29 Cancer of the Oral Cavity
Epidemiology and Genetics
Approximately 19,400 cases of oral cavity cancer (OCC) are seen in the United States each year, with 5200 deaths.1 It is more commonly seen among men than women, with an approximate ratio of 3 : 2.2 It is predominantly a disease of middle-aged men with a history of exposure to various carcinogenic chemicals, including tobacco smoke and alcohol. There is a clear dose-response relationship between the amount and duration of tobacco smoke exposure and the incidence of OCC. In countries such as India where smokeless tobacco (snuff) is popular, oral cancer is also common, although the risk is lower than for smoking (relative risk, 4.2 versus 10 to 15). The use of betel nuts is also related to oral cancer, particularly buccal mucosal cancer.3 Alcohol appears to act as a cocarcinogen and to have a topical effect in that mucosal areas directly exposed to alcohol have a higher incidence of oral cancer.4 Recently, for reasons that are unclear, there is an increasing trend in tongue cancer in young Americans who never had any exposure to tobacco or alcohol.5
The spectrum of molecular changes seen in oral cancer varies by country of origin.6 Mutations of p53 are common in oral cancers in patients from countries with European populations; for example, 47% of Europeans with oral cancer show mutated p53, whereas in patients from India and Southeast Asia, only 7% show mutations. Patients from these areas have tumors with abnormal ras genes, which include mutations, loss of heterozygosity (H-ras), and amplification (K-ras and N-ras). Loss of Rb gene function may be necessary in combination with p53 mutation for oncogenesis. It has been widely observed that oral cancers express transforming growth factor-alpha and epidermal growth factor receptor, which may trigger the autocrine growth pathway.7
Novel markers for the detection of OCC are an area of active research. There have been studies published on novel markers both for patients with a predisposition to OCC resulting from a prior history of oral leukoplakia,8 as well as in an adjunctive setting for diagnosis with messenger ribonucleic acid, using microarray profiling.9 In another study, Sudbφ and colleagues examined cytologic aberrations that persisted in the mucosa of long-term smokers that may predispose to OCC. The authors found that cytogenetic risk factors for OCC are present in smokers, and these findings may normalize after tobacco cessation.10
Anatomy
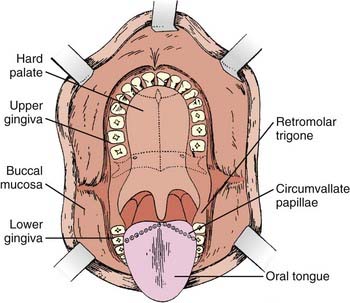
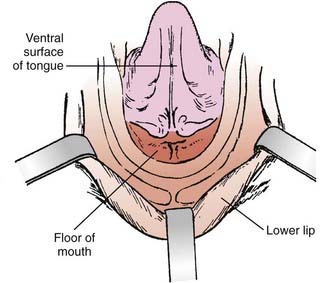
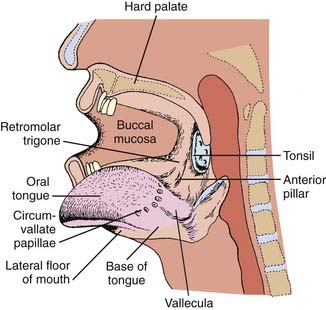
The oral cavity extends from the skin–vermilion junction of the lips to the junction of the hard and soft palate above, and to the line of circumvallate papillae below. It is divided into the following specific areas (Figs. 29-1 to 29-3).
Staging and Grouping System
The preferred clinical staging is the system found in the sixth edition of the American Joint Committee on Cancer (Table 29-1).11 T4 lesions have been divided into T4a (resectable disease) versus T4b (unresectable disease).
Diagnostic and Staging Studies
Positron emission tomography (PET) scan has also been shown to be of value in OCC staging. A study by Ng and colleagues prospectively evaluated 134 patients with squamous cell OCC and a palpably negative neck with both [18F]fluorodeoxyglucose (FDG) PET scan and CT or MRI. The sensitivity and specificity of PET plus CT or MRI scanning was slightly higher than with a PET scan alone (although not significant), and the PET scan was found to reduce the probability of occult neck metastases to less than 15% in T1 through T3 tumors.12 Another study by Kovacs and colleagues showed that PET scan in combination with sentinel node biopsy reduces the rate of elective node dissections in the treatment of oral and oropharyngeal cancer. Thus, PET scan has become more widely used in the staging of OCC and appears to have an additional benefit when compared with traditional staging with CT and MRI alone.13
General Therapeutic Approaches
Combined Chemotherapy and Radiotherapy for Locoregionally Advanced Disease
Chemotherapy has been combined with radiotherapy in the management of patients with unresectable OCC with the goals of increasing local control and survival as well as decreasing distant metastases. The chemotherapeutic agents most commonly used include cisplatin, paclitaxel (Taxol), fluorouracil (5-FU), methotrexate, and bleomycin. Except for one randomized study reported by Lo and colleagues, which showed increased survival in patients with oral cavity lesions receiving 5-FU concurrently with radiotherapy as compared with patients receiving radiotherapy alone,14 there has been no definitive evidence for improved local control or survival in oral cancer when single-agent chemotherapy is combined with radiotherapy. Two recent randomized studies examined multiagent chemotherapy with consolidative chemoradiation in the treatment of locoregionally advanced head and neck cancer, comparing regimens of cisplatin, 5-FU, and docetaxel with cisplatin and 5-FU alone. One study found improved progression-free survival and overall survival,15 while the other study demonstrated improved locoregional control and overall survival.16 Enhanced radiation mucositis has been commonly observed with concurrent drug and radiation administration, especially when 5-FU is given concurrently with radiation.
Targeted agents are also being used to further improve outcomes. A study by Bonner and colleagues compared patients with advanced head and neck malignancies who were treated with radiation therapy alone versus radiation therapy with cetuximab, and found a median overall survival of 23 months in the control group and 49 months in the experimental arm, changing the treatment approach for patients with advanced disease and creating a pathway for the study of other targeted biologic agents in this disease.17
Postoperative Radiotherapy
The aims of postoperative radiotherapy are (1) to prevent local recurrence when there is known residual gross or microscopical disease after surgery, (2) to prevent recurrence in the neck when there are large or multiple lymph node metastases and tumor invasion of the soft tissues in the neck, and (3) to control occult disease in the cervical lymph nodes that were not resected surgically.18 When radiotherapy is given postoperatively, usually a dose of 60 to 66.6 Gy is delivered in 1.8- to 2.0-Gy daily fractions, five fractions a week, to the primary site and involved neck areas. The clinically and pathologically uninvolved neck areas receive 54 Gy.19 It is generally believed that tumor cells trapped in the surgical scars are less well oxygenated and therefore more radioresistant, and that higher radiation doses are required to eradicate them than are required preoperatively. However, this belief has not been adequately tested. Apparent differences in doses required preoperatively and postoperatively may be due to proliferation of tumor cells in the postoperative period before radiotherapy starts. The volume that is irradiated should include the entire surgical bed and the entire neck. Postoperative radiotherapy can be started as soon as wound healing is complete, usually within 2 to 3 weeks after surgery.
Postoperative Chemotherapy and Radiation
Much of the shift in treatment paradigm over the past several years in the management of OCC has arisen from multiple studies assessing when a postoperative chemoradiation approach achieves better outcomes than postoperative radiation alone. The landmark studies of the Radiation Therapy Oncology Group (RTOG) 9501 and the European Organisation for Research and Treatment of Cancer (EORTC) 22931, followed by the comparative analysis of Bernier and colleagues, demonstrated that all patients with resected head and neck cancer receiving standard fractionated postoperative radiation who are found to have positive margins or extranodal extension should be assigned to a combined chemoradiation approach using concurrent cisplatin (100 mg/m2 on days 1, 22, and 43).20–22 More recently, the German Cancer Society 95-06 trial23 demonstrated that even with hyperfractionated accelerated treatment regimens, patients that received concurrent 5-FU and mitomycin experienced an improvement in locoregional control and overall survival. Finally, a study by Garden and colleagues examined patients with stage III and IV disease who received a concomitant boost treatment regimen and cisplatin on days 1 and 22, and found that 4-year locoregional progression-free survival was 74% and that 4-year overall survival was 54%—results which are quite promising.24 Clearly, the ideal chemotherapeutic regimen in the postoperative setting has not yet been fully elucidated.
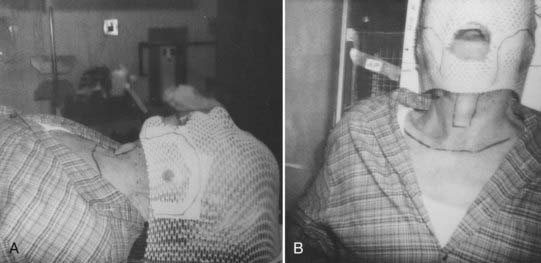
Simulation
IMRT now has widespread acceptance in the treatment of OCC. These patients are simulated in the supine position, and surgical scars are wired as described previously. A mask is then generated to encompass the head and neck region and a bite block is used when appropriate. A CT, MRI, or PET simulation scan is taken and an isocenter is set. If a low anterior neck (LAN) field is being generated to treat the low neck lymph nodes, then at our institution we generally set the isocenter at the match line of the IMRT and LAN fields. The isocenter is generally placed directly above the arytenoids. However, when there are bulky lymph nodes that extend inferior to this point, we treat with whole-field IMRT. Fig. 29-4 depicts a three-point mask, in which the head and neck are immobilized. For patients in whom more rigid lower neck and shoulder immobilization is preferred, a five-point mask can be used that extends inferiorly to immobilize these structures.
General Techniques of Radiotherapy and Treatment Plans
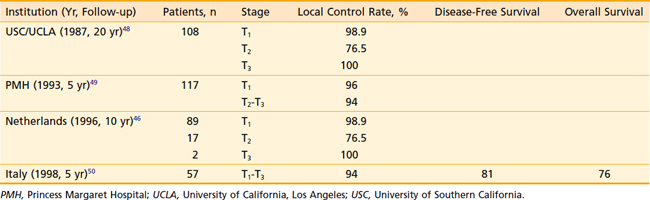
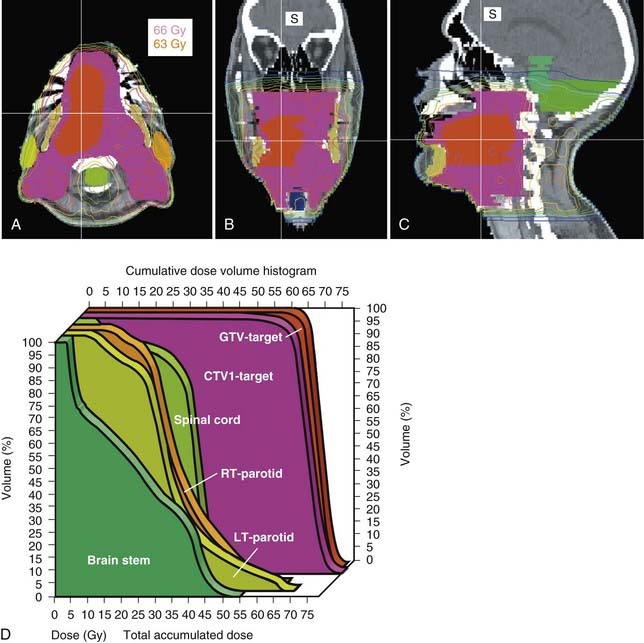
Megavoltage External-Beam Radiotherapy
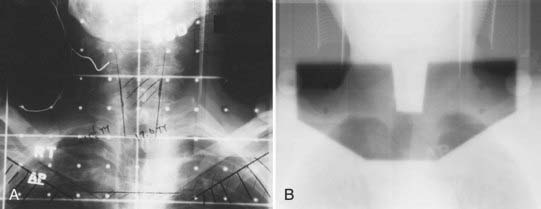
The treatment volume encompassing the primary tumor with adequate margins and cervical lymph nodes of concern is outlined on the treatment simulation films, the skin, or on the relevant imaging slices in the case of IMRT or in 3-D conformal therapy (CT, MRI, or PET scan). When conventional techniques are used, metallic wires, gold seeds, or silver clips placed in the tumor periphery are helpful in localizing the tumor volume on the simulation films. Normal tissues that are in the field but need not be irradiated are shielded with either mounted lead blocks or multileaf collimators. Examples of treatment of an advanced carcinoma of the tongue are shown in Figs. 29-4 to 29-6. Weekly port films are obtained with the patient on the treatment machine to verify the actual volume irradiated. All fields are treated daily. The usual dose fractionation is 1.8 to 2 Gy per day, with five daily treatments per week. The total dose depends on the extent of the disease and whether external-beam radiotherapy is used alone or in combination with interstitial radiotherapy or surgery. When definitive external-beam alone is used, the total dose is usually in the range of 70 to 74 Gy. The spinal cord is either shielded after 44 Gy or constrained in the radiation plan to a dose of 45 Gy or less.
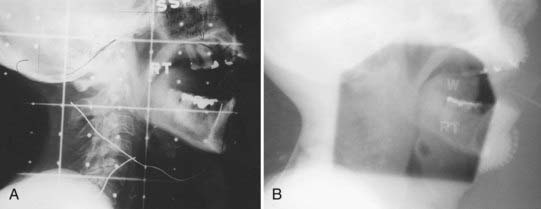
FIGURE 29-5 • A, Simulation film of lateral port for tongue carcinoma. B, Portal film of lateral port.
Peroral Cone Radiotherapy
Intraoral cone radiotherapy using 100 to 250 kVp x-rays or 6 meV electron beams is suitable for the treatment of select small lesions, less than 3 cm in diameter, in the floor of the mouth. For the proper administration of this radiotherapy modality, it is necessary that adequate coverage of the lesion is achieved with the intraoral cone and that patient immobilization be maintained during treatment. The use of a special immobilizing chair that locks the patient and applicator in a rigid unit is advised for orthovoltage treatment, as shown in Fig. 29-7. The analysis by Phillips on the time-dose relationships in peroral radiotherapy for oral cancer suggests that surface doses between 55 Gy in 18 days and 60 Gy in 26 days will result in good control rates with acceptable risk of soft-tissue or bone necrosis.19 Wang has described a technique for using peroral cones with electron beams (Fig. 29-8).25

FIGURE 29-7 • Peroral cone for orthovoltage with treatment chair.
(From Phillips TL: Peroral roentgen therapy, Radiology 90:525, 1968.)
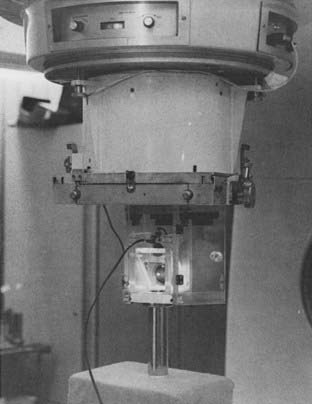
FIGURE 29-8 • Electron beam peroral cone set up at Massachusetts General Hospital.
(From Wang CC: Technical and radiotherapeutic considerations of intra-oral cone electron beam radiation therapy for head and neck cancer, Semin Radiat Oncol 2:171, 1992.)
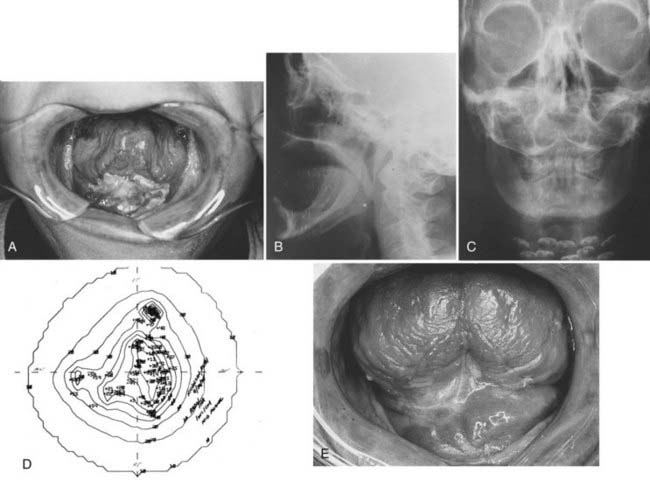
Brachytherapy
Interstitial radiotherapy, either alone or in combination with external-beam radiotherapy, is used for selected cases in the treatment of carcinoma of the oral tongue, floor of the mouth, and buccal mucosa.26,27 Radioactive isotopes that have been used in the past in interstitial radiotherapy of oral carcinomas include radium-226, cesium-137, gold-198, and tantalum-182. Iridium-192 used in the form of pins (epingles), wires, or seeds preloaded in a plastic ribbon have the advantage of being suitable for afterloading techniques, and thus is used commonly for temporary implants. Iodine-125 may be substituted and is the isotope of choice for permanent implants. The use of remote afterloading of iridium sources with high-dose rate (HDR) is replacing the use of hand-loaded seeds in ribbons in most institutions. These techniques minimize exposure to personnel and allow optimization of dose distribution.28
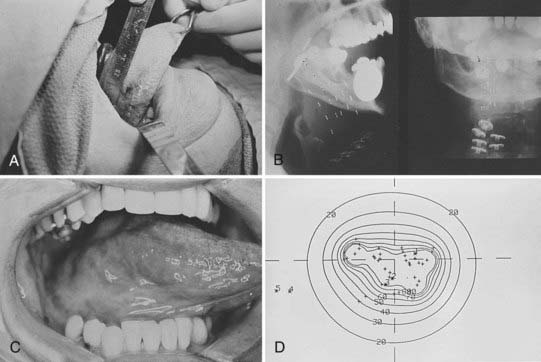
When the tumor thickness is 1 cm or less, a single-plane implant is adequate. When the tumor thickness is greater than 1 cm, then a double-plane implant or volume implant is necessary to deliver a relatively uniform dose to the tumor volume. The Patterson-Parker or Quimby tables are often used for treatment planning; however, dosimetry is best done by a computer using localization films of the actual implant.29,30
When interstitial radiotherapy is used alone for patients who present with early-staged T1 to T2-N0 disease, the usual implant dose is 60 to 70 Gy delivered over a period of 6 to 7 days.31,32 For oral tongue lesions, if a combination of external-beam radiotherapy and interstitial implant is considered, several series have reported on the importance of adequate interstitial implant dose. The total implant dose is correlated with local control. Those patients who received an external-beam dose less than 40 Gy along with a higher brachytherapy dose achieved higher local control rates than those who received a lower brachytherapy dose.33–36 If the patients have neck disease, surgery with or without postoperative radiotherapy is recommended over radiotherapy alone.
No adjustment of total dose is made when the dose rate of the minimum tumor dose is between 30 and 60 cGy per hour.35 Examples of a single-plane iridium implant and a volume iridium implant and the isodose distributions are shown in Figs. 29-9 and 29-10.
Carcinoma of the Lip
Clinical Presentation
Second to the skin, carcinoma of the lip is the most common cancer of the head and neck. In the United States, lip cancer accounts for 12.7 per 100,000 annually.37 It is rare among blacks and Asians, and accounts for approximately 25% of all carcinomas of the oral cavity. Approximately 90% of the carcinomas of the lip arise from the lower lip. Elderly men are affected most frequently, particularly in the sixth and seventh decades. The incidence rates are generally stable or falling among men worldwide, but are rising among many female populations.38 Chronic exposure to sunlight appears to be a predisposing factor, as carcinoma of the lip occurs most frequently in light-complected, fair-skinned persons who work outdoors.39 Other possible causal factors are tobacco smoking and viruses.
The majority of carcinomas of the lower lip are moderately to well-differentiated squamous cell carcinomas. Basal cell carcinomas make up the majority of upper lip lesions.40 Basal cell carcinomas arising from the skin that invade the lips secondarily should be considered carcinomas of the skin.
Carcinoma of the lower lip frequently presents as a thickening of the mucous membrane. Later, desquamation and ulceration that does not heal may develop. There may be a history of long-standing keratosis or leukoplakia.41
Routes of Spread
Carcinoma of the lip tends to be localized. It usually spreads by direct invasion of the surrounding soft tissue, skin, and bone, and infrequently metastasizes to regional lymph nodes.42 The incidence of lymph node metastasis varies with the extent of the primary lesion. The average incidence of regional lymph node metastasis is approximately 3% to 8% on presentation, and approximately an equal proportion of patients develop cervical lymph node metastasis subsequent to treatment of the primary lesion. There is a rare incidence of perineural spread, often into the mandibular canal.43
Treatment Approach
Carcinoma of the lip can be treated successfully with either radiotherapy or surgery.44 The choice of treatment depends on the extent of disease, the functional and cosmetic results of the treatment, expediency, the patient’s age, and the available treatment personnel and facilities.45 Radiotherapy is usually indicated for moderately large (>3 cm) infiltrative lesions that would otherwise require a complicated plastic surgery with less satisfactory cosmetic and functional results. Radiation is also indicated for tumors involving the commissure because surgical excision of the commissure would not yield satisfactory cosmetic and functional results.46 Elderly patients who are at a high risk for complications from general anesthesia or who have persistent or recurrent disease after surgery should be considered for radiotherapy. Radiotherapy is also administered postoperatively when the surgical margin is inadequate, there is invasion of the soft tissues of the neck caused by cervical lymph node metastasis, and in combination with surgery for advanced resectable disease. Surgery is usually preferred for small lesions, young patients, very advanced disease with bone invasion, cervical lymph node metastases, and recurrent disease after radiotherapy.
Radiotherapy modalities commonly used for carcinoma of the lip include external-beam radiotherapy with orthovoltage x-rays or electrons,47 and interstitial implants with radium or iridium.27 The “sandwich” technique has also been used in some centers; however, fractionated external-beam radiotherapy usually yields more satisfactory cosmetic results, especially for moderately advanced disease. When interstitial radiotherapy is used, a dose of 60 to 70 Gy in 6 to 8 days is usually adequate.
When external-beam radiotherapy is used, a lead cut-out is usually made to outline the treatment volume. A lead shield can be inserted between the inner surface of the lip and the gingiva to prevent irradiation of the intraoral structures. The treatment volume should include the lesion with adequate margins. Leukoplakic changes on the lip adjacent to the lesion should also be included in the treatment volume. For small superficial tumors, a single field with 100- to 150-kV x-rays is sufficient. For deeper, more advanced tumors, 200- to 250-kV x-rays or electrons are usually used. The optimal dose-fractionation schedule depends on the volume of irradiation. For small lesions (<2 cm in diameter), a dose of 45 Gy to 50 Gy in 15 fractions over 3 weeks is usually adequate, with good cosmetic results. For larger lesions, more protracted treatments with 50 to 70 Gy in 4 to 7 weeks are often used. The base of the skull should be adequately covered in cases with perineural involvement (Fig. 29-11). The neck is usually not irradiated unless cervical lymph node metastasis is present. Acute moist skin and mucous membrane reactions are managed with frequent cleansing and saline soaks. Topical antibiotics are rarely used unless there is an infection.
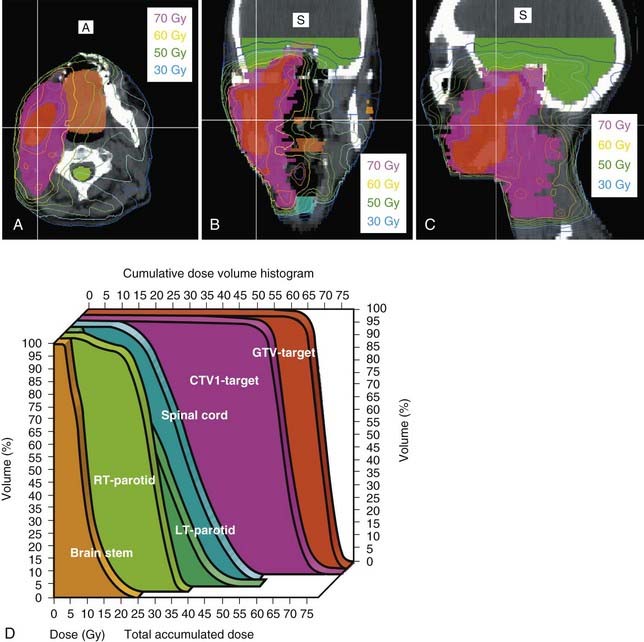
Treatment Outcome
Results of radiotherapy in select series of patients treated with radiotherapy for carcinoma of the lip are shown in Table 29-2.46,48–50 Control of the primary lesion can be achieved with external-beam irradiation or interstitial implants in the majority of patients. Those with recurrent disease after radiotherapy or cervical lymph node metastasis are usually treated surgically. Death resulting from uncontrolled carcinoma of the lip is uncommon (<10% in most series). The local control rate by interstitial implant is comparable to that achieved with external irradiation, although for larger lesions, better cosmetic results are obtained with protracted external-beam radiotherapy.
Carcinoma of the Oral Tongue
Routes of Spread
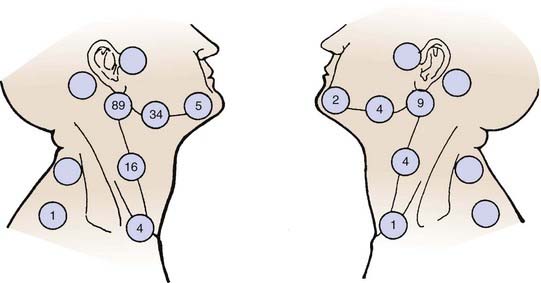
Carcinoma of the oral tongue usually spreads by direct invasion into the floor of the mouth, anterior tonsillar pillar, base of tongue, and mandible. Approximately 30% to 40% of the patients have cervical lymph node metastasis on presentation. The thickness as well as the T stage of the tongue lesion is directly correlated with the incidence of lymph nodal involvement.32,51 The subdigastric nodes are most frequently involved. The submandibular and midjugular lymph nodes are less commonly involved, and the submental, lower jugular, and posterior cervical nodes are rarely involved. Distant metastasis is seldom detected before death. The lungs, liver, and bones are the most common distant metastatic sites. Approximately 19% of patients develop a second malignant tumor. The majority of the second cancers are in the upper respiratory-digestive tract. The distribution of lymph nodes reported by Lindberg is shown in Fig. 29-12.52
Treatment Approach
Surgery followed by radiotherapy for both the primary site as well as the bilateral necks is the preferred treatment modality for carcinoma of the oral tongue. Invasive pattern; T1, T2, T3, or T4 lesions; bone invasion; multiple cervical lymph node metastases; close or positive margins; and lymphovascular or perineural invasion are indications for postoperative radiotherapy. In regard to an invasive pattern, multiple studies have demonstrated that the risk of cervical lymph node metastases is much greater for tumors with a depth of invasion of 5 mm or greater.53,54 In patients with positive margins or extranodal extension, a postoperative chemoradiation approach has been shown to be superior to radiation alone in the analysis of pooled RTOG and EORTC data by Bernier and colleagues, and now is the standard of care, albeit with increased toxicity.20–22 Attempts to spare the parotid glands can be made to reduce xerostomia, particularly with the advent of IMRT (Figs. 29-13 and 29-14).55 With the excellent functional outcome of the reconstructed oral tongue after hemiglossectomy, definitive radiotherapy with or without chemotherapy is reserved for selected cases (i.e., if the patient is medically inoperable or if the lesion is unresectable). It must include brachytherapy to be effective.56,57