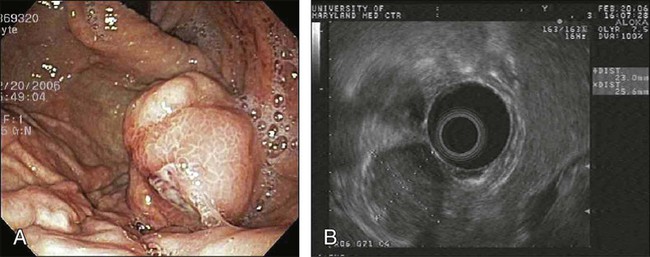
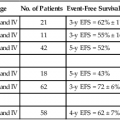
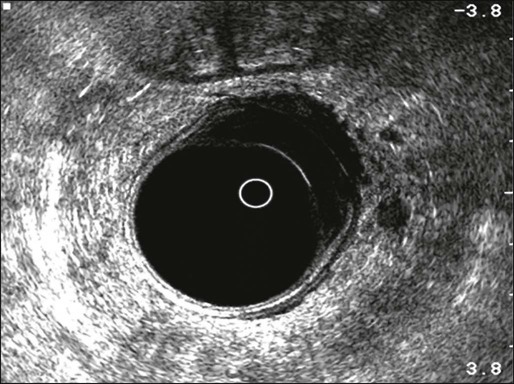
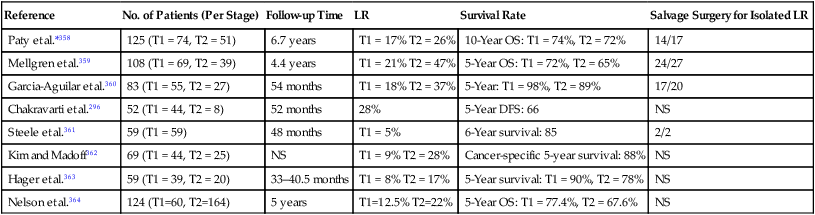
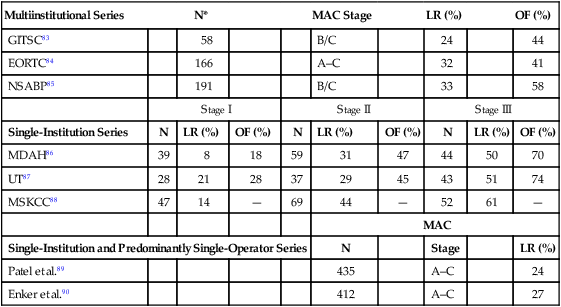
78 Elin R. Sigurdson, Al B. Benson, III and Bruce Minsky • Approximately 40,000 new cases of rectal cancer are diagnosed in the United States annually. • Since 1998, the incidence rate has been decreasing by 2% to 3% per year. • The peak incidence of rectal cancer is during the fifth decade of life. • Aspirin and nonsteroidal antiinflammatory drugs have been shown to be effective in the chemoprevention of colorectal cancer by decreasing the risk of adenoma formation as well as the incidence and mortality of colorectal cancer. Numerous clinical features suggest the presence of rectal cancer, including: • Located approximately 12 cm from the anal verge • Rectal bleeding, often bright red and on the surface of the stool • Subtle changes in bowel habits • Decreased caliber of stool; mucus in stool • Sensation of fullness and tenesmus • Increased straining during defecation • Synchronous colon cancer (in 2% to 9% of patients with rectal cancer) • Careful rectal examination yields 67% to 84% accuracy in staging (superficial, mobile, tethered, fixed) and should include pelvic examination for women and prostate examination in men. • Rigid proctosigmoidoscopy provides the most accurate assessment of distance, size, and position, as well as tethering to surrounding structures. • Colonoscopy, colonography, or double-contrast barium enema is used to assess for synchronous colon tumors. • Endorectal ultrasound can assess the depth of invasion and nodal status. Nodal assessment is less reliable. • Magnetic resonance imaging (MRI) with endorectal coil and ultrasound are useful to stage rectal cancer and are more sensitive and specific than computed tomography (CT) alone. MRI is used to assess locally advanced or recurrent local disease. CT should be performed on all patients to assess intraabdominal spread. CT or chest x-ray is required to evaluate for synchronous lung metastases. • The liver is the most frequent site of distant spread, followed by lung, retroperitoneum, ovary, and peritoneal cavity. • Baseline carcinoembryonic antigen (CEA) levels are assessed and followed postoperatively, even if initially normal. Differential diagnosis includes: • Gastrointestinal stromal tumors • Embryonic tumors (teratomas, chondromas, meningoceles) • Sacral and presacral tumors (neurogenic tumors, liposarcomas, neurofibromatosis) • Goals of treatment are cure, local control, and quality of life. • All retrorectal tumors should be resected, and preoperative biopsy must be avoided. • Full-thickness local excision is feasible for highly selected patients with T1 mucosal, submucosal, and early invasive cancer, particularly in patients with high-risk comorbidities. • For T1 to T3 rectal adenocarcinomas, surgical procedures are total mesorectal excision, low anterior resection, low colorectal or coloanal anastomosis with J pouch, and abdominoperineal resection, leaving at least a 2-cm distal margin and clear lateral margins. With surgery, mortality rates are 1% to 7% and morbidity rates are 13% to 46%. The survival rate at 5 years is 74% to 87%. • Combined therapy cures 50% of N1 patients; 25% of tethered or fixed rectal cancers treated by neoadjuvant chemoradiotherapy are subsequently resected and cured. • Of patients who die of rectal cancer, 25% fail with pelvic disease only. Approximately 40,000 individuals in the United States were diagnosed with rectal cancer in 2012.1 From 1998 through 2006, the incidence rate decreased by 3% per year for men and 2.2% per year for women. Although the incidence rate rises dramatically during the fifth decade of life, the age-adjusted colorectal cancer incidence rates for 1997 to 2006 declined among those age 50 years and older but increased among those younger than 50 years of age.2 Colorectal cancer is the second leading cause of cancer deaths. African Americans are less likely than whites to be diagnosed at a localized stage and have a higher mortality rate than whites for both rectal and colon cancers. In a 32-year period, 1975 to 2007, the gap between the survival rates of African Americans and whites increased from a difference of 6% to 12% for colon cancer and from 3% to 8% for rectal cancer. However, for both colon and rectal cancers, 5-year relative survival rates have significantly increased among all races between 1975 and 1977 and 1999 and 2006.1 Sharpe and colleagues reported an observational study that showed a positive association between cigar smoking and cancer of the rectum. They also noted a weak positive association between cigarette smoking and cancer of the proximal colon.3 Several large cohort studies have shown that cigarette smoking is an independent risk factor for colorectal cancer.4–9 In a large cohort study of more than 22,000 healthy male physicians ages 40 to 84 years who were followed up for more than 12 years, cigarette smoking was an independent risk factor for colorectal cancer incidence, the strongest risk being observed in current smokers of 20 cigarettes or more per day (relative risk: 2.14). Cumulative lifetime exposure and exposure during various periods of life also increased the risk of colorectal cancer.10 One study showed that the increased risk of colorectal cancer associated with cigarette smoking is dependent on the molecular characteristics of the tumor as defined by APC mutation and hMLH1 expression status. The association between frequency of cigarette smoking (for a 5 cigarette/day increment) and colorectal cancer was most apparent and stronger in tumors without a truncating APC mutation, whereas duration of smoking was associated with increased risk in hMLH1-deficient tumors.11 Conversely, aspirin and nonsteroidal antiinflammatory drugs have been shown to be effective in the chemoprevention of colorectal cancer by decreasing the risk of adenoma formation as well as the incidence and mortality of colorectal cancer. Trials have shown that daily aspirin reduces the risk of recurrent colorectal adenoma by 17% to 21% and advanced adenoma by 28%, and that daily aspirin for 5 years reduces incidence and mortality associated with colorectal cancer by 30% to 40% after 20 years of follow-up, and reduces the 20-year risk of all-cause cancer mortality by approximately 20%. Recent evidence also shows that the risk of major bleeding on aspirin diminishes with prolonged use, suggesting that the balance of risk and benefit favors the use of daily aspirin in primary prevention of colorectal and other cancers. In the general population, a significant 26% reduction in colorectal cancer incidence was demonstrated in studies with a 23-year follow-up. In individuals with a history of adenomas, nonsteroidal antiinflammatory drug use was associated with a statistically significant 55% reduction in advanced adenoma incidence and 34% reduction in adenoma recurrence risk.12 Aspirin and celecoxib may be effective in preventing adenomas in patients after polypectomy.13 The importance of a detailed history and a thorough physical examination cannot be overstressed. Comorbid conditions and the patient’s physical habitus may preclude major surgery and influence the decision of adjuvant therapy. Physical examination should always include a digital rectal examination to feel for a mass, assess its location and mobility, and feel for enlarged extrarectal lymph nodes (50% accuracy). Depth of invasion and whether the tumor is tethered or fixed can also be assessed during rectal examination with 67% to 84% accuracy.14,15 A careful pelvic examination in women and a prostate assessment in men are essential. A rigid proctosigmoidoscopic examination of the rectum and the anus should follow. The distance of the tumor from the anal verge, anterior/posterior/lateral position, size, morphologic configuration, and extent of circumferential involvement are determined. Tumor mobility and tethering to surrounding structures are ascertained. If not obstructed, patients with rectal cancer should have a preoperative double-contrast barium enema or preferably a colonoscopy to assess for synchronous colon cancer (2% to 9%). Subjective and objective assessment of the patient’s anal sphincter function is desirable. A weak or incompetent sphincter may indicate the need for a colostomy. Endorectal ultrasound provides valuable preoperative staging (Fig. 78-1), including depth of tumor invasion into the rectal wall (89% to 92% accuracy,16,17 96% sensitivity, 90% specificity, 96% negative predictive value18) and nodal enlargement (79% sensitivity, 74% positive predictive value, 84% negative predictive value19), but confirmation of nodal metastasis with ultrasound-guided needle biopsy is less reliable (77% accuracy, 71% sensitivity, 89% specificity, 92% positive predictive value, and 62% negative predictive value20). Malignant nodes are differentiated from reactive nodes by being hypoechoic, hypervascular, and irregular.21,22 Endorectal ultrasonography and magnetic resonance imaging (MRI) with endorectal coil exhibited similar accuracy and were superior to conventional computed tomographic (CT) scans in preoperative assessment of depth of invasion and adjacent organ invasion.23 High-resolution MRI (83% accuracy, 94% sensitivity, and 67% specificity) and positron emission tomography (PET)-CT (70% accuracy, 61% sensitivity, and 83% specificity) may be helpful in predicting nodal status.24 Improved diagnostic staging information is essential in considering local treatment for rectal cancer, deciding on selective use of preoperative chemoradiotherapy in locally advanced tumors, and choosing between an abdominoperineal and low anterior resection. Both MRI and PET are being investigated for the assessment of pathological response following neoadjuvant therapy.25,26 The liver is the most frequent site of metastasis, followed by the lung, retroperitoneum, ovary, peritoneal cavity, and, rarely, the adrenal glands or bone. Contrast-enhanced CT scan of the abdomen and the pelvis is recommended in all patients with rectal cancer, excluding the very elderly and those with very early cancer, such as cancer within a polyp or T1 rectal cancer. MRI is reserved for patients with locally advanced and recurrent rectal cancer requiring an exenterative procedure. A plain chest radiograph is useful and economical for screening for lung metastasis. Laboratory studies should be ordered as indicated by the patient’s medical condition and anesthetic requirements. Measurement of the carcinoembryonic antigen (CEA) level in combination with imaging can refine the accuracy of preoperative assessment and overall prognosis. Up to 95% of patients with advanced hepatic metastasis will have a CEA level above 20 ng/mL.27 Patients with a normal CEA prior to colorectal resection may still have an elevated CEA with recurrence, so follow-up should include CEA testing postoperatively. Postoperative CEA monitoring may only confer minimal survival advantage. A review of a prospective database of 1900 patients treated for primary colorectal cancer whose follow-up included CEA monitoring found that two-thirds of recurrences were associated with an elevated CEA, which, in turn, was associated with decreased survival. However, of all patients who underwent potentially curative re-resection, only 17% had an elevated CEA.28 Kaposi sarcoma of the rectum should be suspected in patients with acquired immunodeficiency syndrome who are seen with an unusual or atypical anorectal lesion. It is often associated with proctalgia (62%), hematochezia (50%), and diarrhea (50%).29 Rectal carcinoids are often found incidentally during a screening colonoscopy or typically present with symptoms of bleeding, rectal pain, or constipation. They tend to be more indolent and less aggressive than colonic carcinoids, but as with most gastrointestinal carcinoids, tumor size correlates with the risk of metastasis and survival rates. Endoscopic resection is often adequate. Gastrointestinal stromal tumors of the rectum (Fig. 78-2) are uncommon and often present as a source of lower gastrointestinal bleeding, rectal pain, or constipation. Because of their malignant potential and recent advances in their management with imatinib mesylate (Gleevec), it is imperative that these tumors be correctly diagnosed. Positive immunohistochemical staining with CD34 and CD117 confirms the diagnosis. For large or low-lying rectal gastrointestinal stromal tumors, neoadjuvant therapy with imatinib can facilitate local and sphincter-preserving excision. Except for inflammatory masses, developmental cysts (such as dermoid, epidermoid, duplication, and tailgut cysts) and embryonic tumors (such as teratomas, chondromas, and meningoceles) are the most common retrorectal tumors. Other sacral and presacral tumors include neurogenic tumors, liposarcoma, and neurofibromatosis. Sacral pain and the sensation of fullness in the perirectal area are the most common symptoms of retrorectal lesions.30 Digital rectal examination is the most important diagnostic maneuver. Posteroanterior and lateral radiographs of the sacrum and CT scanning are the preferred methods for characterization and differential diagnosis of retrorectal masses. MRI may also aid in planning the operative approach. Barium enema evaluation will confirm the presence of mass effect. Proctoscopy, although indicated, is usually normal. Most retrorectal lesions should be resected when diagnosed, even if they are asymptomatic and seem benign. Preoperative biopsy is generally not recommended, as it will not change the surgical need for resection and may contaminate the surgical field or lead to abscess formation. Biopsy is reserved for unresectable large retrorectal tumors. For most patients with early rectal cancer (T1 to T3), surgical resection is the primary treatment modality. Sound surgical techniques and adjuvant therapy can improve outcomes and maximize local and overall control rates. Tumors in the upper third of the rectum have their lowermost edge 12 cm from the anal verge. Anterior resection or low anterior resection is the primary surgical procedure. Middle and lower-third rectal cancers can be treated with restorative proctectomy with colorectal or coloanal anastomosis or abdominosacral resection with results similar to those that are achieved with abdominoperineal resection and permanent colostomy.31 Overall surgical success depends on the ability to obtain a 2-cm distal margin; surgical expertise in obtaining clear lateral margins; the patient’s body habitus, pelvic width, and prostate size; adequate collateral blood flow through the marginal artery; and whether or not there is associated colonic disease such as diverticulosis. Local approaches may be appropriate for patients with early rectal cancer within 8 cm from the anal verge and in patients with major medical contraindications to radical surgery. Selection factors for full-thickness local excision are the same as or similar to those used for endocavitary radiation therapy. Consequently, this decision is based largely on findings of a digital rectal examination with increasing integration of transrectal ultrasound or MRI with endorectal coil.20,23,32 Patients with T1 tumors without adverse pathological features have a low incidence of local failure (5% to 10%) or lymph node involvement (<10%). With unfavorable pathological features (lymphovascular invasion, high grade, deep submucosal invasion, signet ring cell, or colloid histology)33–36 or evidence of tumor invasion into or through the muscularis propria,35,37,38 the local recurrence rate is at least 17%, and the risk of regional lymph node involvement is at least 10% to 15%.33 In an analysis by the Massachusetts General Hospital of 40 patients who underwent local excision only, patients were categorized according to unfavorable clinical or pathological features.35 Among patients with T1 or T2 cancers following local excision, Blumberg and associates reported positive lymph nodes in 10% of T1 cancers and 17% of T2 cancers.39 In addition, among the total group of 159 patients, the incidence increased with the presence of lymphatic and vascular invasion (14% without vs. 33% with). Even among the 42 patients with the most favorable features (negative lymphatic and vascular space involvement, well- or moderately differentiated T1 cancers), 7% were found to have lymph node involvement. The overall 5-year survival rate for the whole group was 65% with a locoregional recurrence rate of 27%. Hager and associates reported on a series of 20 patients with T2 rectal cancer for which local excision was performed and who were otherwise thought to be “low risk” (well to moderately differentiated, nonmucinous, no lymphovascular invasion, and negative margins), despite which the incidence of locoregional failure was still 17%.37 Others have reported locoregional failure rates as high as 43% following either local or transanal excision in patients with T2 cancers.40 There have been no randomized trials that compared transanal full-thickness local excision alone for T1/T2 with or without adjuvant chemoradiation with low anterior resection or abdominoperineal resection. Recent published results of local excision of T1/T2 rectal lesions without adjuvant therapy show local recurrence rates of 3.4% to 18% for T1 lesions and 27% to 67% for T2 lesions; Table 78-1 summarizes these results. Table 78-1 Local Excision of T1, T2 Lesions Without Adjuvant Therapy in Selected Series with More Than 50 Patients DFS, Disease-free survival; LR, local recurrences; NS, not specified; OS, overall survival. *In this series, 16 patients received postoperative radiotherapy and 15 additional patients received postoperative 5-FU and radiotherapy; however, local and overall recurrence rates were similar in both groups. Optimal candidates for local excision along include small (<4 cm), noncircumferential (<40%), low-lying tumors confined to the muscularis propria, without adverse pathological features (signet ring histology, poor differentiation, lymphovascular invasion). Local excision does not include lymph node evaluation, and adjuvant radiation with or without chemotherapy may be warranted.41 TEM is a minimally invasive surgical technique that was introduced in 1984 by Buess. It incorporates a high-quality binocular operating system and pressure-regulated insufflation with continuous suction. Compared with conventional transanal resection, TEM provides superior intraoperative visualization and the ability to perform full-thickness excision of the tumor with clear margins, together with perirectal fat and adjacent lymph nodes42,43 of tumors higher up in the rectum (4 to 18 cm from the anal verge). The technique is not yet generally established because of the high cost, the necessary special instrumentation and tools, and the unusual technical aspects of the approach.43–51 Treatment of cT2 rectal tumors with TEM combined with preoperative high-dose radiotherapy in 35 patients achieved survival rates similar to those of conventional open surgery.52 Only minor postoperative complications occurred in five (14.3%) patients and included suture-line dehiscence in three patients and stool incontinence in two patients. At a median follow-up period of 38 months, one patient was seen with a local recurrence (2.9%) at 30 months of follow-up, and systemic metastasis developed in four patients (11.4%). The survival and local recurrence rates that were reported in that study led to a prospective multicenter randomized trial (the so-called Urbino trial) to evaluate the efficacy of local excision in T2 tumors that were preoperatively treated by chemotherapy and high-dose radiotherapy versus standard open treatment (low anterior resection or abdominoperineal resection). At a median follow-up period of 56 months (range: 44 to 67 months), the local failure rate (5%) and distant metastasis rate (5%) were equal in the two groups.53 A recent review of the United Kingdom national TEM database from 21 centers since 1993 showed that of 454 rectal cancer patients, 69% underwent TEM with curative intent. The overall morbidity and mortality of TEM were 17.2% and 1.5%, respectively. Pathological staging was as follows: pT0 (1.8%), pT1 (52.9%), pT2 (32.8%), pT3 (9.9%), and pTx (3.1%). Neoadjuvant therapy and adjuvant radiotherapy were administered in 8% and 18% of cases, respectively. Margin positivity (<1 mm) occurred in 20% of cases and was stage dependent. The 5-year disease-free survival rate was 77% for pT1, 74% for pT2, and 35% for pT3, with local recurrence rates of 20%, 25%, and 59%, respectively.54 Sharp, total mesorectal excision (TME) with autonomic nerve preservation is the radical surgical technique of choice in conjunction with low anterior resection or abdominoperineal resection (APR). The mortality rate is 1% to 7%, and the morbidity rate (including genitourinary dysfunction, fecal incontinence, and permanent colostomy) is 13% to 46%. Locoregional recurrent disease is observed in 4% to 20% of cases, and the 5-year survival rate is 74% to 87%.55–59 The ability to obtain a negative lateral circumferential margin is associated with a decreased risk of local recurrence.60–63 In a multivariate analysis, circumferential margin involvement was the most powerful predictor of local recurrence (hazard ratio: 12.2) and of overall cancer mortality (hazard ratio: 3.2; Fig. 78-3). Heald and colleagues have advocated total mesorectal excision (TME) in conjunction with low anterior resection or abdominoperineal resection (APR) as the optimal surgical treatment for rectal cancer.56 This technique involves removal of the entire rectal mesentery, including that distal to the tumor, as an intact unit. Complete distal TME is essential for clearance of any tumor deposits, which occur in 50% of T3 tumors with a maximal distal spread of 4 to 5 cm,64 and is associated with increased frequency of local recurrence and decreased overall survival.65,66 The ability to perform sphincter-preserving surgery in nonirradiated patients is dictated by the requirements of a 2-cm distal margin rather than the traditional 5-cm margin.67–71 Only 2.5% of patients (usually with poorly differentiated and node-positive rapidly disseminating disease) had disease spread greater than 2 cm.31 There is no correlation between risk of local recurrence and the extent of distal margin in excess of 2 cm.72–77 Proximal lymph node dissection should extend just distal to the origin of the left colic artery. No evidence indicates a relationship between local recurrence and survival and dissection of deep iliac lymph nodes78 or high ligation of inferior mesenteric pedicle.79,80 Patients with pathologically positive nodes along the inferior mesenteric artery have very low 5-year survival rates.81,82 Laparoscopic surgery for curable rectal cancer has become increasingly accepted. Laparoscopic anterior resection with curative intent generates considerably more reservations than does laparoscopic APR, which is technically much easier to perform. Data, including results from randomized trials, on the extent of lymphadenectomy, margins of resection, actuarial survival, and local recurrence rates continue to emerge. The technique of laparoscopic TME is well described by Pikarsky and associates.70 Reports suggest short-term gains of reduced pain, shortened hospital stay, accelerated activity, possible cost reduction, and improved cosmesis.71 Hand-assisted laparoscopic surgery is a new technique that has the potential to overcome many of the existing limitations of pure laparoscopy.83 A prospective nonrandomized single institution trial comparing open versus laparoscopic resection in 191 consecutive patients with low and midrectal cancer demonstrated a conversion rate of 18.4%. In the laparoscopic group, the mean time for complete patient mobilization was shorter (1.7 vs. 3.3 days; P < 0.001), and patients were earlier in passing flatus (2.6 vs. 3.9 days; P < 0.001) and stools (3.8 vs. 4.7 days; P < 0.01) and in resuming oral intake (3.4 vs. 4.8 days; P < 0.001). The mean hospital stay and overall morbidity and mortality rates were similar with no statistically significant differences. Laparoscopic patients had a higher rate of anastomotic fistulas (13.5% vs. 5.1%) and reoperations (6.1% vs. 3.2%), but the difference was statistically nonsignificant. Laparoscopic resection presented a significantly lower local recurrence rate (3.2% vs. 12.6%; P < 0.05). Although the cumulative survival and disease-free rates at 5 years were nonsignificant between both groups (80% and 65.4% after laparoscopic surgery and 68.9% and 58.9% after open surgery), stage-by-stage comparison showed prolonged cumulative survival for stages III and IV cancer in the laparoscopic group (82.5% vs. 40.5%; P = 0.006 and 15.8% vs. 0%; P = 0.013, respectively) and a reduced rate of cancer-related death for stage III in the laparoscopic group (11.4% vs. 51.9%; P = 0.001).84 The U.K. Medical Research Council (MRC) prospective multicenter, randomized, controlled trial of conventional versus laparoscopic-assisted surgery in colorectal cancer included 128 rectal cancer patients in the open group and 253 patients with rectal cancer in the laparoscopy-assisted group with intent to treat. (The actual treatment groups included 132 open and 160 laparoscopy-assisted operations). Approximately 10% more patients underwent TME in the laparoscopy-assisted group than in the open surgery group. The rate of APR was similar (27% in the open surgery group and 25% in the laparoscopic group). Lymph node yield was equally high in the two groups. The intraoperative conversion rate from laparoscopic to open was 34%. In the intent-to-treat population, there was no significant difference in the open versus laparoscopy-assisted group with regards to positive circumferential margin (14% vs. 16%), overall intraoperative complications (14% vs. 18%), overall morbidity (50% vs. 59%), and mortality (5% vs. 4%). Although laparoscopic rectal resection did not adversely affect bladder function, there was a trend toward worse male sexual function, which might be explained by the higher rate of TME in the laparoscopic rectal resection group.85,86 In a 2006 systematic review by the Cochrane group, it was noted that most reported laparoscopic surgery studies for rectal cancer are individual cohort studies, individual case-control studies, or case series with only one reported randomized, controlled trial. Collectively, in 48 studies representing 4224 rectal cancer patients, there appeared to be no significant differences in disease-free survival rate, local recurrence rate, mortality, morbidity, anastomotic leakage, resection margins, or number of lymph nodes harvested. Laparoscopic approaches are generally associated with less blood loss, quicker return to normal diet, less pain, and less narcotic use, but are also associated with longer operative time and higher costs, and no results of quality of life were reported.87 A more recent meta-analysis of trials reporting oncologic outcomes for laparoscopic rectal resections included 1403 laparoscopic and 1755 open rectal resections from 24 publications; 5 of the 24 studies were prospective randomized trials, and long-term survival estimates were reported. This review found that although laparoscopic procedures harvested fewer lymph nodes (10 vs. 12), 3-year overall survival (76% laparoscopic, 49% open) and mean local recurrence (7% laparoscopic, 8% open) were not statistically different. There was also no difference in radial margin positivity.88 Following potentially curative standard or conventional surgical resection for adenocarcinoma of the rectum, the incidence of locoregional or distant treatment failure is related to the extent of transmural disease and associated involvement of regional lymph nodes by metastases.89–96 The incidence of locoregional failure is 8% to 21% in American Joint Committee on Cancer (AJCC) stage I disease (modified Astler Coller [MAC] stages A/B1), 29% to 44% in AJCC stage II disease (MAC stages B2/B3), and 50% to 61% in AJCC stage III disease (MAC stage C). The incidence of distant failure (as a component of failure) is up to 28% in AJCC stage I disease, up to 47% in AJCC stage II, and up to 74% in AJCC stage III disease. It has been claimed that when one compares these patterns of failure between multiinstitutional trial settings versus single-institutional and predominantly single-operator (surgeon) series, great differences in results can be seen. Table 78-2 summarizes these patterns of failure according to multiinstitutional versus single-institutional/single-operator series.89–96 Although distant metastasis is most likely to be attributed as the cause of death in rectal cancer patients, the potential influence of locoregional failure as an antecedent event to the development of distant metastases is clinically important. Hence, decreasing locoregional failure is an important end point of treatment in rectal cancer. These data and rationale serve as the basis for consideration of adjuvant chemoradiotherapy in the management of rectal cancer and, in particular, as a standard for AJCC stage II (MAC stages B2/B3) and stage III disease (MAC stage C). It is important to note that limited retrospective data identify subsets of patients with stage I disease who may be considered for adjuvant therapy, as well as subsets of patients with T3N0 disease who may not require adjuvant therapy.97,98 Willett and associates identified a subset of patients with stage I disease who have an increased incidence of locoregional failure following APR.97 In an additional review of 117 patients with T3N0 disease, Marks and associates identified a favorable group of patients with moderately or well-differentiated cancers invading less than 2 mm into perirectal fat who had a 10-year actuarial locoregional failure rate of only 5% following surgery alone, compared with 29% in T3N0 patients without these favorable features.99 Table 78-2 Patterns of Locoregional Recurrence and Overall Failure Following Standard/Conventional Surgery Alone for Rectal Cancer Table 78-3 summarizes the advantages and disadvantages of preoperative (typically chemoradiation) versus postoperative adjuvant therapy. The major advantages of preoperative therapy are tumor downstaging with increased resectability and sphincter preservation as well as a reduced incidence of acute and chronic toxicity. Adequate doses of radiation (≥4500 Gy) can sterilize peripheral margins of disease.96 Marginally resectable and unresectable tumors can undergo tumor shrinkage, making them amenable to curative surgical resection, particularly within the confines of the ridged, funnel-shaped bony pelvis, which often limits the potential for adequate circumferential margins of resection.63 Preoperative therapy also allows tumors to be resected with limited longitudinal surgical margins, thereby extending the level to which sphincter-sparing procedures can be performed safely in the distal rectum. These advantages, in turn, are associated with the potential for a significant reduction in a source of tumor spillage associated with locoregional recurrence of disease as well as a reduction of the dissemination during surgery of viable tumor cells increasing the risk for developing distant metastatic foci. The potential therapeutic advantage of preoperative therapy (particularly radiation) with enhanced oxygenation before surgical disruption of tumor blood supply is well established.100,101 Table 78-3 Advantages of Preoperative Versus Postoperative Adjuvant Therapy* Preoperative therapy also has the potential advantage of reducing the risk of treatment of both chemotherapy- and radiation-related morbidity compared with that seen with postoperative therapy.104–104 Following surgical resection, adhesions often develop and cause loops of bowel to be fixed within the pelvis. These fixed bowel loops often show enhanced tissue reaction with associated bacterial invasion, increasing the risk of severe treatment-related complications. In the preoperative therapy setting, the small bowel is less likely to be fixed within the treatment field and thereby is less prone to both acute and chronic treatment-related injury.
Cancer of the Rectum
Epidemiology
Clinical Presentation, Evaluation, and Staging
Differential Diagnosis
Surgical Treatment of Resectable Rectal Cancer
Local Treatment
Selection Factors
Reference
No. of Patients (Per Stage)
Follow-up Time
LR
Survival Rate
Salvage Surgery for Isolated LR
Paty et al.*358
125 (T1 = 74, T2 = 51)
6.7 years
T1 = 17% T2 = 26%
10-Year OS: T1 = 74%, T2 = 72%
14/17
Mellgren et al.359
108 (T1 = 69, T2 = 39)
4.4 years
T1 = 21% T2 = 47%
5-Year OS: T1 = 72%, T2 = 65%
24/27
Garcia-Aguilar et al.360
83 (T1 = 55, T2 = 27)
54 months
T1 = 18% T2 = 37%
5-Year: T1 = 98%, T2 = 89%
17/20
Chakravarti et al.296
52 (T1 = 44, T2 = 8)
52 months
28%
5-Year DFS: 66
NS
Steele et al.361
59 (T1 = 59)
48 months
T1 = 5%
6-Year survival: 85
2/2
Kim and Madoff362
69 (T1 = 44, T2 = 25)
NS
T1 = 9% T2 = 28%
Cancer-specific 5-year survival: 88%
NS
Hager et al.363
59 (T1 = 39, T2 = 20)
33–40.5 months
T1 = 8% T2 = 17%
5-Year survival: T1 = 90%, T2 = 78%
NS
Nelson et al.364
124 (T1=60, T2=164)
5 years
T1=12.5% T2=22%
5-Year OS: T1 = 77.4%, T2 = 67.6%
NS
Local Approaches
Radical Resections
Surgical Issues in Radical Resections
Radial Margins and Total Mesorectal Excision
Distal Mucosal Margin
Proximal Extent of Lymph Node Dissection
Laparoscopic Surgery
Patterns of Failure
Multiinstitutional Series
N*
MAC Stage
LR (%)
OF (%)
GITSC83
58
B/C
24
44
EORTC84
166
A–C
32
41
NSABP85
191
B/C
33
58
Stage I
Stage II
Stage III
Single-Institution Series
N
LR (%)
OF (%)
N
LR (%)
OF (%)
N
LR (%)
OF (%)
MDAH86
39
8
18
59
31
47
44
50
70
UT87
28
21
28
37
29
45
43
51
74
MSKCC88
47
14
—
69
44
—
52
61
—
MAC
Single-Institution and Predominantly Single-Operator Series
N
Stage
LR (%)
Patel et al.89
435
A–C
24
Enker et al.90
412
A–C
27
Adjuvant Therapy
Treatment Sequencing Issues
Preoperative Versus Postoperative Therapy: Potential Advantages and Disadvantages
Advantage
Preoperative Therapy
Postoperative Therapy
Tumor downstaging
+
–
Increased tumor resectability
+
–
Increased sphincter preservation
+
–
Treatment based on operative/pathological findings
–
+
Decreased locoregional recurrence
++
+
Increased survival
+
–
Cancer of the Rectum