke, for further information).
PVD refers to atherosclerosis of arteries supplying the limbs, usually affecting the lower limbs. It is characterised by the development of pain in the muscles of the leg on exertion due to intermittent claudication and in severe cases by pain even at rest. Whilst severe ischaemic conditions can result in gangrene and the need to amputate, there is a far greater risk of the individual developing atheromatous complications resulting in ischaemic heart disease or a stroke if the underlying causes are not addressed.
IHD is a continuum of disorders, from asymptomatic plaques in coronary arteries to full-blown heart attacks or MI.
Stable angina is exertional chest pain that settles readily with rest and/or glyceryl trinitrate spray.
Unstable angina is brought on much more easily and sometimes happens at rest. It also tends to last longer than a typical episode of stable angina attack.
Decubitus angina means angina precipitated by lying flat.
Prinzmetal’s angina is rare and caused by coronary artery spasm; although it is not caused by atherosclerosis, it can certainly coexist with the latter.
Myocardial infarction is a major ischaemic event leading to myocardial damage, and can be subdivided into ST elevation MI and non-ST elevation MI, abbreviated as STEMI and NSTEMI, respectively. ST elevation is where the vessel is blocked completely by a fibrin-rich thrombus (traditional heart attack). A non-ST elevated MI is where the vessel is severely narrowed by a platelet-rich thrombus.
The term acute coronary syndrome (ACS) is an umbrella term that includes unstable angina, NSTEMI and STEMI.
Figure 19.3. shows the different states of the coronary artery vessel wall and the corresponding clinical syndromes. Figure 19.4 shows an angiogram of a STEMI.
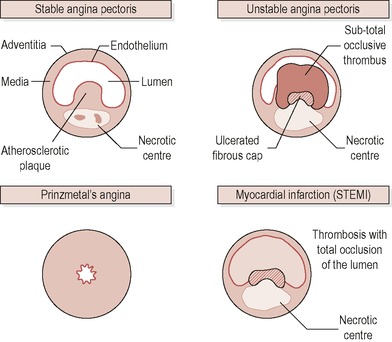 |
| Figure 19.3 • Reproduced from Kumar P and Clark M (eds), Clinical Medicine, 5e, 2002, with permission from Elsevier Ltd. |
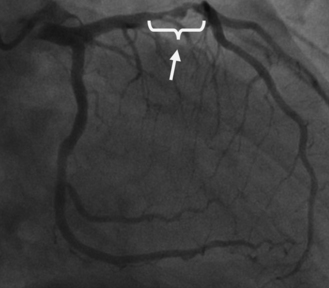 |
| Figure 19.4 • Reproduced with permission from Papworth Hospital NHS Foundation Trust. |
Chronic heart failure (CHF) is a complex syndrome that can result from any structural or functional cardiac disorder that impairs the ability of the heart to function as a pump to support the circulatory system. 5 The incidence has doubled during the past 20 years. One in 6 adults over the age of 85 has CHF and it accounts for over 5% of hospital admissions. IHD is the leading cause of heart failure in the UK, accounting for more than 70% of the incidence. Whilst excessive alcohol intake, hypertension and obesity are significant risk factors and may also contribute to the development of atherosclerosis, strategies to reduce heart failure are aimed predominantly at reducing the risk factors associated with atherosclerosis and IHD. 6
Investigations and diagnosis of CVD
PVD is usually diagnosed on the basis of symptoms displayed. Blood pressure measurements taken in the ankle may provide evidence of vascular occlusion. Imaging techniques are useful if the diagnosis is uncertain or if surgery is required.
The investigation and diagnosis of stroke following the recognition of the signs and symptoms relies on patient history, neurological examination and various imaging techniques. There is no blood test specific to stroke, although blood tests may be useful in establishing the underlying cause (please refer to the chapter on Management of Stroke, for further information).
The diagnosis of an MI usually requires at least two of the three of the following criteria:
• A typical history;
• The establishment of electrocardiogram (ECG) changes; and
• Cardiac enzyme elevation.
An ECG is the first investigation to be done if a chest pain is suspected to be cardiac in origin. The 12 leads on an ECG can indicate which area(s) of the heart, and which coronary artery, is involved in an MI. There are ECG criteria to differentiate between a STEMI and an NSTEMI, for which there are different management strategies.
Troponin T and troponin I are very sensitive and specific markers for myocardial damage. The cardiac troponins T and I are released from damaged cardiac cells within 4–6 hours of an MI and remain elevated for up to 2 weeks. They have nearly complete tissue specificity and are now the preferred markers for assessing myocardial damage. Creatine kinase is also released from heart muscle when it is damaged and may also be used as a marker.
Careful analysis of the changing pattern of released cardiac markers and ECG recordings can provide an accurate assessment of the timing and extent of cardiac damage. Whilst the troponins are also elevated in other conditions, notably pulmonary embolism and renal failure, the pattern of elevation seen following an MI compared to other conditions allows differentiation of the conditions. Figure 19.5 shows the damage to the heart after an MI.
 |
| Figure 19.5 • Reproduced with kind permission of Elsevier Ltd. |
Risk factors for atherosclerosis and cardiovascular disease
As indicated above, atherosclerosis and the development of ischaemic conditions in the circulation and heart remain the overwhelming major cause of CVD and risk factor analysis is focused in this area.
Framingham and risk factors
The Framingham heart study is a longitudinal prospective cohort study originally directed by the National Heart Institute (now the National Heart, Lung and Blood Institute), which started in 1948. 7 Its goal has been to identify risk factors or characteristics which contribute to the development of CVD in a cohort free from CVD at the start of the study. Over 5000 adults between the ages of 30 and 62 from Framingham, Massachusetts, have been reviewed comprehensively and periodically since 1948. Through this surveillance, major CVD risk factors, such as high blood pressure, serum cholesterol levels, smoking, obesity, diabetes and physical inactivity, along with others such as triglyceride level, age, gender and psychosocial factors, have been identified. In 1971 a second generation group was enrolled and in 2002 a third generation.
The epidemiology of CVD is still not fully understood and assessment of risk is inexact, hence the need for ongoing surveillance. An increasing proportion of CVD morbidity in individuals formerly without disease occurs in people over the age of 60. In this case, it is less predictable when new patients will present with CVD. Furthermore, patterns of disease incidence are changing. Alterations in health behaviours relating to nutrition, cigarette smoking and exercise, for example, along with improvements in medical treatment may affect future CVD death and illness rates. 7
Risk factors can be divided into two groups—those that cannot be modified or influenced by or for the individual and those that can.
Non-modifiable risk factors
• Gender: affects males more than females up to the age of 70, as females are thought to be protected by oestrogens until menopause. After the age of 70, males and females have similar incidences;
• Age: the risk increases with age;
• Family history: ACS in a first-degree relative at less than 55 years of age;
• Ethnicity; and
• Previous medical history.
Modifiable risk factors
• Hypertension;
• Dyslipidaemia;
• Smoking;
• Obesity;
• Diabetes and glucose intolerance;
• Fibrinogen;
• Drug abuse;
• Behavioural factors/stress; and
• Physical inactivity.
Hypertension
Blood pressure (BP) has a skewed normal distribution in a population and there is no fixed dividing line between normal blood pressure and blood pressure that is slightly raised. In the population as a whole, the target is to have a blood pressure of 140/85 mmHg (140 systolic and 85 diastolic). In those with diabetes, or disease of the heart and circulation the target is below 130/80 mmHg. 8 The British Hypertension Society suggests that the ideal blood pressure is 120/80 mmHg and normal is less than 130/80 mmHg. 8
Hypertension can occur in the systemic, pulmonary or even portal circulations, although as a term it is usually used to describe high blood pressure in the systemic arteries. Using a threshold of 140/90, about 40% of the UK population have hypertension and the prevalence increases with age. In fact, isolated systolic hypertension affects more than 50% of the over-60 population.
Most cases (around 95%) of hypertension have no known medical cause and are termed essential or primary hypertension and the minority of cases are secondary hypertension.
Secondary hypertension can be due to:
1. Renal disease including intrinsic renal disease (e.g. glomerulonephritis) or renovascular diseases (e.g. secondary to atherosclerosis in renal arteries);
2. Endocrine disorders (e.g. Cushing’s syndrome, Conn’s syndrome);
3. Drugs (e.g. steroids, oral contraceptive pills);
4. Pregnancy; and
5. Rarer causes such as coarctation of aorta.
Hypertension is usually asymptomatic; hence screening is essential. Occasionally symptoms such as headache and blurred vision can occur, especially with malignant hypertension (i.e. a hypertensive emergency with papilloedema and other evidence of target organ damage). BP fluctuates significantly and can even go up only when measured by a healthcare professional, giving rise to the so-called ‘white coat hypertension’. It is crucial to repeat BP measurements and to consider ambulatory BP monitoring, also known as 24-hour BP monitoring, in some cases.
For adults aged between 40 and 69 years, every 20 mmHg rise in typical systolic blood pressure or 10 mmHg rise in diastolic blood pressure doubles the risk of death from IHD. Within the INTERHEART case control study those with hypertension had nearly double the risk of MI. In Western Europe it was estimated that 22% of MIs were due to a history of hypertension. 9 Hypertension is the largest risk factor for stroke. Reducing blood pressure significantly reduces the risk of CVD. In people with diabetes reducing blood pressure in addition reduces the risk of microvascular complications. 10
The classification of blood pressure levels developed by the British Hypertension Society is shown in Table 19.2 and the threshold blood pressures for treatment are shown in Table 19.3. 11
| BP, blood pressure. | ||
| Systolic BP (mmHg) | Diastolic BP (mmHg) | |
|---|---|---|
| Optimal | < 120 | < 180 |
| Normal | < 130 | < 85 |
| High-normal | 139 | 85–89 |
| Hypertension | ||
| Grade 1: Mild | 140–159 | 90–99 |
| Grade 2: Moderate | 160–179 | 100–109 |
| Grade 3: Severe | ≥ 180 | ≥ 110 |
| Isolated systolic hypertension (Grade 1) | 140–159 | < 90 |
| Isolated systolic hypertension (Grade 2) | ≥ 160 | < 90 |
| TC, total cholesterol; LDL-C, low density lipoprotein cholesterol; HDL-C, high density lipoprotein cholesterol; BP, blood pressure. | ||
| aAudit standards for blood pressure and lipids are different: BP < 150/90 mmHg; < 145/80 mmHg for diabetes; TC < 5 mmol/L, LDL < 3 mmol/L, i.e. minimum standard of care. | ||
| bDesirable lipid levels: triglycerides < 1.7 mmol/L; HDL-C > 1 mmol/L (men), > 1.2 mmol/L (women); non-HDL-C < 3 mmol/L (non-HDL-C is total minus HDL-C). | ||
| cIndications for medications and doses of medications for individuals with diabetes mellitus may differ. | ||
| dSimvastatin is the first choice of statin preparation; lower dose or alternative preparation may be indicated if clinical contraindication. | ||
| eNICE recommends replacing saturates with unsaturates. 14 | ||
| fNICE does not routinely recommend plant sterols/stanols or omega 3 supplementation for primary prevention. 14 | ||
| Modified from British Cardiac Society et al8 | ||
| Asymptomatic people at high risk (CVD risk ≥ 20% over 10 years) | People with atherosclerotic cardiovascular disease | |
|---|---|---|
| Blood pressurea | ||
| ≤ 140/85 mmHg | ≤ 130/80 mmHg (includes people with diabetes) | |
| Lipidsa,b | ||
TC < 4 mmol/L (or a 25% reduction) LDL-C < 2 mmol/L (or a 30% reduction) | TC < 4 mmol/L (or a 25% reduction) LDL-C < 2 mmol/L (or a 30% reduction) | |
| Fasting plasma glucose | ||
| ≤ 6 mmol/L | ≤ 6 mmol/L | |
| Pharmacotherapyc | ||
| Antiplatelet drugs | Aspirin 75 mg/day (once BP controlled to audit standard) a | Aspirin 75 mg/day |
| Statinsd | For all persons to meet cholesterol targets | For all persons to meet cholesterol targets |
| ACE inhibitors/all receptor blockers | For persons with heart failure or left ventricular dysfunction. Consider in others with heart disease and normal LV function if BP is not at target | |
| Beta blockers | For all persons post-myocardial infarction | |
| Calcium channel blockers | Consider in persons with heart disease when goal BP is not achieved | |
| Anticoagulants | Consider in persons at high risk of systemic vessel occlusion | |
| Lifestyle | ||
| Smoking habit | Stop smoking | Stop smoking |
| Diete,f | Cardioprotective diet: five portions of fresh fruit and vegetables per day at least Regular consumption of fish and other sources of omega-3 polyunsaturates Total fat intake ≤ 30% total energy • Saturated fat ≤ 10% total energy • Replace saturates with monounsaturates • Dietary cholesterol < 300 mg/day Alcohol: ≤ 14 units per week for women; ≤ 21 units per week for men Salt: ≤ 6 g/day (≤ 100 mmol/2.4 g sodium/day) | |
| Adiposity | Waist circumference Asians: men < 90 cm, women < 80 cm. White Caucasians: men < 102 cm, women < 88 cm; BMI 20–25. | |
| Physical activity | ||
Regular aerobic physical activity for a minimum of ½ hour per day nearly every day e.g. swimming/fast walking. | ||
Dyslipidaemia
Dyslipidaemia refers to an abnormal pattern of lipid levels. A population is thought to be unhealthy when its average plasma cholesterol is greater than 5 mmol/L (LDL > 3 mmol/L). 12 In the UK the average cholesterol level is 5.9 mmol/L. 12 A 1% decrease in total cholesterol is associated with a 3% reduction in IHD risk at a population level. On the other hand, for every 1% decrease in HDL cholesterol there is thought to be a 2–3% increase in the risk of IHD. 13 Some believe that the total cholesterol:HDL cholesterol ratio is a more optimal predictor for CVD risk than LDL cholesterol alone. Experts vary in their opinion as to what constitutes an ideal, desirable or abnormal lipid level. Reference ranges based on the distribution of blood cholesterol levels in a normal population do not reflect ideal levels. It is important to consider the levels in the context of existing CVD or other CVD risk factors (see the section Calculation of Cardiovascular Risk).
The commonly measured lipids in clinical practice include:
• Total cholesterol;
• LDL cholesterol;
• Total cholesterol:HDL ratio;
• HDL cholesterol; and
• Total triglyceride.
Table 19.3 shows target or ‘optimal’ levels for total and LDL cholesterol and desirable values for other lipid fractions recommended by the Joint British Societies. 8 The National Institute of Health and Clinical Excellence (NICE) does not make any targets in primary prevention for total or LDL cholesterol. 14 For secondary prevention the targets are < 4 and < 2 mmol/L for total and LDL cholesterol, respectively. 14 There is evidence that reducing absolute cholesterol from baseline level may help to achieve greater risk reduction than through meeting specific targets alone. For this reason, NICE set no target for total or LDL cholesterol levels post MI. 15 It should be noted that at the time of an ACS, total, LDL cholesterol and HDL cholesterol levels diminish. These decreases generally do not last longer than 6–8 weeks unless there are complications. 8 A lipid profile within 1 day of symptoms presenting can give an acceptable approximation.
There are many different types of primary hyperlipidaemia with different underlying biomolecular defects and different lipid profiles. It is helpful, clinically, to consider this wide spectrum of disorders in terms of whether cholesterol or triglyceride or both are elevated. They are summarised in Table 19.4.
| AD, autosomal dominant; AR, autosomal recessive; DM, diabetes mellitus; TG, triglyceride; LDL, low density lipoprotein; VLDL, very low density lipoprotein; IDL, intermediate density lipoprotein. | |||||||
| Disorder with lipid levels where appropriate | Fredrickson classification | Estimated prevalence in European adults (%) | Molecular defect | Elevated lipoprotein | Total cholesterol | Total triglyceride | Clinical features/comorbidities |
|---|---|---|---|---|---|---|---|
| Familial hyper-cholesterolaemia | IIa | 0.2 (heterozygous) | AD, absent or malfunctioning LDL receptors | LDL | ↑ | Normal | Tendon xanthoma (specific), corneal arcus, xanthelasma |
| Polygenic hyper-cholesterolaemia | IIa | 20–80 | Mechanism unclear | LDL | ↑ | Normal | As above but no tendon xanthoma |
Familial combined hyperlipidaemia/combined Hyperlipidaemia: TG 2–10 mmol/L | IIb | 10+ | AD, mechanism unclear | LDL, VLDL | ↑ | ↑ | Corneal arcus, xanthelasma (Often DM, obesity or hypertension present) |
Familial or sporadic hypertriglyceridaemia TG 2–10 mmol/L | IV | 1 | AD, mechanism unclear | VLDL | Normal | ↑ | Recurrent pancreatitis, eruptive xanthoma, lipaemia retinalis, hepatosplenomegaly (Often secondary to DM, obesity, pancreatitis, alcoholism and/or hypothyroidism) |
Familial hyper-chylomicronaemia TG > 10 mmol/L | I | 0.1 | Deficient lipoprotein lipase or apo C-II | Chylomicrons | Normal | ↑ | Recurrent pancreatitis, eruptive xanthoma, lipaemia retinalis, hepatosplenomegaly |
Remnant particle disease TG 5–20 mmol/L cholesterol typically 7–12 mmol/L | III | 0.02 | AR, defective clearance of remnants at hepatic remnant receptor | Chylomicron remnant, IDL | ↑ | ↑ | Palmar xanthoma, tubero-eruptive xanthoma (Often associated with obesity, hyperuricaemia and DM) |
Type V hyper-lipoproteinaemia TG > 10 mmol/L | V | Rare | Similar mechanism to type I | Chylomicrons, VLDL | ↑ | ↑ | Eruptive xanthoma, lipaemia retinalis, hepatosplenomegaly (may be associated with DM or excessive alcohol intake) |
Elevated lipid levels could also be secondary to or associated with other conditions or factors, which must be excluded before starting patients on lipid-lowering agents. Examples of secondary hyperlipidaemia include:
• Endocrine disorders—hypothyroidism, diabetes mellitus;
• Renal disorders—nephrotic syndrome, renal failure;
• Drugs—e.g. thiazide diuretics, isotretinoin;
• Gastrointestinal disorders—biliary obstruction; and
• Dietary factors—high intakes of saturates are associated with raised total and LDL cholesterol and triglycerides; obesity and diets high in refined carbohydrates, excessive alcohol or energy intake are associated with raised triglycerides.
Figure 19.6 shows the endogenous and exogenous pathways in lipid metabolism. The endogenous pathway handles synthesised lipids, while its counterpart deals with dietary fat.
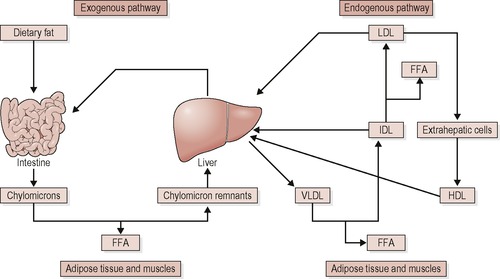 |
| Figure 19.6 • Reproduced with kind permission of Dr Hari Parthasarathy. FFA, free fatty acids; LDL, low density lipoprotein; VLDL, very low density lipoprotein; IDL, intermediate density lipoprotein; HDL, high density lipoprotein. |
Traditionally it was thought that LDL cholesterol was the main culprit in CVD and it is well established that high total cholesterol and/or LDL cholesterol is a risk factor. However, several other lipoproteins are also atherogenic, namely chylomicron remnants, very low density lipoprotein (VLDL), intermediate density lipoprotein (IDL) and small, dense LDL. VLDL and IDL are rich in triglycerides, and this is in keeping with hypertriglyceridaemia being an independent risk factor for IHD. Hypertriglyceridaemia is associated with an elevated VLDL level. In the presence of high VLDL levels, cholesterylester transfer protein (CETP) can facilitate exchange of triglycerides on VLDLs for cholesterol esters on either HDL or LDL. The result is twofold:
1. HDL becomes more readily excreted by the kidneys, resulting in a reduction in HDL cholesterol levels. This explains why there is a strong inverse relationship between triglyceride levels and HDL levels. Note that low HDL levels are associated with an increased risk of IHD.
2. The now triglyceride-rich LDL can undergo further hydrolysis catalysed by various lipases, and the result is a small, dense LDL particle which is highly atherogenic due to its susceptibility to oxidation and its high penetration through endothelial layers. It tends to bypass the usual route of LDL receptor mediated uptake which is an important regulatory mechanism.
This is the biochemical picture seen in the metabolic syndrome X, which is also a risk factor for IHD. Individual risk approaches that of full diabetes and if it is uncontrolled it results in type 2 diabetes and should be managed accordingly. Box 19.1 shows the features of the metabolic syndrome.
 Box 19.1
Box 19.1 Diagnosed if three or more of the features below are present:
• Hypertension (≥ 130/85 mmHg or active treatment for hypertension)
• Central obesity: increased waist circumference ≥ 102 cm in men and ≥ 88 cm in women; ≥ 90 cm for Asian men, ≥ 80 cm Asian women
• Insulin resistance
• Hypertriglyceridaemia (≥ 1.7 mmol/L)
• Low HDL cholesterol (< 1.03 mmol/L for men; < 1.29 mmol/L for women)
• Fasting blood glucose (> 5.6 mmol/L or active treatment for hyperglycaemia)
aDefinition from the American Heart Association and the National Heart, Lung, and Blood Institute.16
Smoking
Cigarette smoking is a major factor in the development of coronary heart disease, stroke and PVD. Smoking is one of the major causes of CVD and smokers are almost twice as likely to have a heart attack as people who have never smoked . It can increase the risk of developing several different types of cancer and is the main cause of some lung diseases. Smoking increases the risk of elevation in fibrinogen and increased blood viscosity. The British doctors cohort study found that mortality from CHD was 50% higher in smokers and over 75% higher in heavy smokers, than in non-smokers. It is estimated that in 2000 around 30,600 deaths or 27% of all smoking attributable deaths were due to CVD. 17
Obesity
Overweight and obesity increase the risk of CHD. As well as being an independent risk factor, obesity is also a major risk factor for high blood pressure, raised blood cholesterol, diabetes and impaired glucose tolerance. 18
The distribution of excess weight is an important factor and the impact is greatest when the fat is concentrated in the abdomen, assessed by the waist-to-hip ratio or waist circumference.
The World Health Organization’s World Health Report 2002 estimated that over 7% of all disease burden in developed countries was caused by raised body mass index (BMI), and that around a third of CHD and ischaemic stroke and almost 60% of hypertensive disease in developed countries were due to being overweight. 19
More recently the INTERHEART case-control study estimated that 63% of heart attacks in Western Europe and 28% of heart attacks in Central and Eastern Europe were due to abdominal obesity, as assessed by a high waist-to-hip ratio and those with abdominal obesity were at over twice the risk of a heart attack compared to those without. 9 This study also found that abdominal obesity was a much more significant risk factor for heart attack than BMI.
Diabetes mellitus and insulin resistance
Diabetes substantially increases the risk of CHD. There are two main types of diabetes: type 1 and type 2 diabetes. Men with non-insulin-dependent diabetes (type 2) have a two- to fourfold greater annual risk of CHD than normal and in women with type 2 diabetes they are at an even higher, three- to fivefold, increased risk. 20 Diabetes not only increases the risk of CHD but also magnifies the effect of other risk factors for CHD such as raised cholesterol levels, raised blood pressure, smoking and obesity.
The recent INTERHEART case-control study estimated that 15% of heart attacks in Western Europe and 9% of heart attacks in Central and Eastern Europe are due to diagnosed diabetes, and that people with diagnosed diabetes are at three times the risk of a heart attack compared to those without. 9
Fibrinogen
Fibrinogen is a strong predictor of CHD, fatal or non-fatal, new or recurrent and of death from an unspecified cause, for both men and women. Its effect is only partially attributable to other coronary risk factors, the most important of which is smoking. 21 Whilst the assessment of cardiovascular risk is usually made on the basis of a number of established risk factors, the suggestion that fibrinogen, C-reactive protein (CRP) and homocysteine should be included in such assessments does not have universal support. For example, a factfile from the British Heart Foundation developed for GPs in February 2007 concludes that there is no clear indication that measuring novel potential risk factors, such as CRP, fibrinogen and homocysteine, is of any value in predicting risk of CHD. Similar conclusions apply to the prediction of CVD risk. However, measurement of homocysteine may be indicated in patients with a demonstrated, strong predisposition to venous and arterial thromboses. 22
Behavioural factors/stress
Inadequate social support, depression (including anxiety), personality (chiefly hostility) and work stress are the four psychosocial factors most often correlated with a raised risk of CHD. 2 More men than women appear to lack social support. The Health Survey for England data, in 2005, show that 18% of men compared with 11% of women reported a severe lack of social support. 23




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


