Pain is the most feared aspect of cancer for most patients and families. For cancer patients, pain often means the cancer is getting worse and death may be imminent. Pain is the most common source of both physical and existential suffering and often leads patients to functional decline, anxiety, depression, and social isolation. These facts are ironic, given the current availability of highly effective drugs and other interventions for pain relief. Ample evidence exists to indicate that cancer pain can be controlled and suffering effectively reduced for almost all cancer patients.
The approach to cancer pain assessment and management is different in elderly versus younger persons. Older persons may underreport pain for a variety of reasons, despite functional impairment, psychological distress, and needless suffering related to pain. They often present with concurrent illnesses and multiple problems making pain evaluation and treatment more difficult. Elderly persons have a higher incidence of side effects to pain medications and a higher potential for complications and adverse events related to many cancer and pain treatment procedures. Despite these challenges, pain can be effectively managed in most elderly patients. Moreover, clinicians have an ethical and moral obligation to prevent needless suffering and provide effective pain relief, especially for those near the end of life.
Physiology of Cancer Pain
Cancer may be nociceptive or neuropathic. Identification of the physiologic process by which pain is perceived may help guide clinicians’ choice of pain management strategies. Treatment aimed at specific pathophysiologic pain mechanisms may be more effective. Nociceptive pain is largely the result of stimulation of somatic or visceral pain receptors. Nociceptive pain may arise from tissue injury, inflammation, or mechanical deformation. Examples include tissue injury by tumor enlargement, organ obstruction, ischemia, inflammation, or injury related to diagnostic or treatment procedures such as surgery. Pain from nociception usually responds well to common analgesic medications, relief of the underlying cause, and tissue healing. Neuropathic pain results from pathophysiologic processes that arise in the peripheral or central nervous system. Examples include tumor pressure or infiltration of nerves, neurotoxicity due to chemotherapy, and posttraumatic neuralgia (after amputation or mechanical nerve injury). Neuropathic pain mechanisms may be identified by association with known disease processes (e.g., postherpetic neuralgia or chemotherapy neurotoxicity), by neuroanatomical location (e.g., a dermatomal pattern), or specific descriptions of the character of the pain. Neuropathic pain may cause a radiculopathy, a pain sensation that travels along a nerve pathway. Common characteristics may include allodynia (a light touch elicits a painful sensation) or hypersensitivity (a painful sensation or pinprick elicits a hyperactive response), as well as descriptions of anesthesia, “pins and needles,” or “like electricity.” In contrast to nociceptive pain, neuropathic pain syndromes have been found to respond frequently to nonconventional analgesic medications such as anticonvulsant and antidepressant drugs. Some pain syndromes are thought to have multiple or unknown pathophysiologic mechanisms for which treatment is more problematic and unpredictable. Examples include fibromyalgia, recurrent headaches, and some vasculitic syndromes.
It is important to remember that all pain perception is modified by individual memory, expectations and emotions. These psychological mechanisms may enhance or diminish pain perception at the cortical level. Pain perception related to a purely psychological mechanism appears to be extremely rare in older people. These disorders akin to conversion reactions are more often related to somatoform disorders where nociceptive or neuropathic pain mechanisms become deeply entwined in psychological and behavioral pathology. Thus the assessment and treatment of pain should always take into consideration the psychological aspects of pain perception, and professional psychological and psychiatric interventions should be included in the multidimensional approach to pain management when appropriate.
Age-related changes in pain perception have been a topic of interest for many years. Elderly persons have been observed to present with painless myocardial infarction and painless intraabdominal catastrophes. The extent to which these observations are attributable to age-related changes in pain perception remains uncertain. Studies of pain sensitivity across the life span have shown mixed results. Decreased pain sensitivity (increased threshold) with aging can be supported by evidence of decreased numbers of receptors and changes in nerve conduction. Increased pain sensitivity (decreased threshold) with aging can also be supported by evidence of alterations in spinal cord and central nervous system processing (poorer endogenous analgesia). If these observations are correct, overall pain perception may not change much with aging. Clearly, additional studies are needed to define age-related changes specific to nervous system function and pain perception.
Assessment and Measurement of Pain in Older Patients
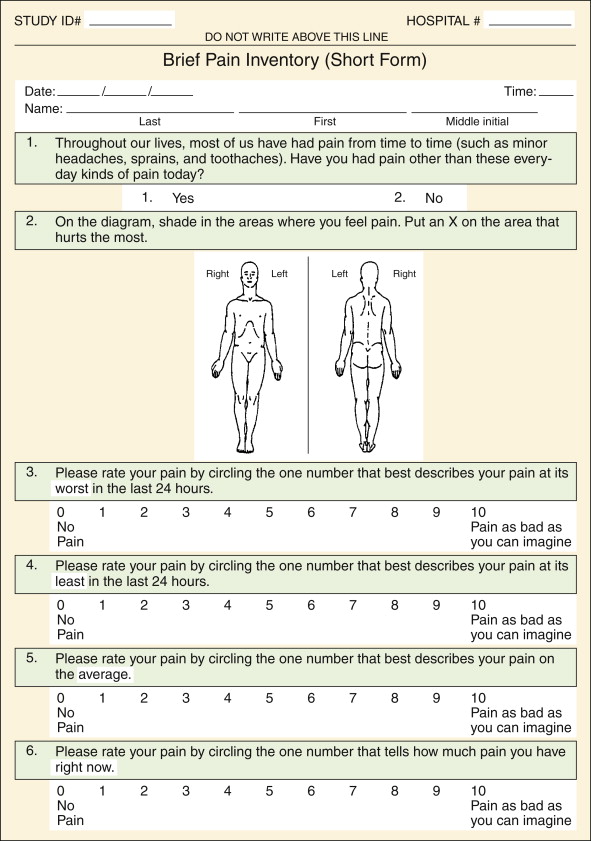
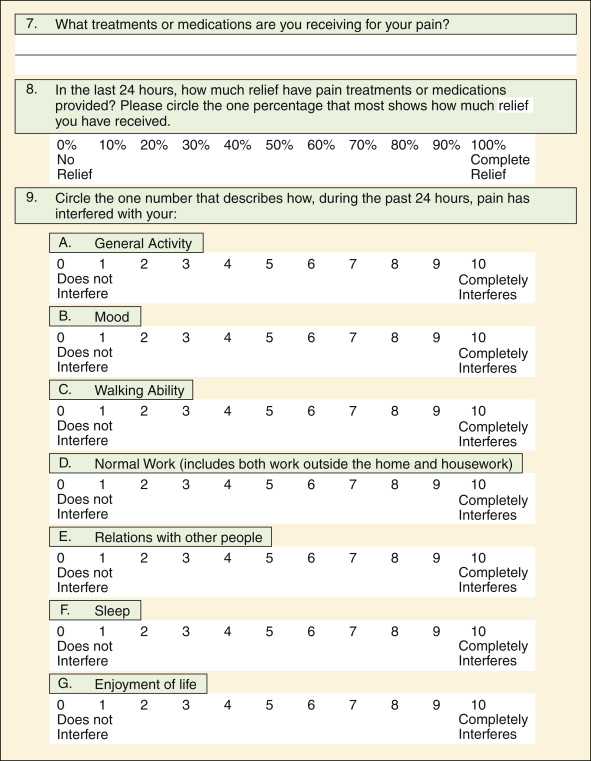
Accurate pain assessment includes an estimate of pain intensity. Pain intensity can be estimated using a valid and reliable pain scale. Pain scales can be grouped into multidimensional and unidimensional scales. In general, multidimensional scales with multiple items often provide more stable measurement and evaluation of pain in several domains. For example, the McGill Pain Questionnaire has been shown to capture pain in terms of intensity, affect, sensation, location, and several other domains that are not possible to evaluate with a single question. The Brief Pain Inventory is a two-dimensional scale that includes intensity and interference with activities. This instrument, originally established for evaluation of cancer pain, has recently been validated in elderly patients, as well as in those with other causes of pain, and has been translated into several foreign languages ( Figure 16-1 ).
Unidimensional scales consist of a single item that usually relates to pain intensity alone. These scales are usually easy to administer and require little time or training to produce reasonably valid and reliable results. Examples include the verbally administered 0 to 10 scale, a single-item visual analog scale, or one of several word descriptor scales that are available. These scales have found widespread use in many clinical settings to monitor treatment effects and for quality assurance indicators. It is important to remember that unidimensional pain scales often require framing the pain question appropriately for maximum reliability. Subjects should be asked about pain in the present tense (here and now). For example the interviewer should frame the question “How much pain are you having right now?” Alternatively the interviewer can ask, “How much pain have you had over the last week?” or “On average, how much pain have you had in the last month?” The latter questions require accurate memory and integration of pain experiences over time that may be more difficult for patients. Recent studies in those with cognitive impairment have shown that pain reports requiring recall are influenced by pain at the moment. Thus it may be more useful to use unidimensional scales to assess pain frequently at the moment while evaluating pain reports over time, much the way vital signs are used. This is especially true for those with some cognitive impairment.
Pain Assessment in Those with Cognitive Impairment
Cognitive impairment, Alzheimer disease, stroke, or dementia can present substantial challenges to pain assessment. Fortunately, it has been shown that pain reports from those with mild to moderate cognitive impairment are no less valid than other patients with normal cognitive function. Weiner and associates have shown that these reports are usually reliable (stable over time) as well. Experience has shown that commonly available instruments are feasible for use in most patients with cognitive impairment. Thus most elderly patients with mild to moderate cognitive impairment appear to have the capacity to report pain accurately and reliably using commonly available methods.
Patients with severe cognitive impairment may represent substantial challenges for which no generalizable methods for pain assessment have been identified. Although it has been assumed that those in deep coma do not experience pain, it is not clear that such brain damage necessarily results in complete anesthesia. Patients with “locked-in syndrome” (having intact perception and cognitive function but no purposeful motor function and no means of communication) may suffer severely. Unfortunately no reliable methods exist to assess pain in these individuals. Health care providers must be aware of these situations and provide analgesia empirically, especially during procedures or for conditions known to be uncomfortable or painful. More often, most of those with severe cognitive impairment can and do make their needs known in simple yes or no answers communicated in various ways. For example, those with profound aphasia can often provide accurate and reliable answers to yes and no questions when confronted by a sensitive and skilled interviewer. For these patients it is important to be creative in establishing communication methods for the purpose of pain assessment.
Although pain is an individual experience, the use of family and caregivers in the assessment of pain can sometimes be helpful. Among patients with cognitive impairment, the history is often only obtainable from family or close caregivers. Family and caregivers are an excellent source of qualitative information about general behavior, medication usage, actions that seem to reduce pain, and actions that seem to aggravate pain. It is important to remember, however, that family and caregivers are limited in their interpretation of events and behaviors. In fact, evidence has suggested that when it comes to estimating pain intensity, proxies are not always very accurate or reliable. Our studies of elderly cancer patients suggest that caregivers may overestimate pain intensity and distress. It is often distressing to family and other caregivers who feel helpless in managing severe pain. Both physicians and nurses have been found to underestimate pain and to provide inadequate pain medication. In the final analysis, family and close caregivers can be valuable sources of qualitative information, but they probably should not be relied on entirely for quantitative assessment of pain intensity or distress, especially among those patients able to communicate their pain experiences.
Pain Assessment in Those with Cognitive Impairment
Cognitive impairment, Alzheimer disease, stroke, or dementia can present substantial challenges to pain assessment. Fortunately, it has been shown that pain reports from those with mild to moderate cognitive impairment are no less valid than other patients with normal cognitive function. Weiner and associates have shown that these reports are usually reliable (stable over time) as well. Experience has shown that commonly available instruments are feasible for use in most patients with cognitive impairment. Thus most elderly patients with mild to moderate cognitive impairment appear to have the capacity to report pain accurately and reliably using commonly available methods.
Patients with severe cognitive impairment may represent substantial challenges for which no generalizable methods for pain assessment have been identified. Although it has been assumed that those in deep coma do not experience pain, it is not clear that such brain damage necessarily results in complete anesthesia. Patients with “locked-in syndrome” (having intact perception and cognitive function but no purposeful motor function and no means of communication) may suffer severely. Unfortunately no reliable methods exist to assess pain in these individuals. Health care providers must be aware of these situations and provide analgesia empirically, especially during procedures or for conditions known to be uncomfortable or painful. More often, most of those with severe cognitive impairment can and do make their needs known in simple yes or no answers communicated in various ways. For example, those with profound aphasia can often provide accurate and reliable answers to yes and no questions when confronted by a sensitive and skilled interviewer. For these patients it is important to be creative in establishing communication methods for the purpose of pain assessment.
Although pain is an individual experience, the use of family and caregivers in the assessment of pain can sometimes be helpful. Among patients with cognitive impairment, the history is often only obtainable from family or close caregivers. Family and caregivers are an excellent source of qualitative information about general behavior, medication usage, actions that seem to reduce pain, and actions that seem to aggravate pain. It is important to remember, however, that family and caregivers are limited in their interpretation of events and behaviors. In fact, evidence has suggested that when it comes to estimating pain intensity, proxies are not always very accurate or reliable. Our studies of elderly cancer patients suggest that caregivers may overestimate pain intensity and distress. It is often distressing to family and other caregivers who feel helpless in managing severe pain. Both physicians and nurses have been found to underestimate pain and to provide inadequate pain medication. In the final analysis, family and close caregivers can be valuable sources of qualitative information, but they probably should not be relied on entirely for quantitative assessment of pain intensity or distress, especially among those patients able to communicate their pain experiences.
Management of Cancer Pain
A variety of both drug and nondrug methods are available and effective in cancer pain management. Data clearly shows that patients benefit most from a multimodal approach incorporating both drug and nondrug strategies along with requisite patient and caregiver education, follow-up, and support. Patients should be given an expectation of pain relief, but it may be unrealistic to suggest or sustain an expectation of complete relief for some patients with persistent pain. The goals and trade-offs of possible therapies need to be discussed openly. Sometimes a period of trial and error should be anticipated when new medications are initiated and titration occurs. Review of medications, doses, use patterns, efficacy, and adverse effects should be a regular process of care. Ineffective drugs should be tapered and discontinued. Patients and caregivers benefit from the empowerment often associated with “patient-controlled analgesia;” encouragement in the use of physical methods such as heat, cold, massage, and distraction; and the use of other cognitive behavioral techniques. Patient and caregiver education and instruction for these “self-help” interventions should be a part of the pain management plan for every patient with serious pain.
Analgesic Drugs for Cancer Pain
Any patient who has pain that impairs functional status or quality of life is a candidate for analgesic drug therapy. Analgesic medications are safe and effective in elderly people. All analgesic interventions carry a balance of benefits and burdens. For some classes of pain-relieving medications (opioids, for example) elderly patients have been shown to have increased analgesic sensitivity. However, elderly people are a heterogeneous population, thus optimum dosage and known side effects are difficult to predict. Recommendations for age-adjusted dosing are not available for most analgesics. In reality, dosing for most patients requires beginning with low doses with careful upward titration, including frequent reassessment for dosage adjustments and optimum pain relief.
The use of placebos is unethical in clinical practice and there is no place for their use in the management of acute or chronic pain. Placebos, in the form of inert oral medications, sham injections, or other fraudulent procedures are only justified in certain research designs where patients have given informed consent and understand that they may be receiving a placebo as a part of the research design. In research, placebos help identify and measure random or uncontrollable events that may confound results of some research designs. In clinical settings, placebo effects are common, but they are neither diagnostic of pain nor indicative of a therapeutic response. The effects of placebos are short-lived and most patients eventually learn the truth, resulting in loss of patient trust and more needless suffering.
Acetaminophen
Acetaminophen is the drug of choice for elderly persons with mild to moderate pain, especially that of osteoarthritis and other musculoskeletal problems. As an analgesic and antipyretic, acetaminophen acts in the central nervous system to reduce pain perception. Despite the lack of anti-inflammatory activity, studies have shown that acetaminophen is as effective as most nonsteroidal anti-inflammatory drugs (NSAIDs). Given in a dose of 650 mg to 1000 mg four times a day, it remains the safest analgesic medication for most patients compared to traditional NSAIDs and other analgesic drugs. Unfortunately, acetaminophen overdose can result in irreversible hepatic necrosis. Therefore, the maximum daily dose should never exceed 4,000 mg per day. Some authors have suggested that the maximum dose of acetaminophen should be reduced in hepatic insufficiency. Unfortunately, evidence to identify a level of hepatic impairment justifying a dose adjustment has not been validated.
Nonsteroidal Anti-Inflammatory Drugs
Nonsteroidal anti-inflammatory drugs (NSAIDs) have analgesic activity both peripherally and centrally. They are potent inhibitors of cyclooxygenase and prostaglandin synthesis that have effects on inflammation, pain receptors, and nerve conduction and may have central effects as well. Clinical trials have found no advantage of COX-2–specific inhibitors compared to traditional nonspecific COX-inhibiting NSAIDs in terms of peak pain relief, total pain relief, and in indices of joint inflammation in patients with arthritis. Safety profiles of these agents have been impressive in reduction of gastrointestinal injury, renal toxicity, and bleeding diathesis, but concerns about a higher risk of cardiovascular events have reduced their overall appeal. Moreover, COX-2–specific inhibitor NSAIDs appear to have similar problems compared with traditional NSAIDs with respect to the incidence of both drug-drug and drug-disease interactions.
NSAIDs are appropriate for short-term use in inflammatory conditions such as gout, calcium pyrophosphate arthropathy, acute flare-ups of rheumatoid arthritis, and other inflammatory rheumatic conditions. They have also been reported to relieve the pain of headache, menstrual cramps, and other mild to moderate pain syndromes. Individual drugs in this class vary widely with respect to anti-inflammatory activity, potency, analgesic properties, metabolism, excretion, and side-effect profiles. Moreover, it has been observed that failure of response to one NSAID may not predict the response to another. A disadvantage of NSAIDs is that they all demonstrate a ceiling effect, that is, a level at which increased dose results in no further increase in analgesia. A large number of NSAIDs are now available; however, there is no evidence to support a particular compound as the NSAID of choice. Several are available over-the-counter without a prescription.
Use of high-dose NSAIDs for long periods of time should be avoided in elderly patients. The concomitant use of misoprostol, histamine-2 receptor antagonists, proton pump inhibitors, and antacids is only partially successful at reducing the risk of significant gastrointestinal bleeding associated with NSAID use. Also, the side-effect profiles of gastroprotective drugs in this population must be weighed against their limited benefits. For those with multiple medical problems, NSAIDs are associated with an increased risk of drug-drug and drug-disease interactions. NSAIDs may interact with antihypertensive therapy. Thus, the relative risks and benefits of NSAIDs must be weighed carefully against other available treatments for older patients with chronic pain problems. For some patients, chronic opioid therapy, low-dose or intermittent corticosteroid therapy, or many other nonopioid analgesic drug strategies may have fewer life-threatening risks compared to long-term, high-dose NSAID use.
Opioid Analgesic Medications
Opioid analgesic medications act by blocking receptors in the central nervous system (brain and spinal cord) resulting in a decreased perception of pain. Selected opioid analgesic medications are listed in Table 16-1 . Opioid drugs have no ceiling to their analgesic effects and have been shown to relieve all types of pain. Short-term studies have suggested that elderly people, compared to younger people, may be more sensitive to the pain-relieving properties of these drugs. This has been shown for acute postoperative pain and chronic cancer pain. Advanced age is associated with a prolonged half-life and prolonged pharmacokinetics of opioid drugs. Thus, elderly people may achieve pain relief from smaller doses of opiate drugs than younger people.
| Drug | Starting Dose (Oral) | Description | Comments |
|---|---|---|---|
| Morphine (Roxanol, MSIR) | 30 mg (q4h dosing) | Short-intermediate half-life; older people are more sensitive than younger people to side effects | Titrate to comfort; continuous use for continuous pain; intermittent use for episodic pain; anticipate and prevent side effects |
| Sustained-release morphine (MS Contin, Oramorph, Avinza) |
| Morphine sulfate in a wax matrix tablet or sprinkles; MS Contin and Oramorph should not be broken or crushed; Avinza capsules can be opened and sprinkled on food, but should not be crushed | Titrate dose slowly because of drug accumulation; rarely requires more frequent dosing than recommended on package insert; immediate release opioid analgesic often necessary for breakthrough pain |
| Codeine (plain codeine, Tylenol #3, other combinations with acetaminophen or NSAIDs) | 30-60 mg (q 4-6 h dosing) | Acetaminophen or NSAIDs limit dose; constipation is a major issue | Begin bowel program early; do not exceed maximum dose for acetaminophen or NSAIDs |
| Hydrocodone (Vicodin, Lortab, others) | 5-10 mg (q 3-4 h dosing) | Toxicity similar to morphine; acetaminophen or NSAID combinations limit maximum dose | Same as codeine |
| Oxycodone (Roxicodone, OxyIR; or in combinations with acetaminophen or NSAIDs such as Percocet, Tylox, Percodan, others) | 20-30 mg (q 3-4 h dosing) | Toxicity similar to morphine; acetaminophen or NSAID combinations limit maximum dose; oxycodone is available generically as a single agent | Same as morphine |
| Sustained-release oxycodone (OxyContin) | 15-30 mg (q 12 h dosing) | Similar to sustained-release morphine | Similar to sustained-release morphine |
| Hydromorphone (Dilaudid) | 4 mg (q 3-4 h dosing) | Half-life may be shorter than morphine; toxicity similar to morphine | Similar to morphine |
| Methadone (Dolophine) | Equal analgesic potency is dose-dependent and difficult to predict; significant overdose risk when switching from other opioids | Serum half-life 18 hr; analgesic half-life 8-12 hr. Highly lipid soluble; metabolism by oxidation and dependent on liver cytochrome enzyme activity. | Black box warning: Significant risk of drug accumulation. |
|
| Slightly more potent than morphine, not as potent as hydromorphone | Same as morphine |
| Transdermal fentanyl (Duragesic) | 25 μg patch (q 72 h dosing) | Reservoir for drug is in the skin, not in the patch; equivalent dose compared to other opioids is not very predictable (see package insert); effective activity may exceed 72 hrs in older patients | Drug reservoir is in skin, not patch. Titrate slowly using immediate release analgesics for breakthrough pain; peak effect of first dose may take 18-24 h; not recommended for opioid-naive patients |
| Fentanyl lozenge on an applicator stick | Rub on buccal mucosa until analgesia occurs, then discard | Short half-life; useful for acute and breakthrough pain when oral route is not possible | Absorbed via buccal mucosa, not effective orally |
∗ A limited number of examples is provided. For comprehensive lists of other available opioids, clinicians should consult other sources.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


