Cancer of the Lip
Jessica J. Peck
Daniel Petrisor
Mark K. Wax
Approximately 25% of all carcinomas of the oral cavity involve the lips, making the lips the most commonly affected subsite in the oral cavity. The prominent location of cancers of the lip allows for early detection of pathology. The lips play such a prominent role in how we present ourselves to the outside world that any abnormality is immediately noticed and reacted to. The fact that lesions of the lips are detected so early makes treatment relatively easy and successful, making cancer of the lip one of the most curable cancers of the head and neck. Unfortunately, even with the prominent location and ease of detection, as many as 15% of the cases, the disease will demonstrate aggressive behavior manifested by recurrence, metastasis, and death from disease. Late presentation due to neglect or poor access to health care accounts for a portion of these cases. The vast majority of cancers of the lip are treated with local resection followed by repair through local tissue rearrangement. Reconstruction of larger defects after resection of larger tumors may require complex composite flaps to optimize both function and cosmesis.
ANATOMY OF THE LIP
The upper and lower lips are the most dominant feature of the lower third of the face. The area of the lips extends vertically from the subnasale to the mental crease and horizontally to each oral commissure. Embryologically, the lips are formed by the union of five facial processes. The upper lip is formed from the two lateral maxillary processes that fuse centrally with the frontomedian process, whereas two mandibular processes meet in the midline to form the lower lip.
The lip is a complex anatomical structure, which includes a muscular layer that is a part of the oral sphincter, lying between a mucosal layer and the overlying skin. This muscular layer is composed of the orbicularis oris muscle, which is derived from the second branchial arch. The muscle fills most of the body of the lip and completely encircles the mouth creating the oral sphincter. This skeletal muscle helps in the regulation of food entrance and maintenance within the oral cavity. The orbicularis muscle of the lip is not a simple sphincter because, in its periphery, it receives fibers from the many different surrounding facial muscles. These act together with the orbicularis to produce the various shapes and functions that are possible with the lips, such as smiling, frowning, kissing, blowing, whistling, articulating speech, and closing the lips.
The most characteristic feature of the lip is the vermilion—a transitional mucosal surface that covers the free margin of the lip and bridges the external skin with the internal mucosa. The mucocutaneous junction forms the anterior vermilion border, whereas the posterior point of contact of the lips, when they are held closed, marks the posterior vermilion border.
Sensory innervation of the lip is supplied by the second and third division of the trigeminal nerve. The upper lip is supplied by the infraorbital branch of the maxillary nerve (V2), exiting from the infraorbital foramen. The oral commissure is supplied by the buccal branch of the mandibular nerve (V3). Lower lip sensation is supplied by the mental branch of the mandibular nerve, which enters the mandible as the inferior alveolar nerve at the inferior alveolar foramen. The nerve traverses the mandible and exits through the mental foramen as the mental nerve. The nerve transitions from posterior to the mandible to anterior as it passes through the mandible. As the nerve of the second branchial arch, the facial nerve provides lip motor innervation via the buccal and marginal mandibular branches. The buccal branch of the facial nerve supplies the upper lip, whereas the lower lip motor functions are supplied through the marginal mandibular branch.
The arterial supply to the lips is provided principally by the left and right facial arteries, from which arise first the inferior and then the superior labial arteries. These vessels encircle the left and right side of the mouth passing between the respective orbicularis and submucosa. Venous drainage is supplied by the left and right anterior facial veins. These run posterior to the facial arteries with their corresponding branches. Interconnections are abundant, and the total lip complex can survive on the contralateral supply.
Lymphatic drainage of the upper lip and oral commissure is accomplished by an interconnecting network of delicate vascular structures found in both the submucosal and subcutaneous tissue planes. This network goes on to drain into five collecting trunks on either side, which in turn drain laterally to the preauricular, infraparotid, submandibular, and submental lymph nodes. Embryonically, the central frontonasal process separates the lateral maxillary processes. As such, there is no contralateral drainage from the upper lip. By contrast, the mandibular processes of the lower lip fuse at midline, allowing numerous crossing anastomoses to occur. Lymphatic drainage to the lower lip therefore occurs to the submental and submandibular nodes bilaterally.
EPIDEMIOLOGY OF CANCER OF THE LIP
The incidence of cancer of the lip varies significantly throughout the world. It is presumed that the variations are due to such factors as race, environment, and personal habits. Overall, cancer of the lip is most commonly observed in the white, male, smoker, over the age of 50, with fair complexion and blue eyes. Thus, it should not be surprising that the highest incidence of lip cancer is reported among the white populations of Canada and Australia. More than 50% of oral cancers in Australians are located on the lip. Lip cancer is rare in the
nonwhite populations, as darkly pigmented populations have greater amounts of protective pigment within their vermilion.1
nonwhite populations, as darkly pigmented populations have greater amounts of protective pigment within their vermilion.1
Although a number of identified factors are felt to be associated with the development of cancer of the lip, ultraviolet light exposure is by far the greatest contributing factor and is associated with 90% of cases of cancer of the lip. Because the lips are located on the face, they are subjected to greater exposure to ultraviolet light than most of the other areas of the body. Eighty-eight percent to ninety-eight percent of cancers of the lip are found in the vermillion of the lower lip.2 It is believed that this is caused by outward projection of the lower lip together with a downward angulation that favors direct exposure of the vermilion to overhead sunlight.
On the lower lip, cancer is most frequently found on the exposed vermilion border, arising at the point midway between the oral commissure and midline. Cancer arises in the commissure of the lip in fewer than 1% of all cases. This rate is roughly proportionate to the actual exposed surface area. Although the upper lip is also outwardly projected, its vermilion surface faces downward, away from direct sunlight. Malignancy arising in the upper lip vermilion constitutes only 2% to 7% of reported cases.3 When they occur, they most frequently arise near the midline where exposure to direct sunlight may be greatest.
Much of the evidence that has implicated ultraviolet light exposure as etiologic in cancer of the lip is derived from associations that have been made in case series studies and epidemiologic surveys. These studies and surveys show that at least one-third of patients who develop cancer of the lip have outdoor occupations, presumably subjecting them to substantial ultraviolet light exposure. UV radiation is known to produce mutations in DNA. When the body fails to repair these mutations, cancer may form. Regardless of the patient’s age, the damaging effects of excessive solar exposure can be expected to be found in patients who develop cancer of the lip. Typical findings include generalized atrophy of the vermilion, loss of elastic fibers, atrophy of adipose tissue, and glandular elements, as well as cellular changes such as hyperkeratosis and atypia. Advanced chronic solar injury to the lip often produces fading of the sharp color contrast normally seen at the mucocutaneous line. Areas of the vermilion that have sustained particularly severe solar injury may display areas of chronic scaling or crusting (actinic cheilitis) that are analogous to actinic keratoses found in sundamaged skin. In general, patients with cancer of the lip will often be found to have other sun-induced malignancies or premalignant changes in the surrounding vermilion and facial skin.
Exposure to tobacco products has clearly been shown to increase the risk for malignancy particularly within the oral cavity. The relationship between tobacco use and the development of cancer of the lip is less clear. The data so far have been based primarily on information obtained from various case series that have identified a large proportion of patients with cancer of the lip that has regularly used tobacco products. Some case controlled studies, however, have failed to support a distinct relationship of tobacco use with cancer of the vermilion of the lip.4
Immunosuppressed populations show a markedly increased risk for development of malignancies. This is particularly true for the development of squamous cell carcinoma (SCC) of exposed cutaneous surfaces. The increased risk of lip cancer among renal allograft patients on immunosuppressive therapies may be as great as 30-fold.5 People receiving higher doses of immunosuppressant’s tend to develop more nonmelanoma skin cancers than those on lower doses. These patients are also at an increased risk for development of second primary cancers of the lip.
A variety of other factors have been reported to have some association with the development of cancer of the lip. These include thermal injury, mechanical irritants, trauma, use of alcohol, poor oral hygiene, chemical exposure, influence of various infectious diseases, and prolonged exposure to harsh weather conditions (e.g., wind, cold, dryness). Currently, most of these can be considered only associations, because welldesigned and controlled studies to establish a firm causative relationship are lacking.
HISTOLOGY OF THE LIP
Histologically, the lips are covered by three distinct epithelial surfaces. The external skin is keratinizing stratified squamous epithelium with a rich complex of hair follicles, sweat, and sebaceous glands located in the dermis, whereas the lip vermilion is composed of nonkeratinizing stratified squamous epithelium, adapted for external exposure. It remains smooth and dry, due to the paucity of glandular structures in the submucosal layer. Finally, the labial mucosa contains many serous, mucous, and mixed salivary glands in its submucosal layer, keeping the epithelial surface moist. Both the vermilion and labial layers are pink due to the presence of many elongated, vascular connective tissue papillae that project into the epithelial layer.
HISTOPATHOLOGY OF CANCER OF THE LIP
Squamous Cell Carcinoma
More than 90% of cancers of the oral cavity are of squamous cell origin. This cancer first appears as a nonhealing blister, recurrent crusting, lip induration, or an exophytic growth. Clinically, it may be impossible to distinguish between actinic cheilitis and early squamous cancer, creating a low index of suspicion for biopsy. Three primary subtypes of SCC are identified in SCC of the lip: exophytic, ulcerative, and verrucous.
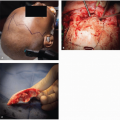
The exophytic form develops as an area of thickened epithelium that rises up from the surrounding tissue as it develops. With continued growth, there is a tendency for the base of the tumor to take on a saucer shape (Fig. 12.1). This base
extends only a few millimeters under the epithelium, but externally, the lesion becomes heaped up upon itself extending outwardly a centimeter or more. Laterally, lesions may extend several centimeters with relative little invasion or metastasis.
extends only a few millimeters under the epithelium, but externally, the lesion becomes heaped up upon itself extending outwardly a centimeter or more. Laterally, lesions may extend several centimeters with relative little invasion or metastasis.
The ulcerative type of SCC of the lip begins like the exophytic type, that is, as an epithelial thickening or blister. Ulceration usually occurs earlier and, in fact, may be present as a first symptom. As the lesion enlarges, it tends to take on a round or oval shape. Ulcerative carcinomas tend to bleed more easily than other subtypes. Further growth of the lesion tends to be more endophytic, displaying a relatively greater degree of invasion when compared with a similar-sized exophytic tumor.
Verrucous carcinoma occurs rarely on the lips. It is a unique form of SCC in both its clinical behavior and morphology. Clinically, the lesion develops with a warty surface. Verrucous types are usually broad based and locally invasive. Histologically, they are well differentiated with few malignant features, save for invasion. The margins tend to push, and the integrity of the basement membrane is generally preserved. Biopsy of suspected verrucous carcinoma should include the full thickness of the lesion and a segment of adjacent uninvolved tissue. It is otherwise possible for the diagnosis to be confused with other forms of hyperplasia or hyperkeratosis as well as other SCC forms.
Basal Cell Carcinoma
Basal cell carcinoma is the second most common malignancy of the perioral region, accounting for 1% of cancers occurring in this region. These cancers occur with approximately equal frequency in both the upper and lower lips, but because of the infrequency of other cancers affecting the upper lip, basal cell carcinoma vastly dominate the total percentage of lesions of the upper lip.6
There has been considerable debate in the medical literature as to the actual existence of basal cell carcinoma arising from the vermillion portion of the lip. It is argued that the vermillion is involved only by direct extension of a lesion, which began periorally. Indeed, nearly all basal cell carcinomas found involving the vermilion are reported as arising from the cutaneous portion of the lip, at or near the mucocutaneous borer.
Melanoma
Melanoma may arise at the cutaneous, vermilion, or mucosal portions of the lip from melanocytes normally found in those sites. When arising from the lip vermilion, it is considered a mucosal melanoma subtype. Mucosal melanoma is most frequently found in the palatal or gingival mucosa and is found with less frequency in the buccal mucosa and vermilion. It presents as a smooth, black, or blue submucosal nodule that is covered by a thin, intact mucosa. However, before the diagnosis of a mucosal melanoma is accepted, careful screening of other body sites is required to confirm that it does not actually represent a metastasis from a distant primary melanoma.2
PROGNOSTIC FEATURES ASSOCIATED WITH SQUAMOUS CELL CARCINOMA
Overall, carcinoma of the lip carries an excellent prognosis with 5-year survival rates reported at 79%.2 The fact that most patients present with relatively small and early tumors is obviously an important factor in achieving this outcome. Even so, most of these cancers will have been present in some form for many months after home treatment with antibiotic ointment or skin creams has failed. But this delay is often offset by the fact that these cancers tend to be slow growing, tending toward more superficial lateral growth while remaining confined to the vermilion or immediate submucosal tissues until later in their course. A small percentage of patients will postpone evaluation until later in the course of the disease, by which time the cancer has grown to involve the musculature of the lip.
The size of the primary cancer is one of the most significant factors in predicting prognosis. That when tumors grow to a size larger than 4 cm (T3), the 5-year survival rates drop to 60%. Studies also consistently indicate that the rate of metastases increases with the size of the cancer; regional nodal metastasis has been found to be 5% for T1 lesions, 50% for T2 lesions, and 70% for T3 lesions.7 When nodal metastasis occurs, 5-year survival is decreased to a reported rate of 40% to 80%.
Eighty percent of patients with perineural spread will have concomitant nodal metastasis. This further decreases 5-year survivor rates to 35%.8 Although only occurring in 2% of patients, perineural spread requires special consideration for treatment and prognosis. SCC and other malignancies of the lip may invade the mandible by perineural spread along the mental nerve. Invasion of the maxilla can also occur via the infraorbital nerve. Classical clinical symptoms of perineural spread such as tingling, numbness, and pain cannot be relied upon as early indicators. Several cases have been reported with early spread along the inferior alveolar nerve extending to the cranial cavity, despite the lack of symptoms and a relatively small cancer.
MANAGEMENT OF CANCER OF THE LIP
A lesion of the lip that is nonhealing or in any other way suspicious for malignancy should be biopsied to obtain diagnosis. Once histopathologic verification is made, a treatment plan can be formulated. This must include curative management of the primary cancer and for any regional metastasis that may be present. Choice of treatment is made based on the preferences of both physician and patient, taking into account size, location, age, concomitant medical conditions, the likelihood that function of the lip and/or cosmesis can be preserved or restored, the relative ease of treatment delivery, and considerations of time and cost. A variety of therapeutic methods have been successfully employed in the treatment cancers of the lip, to include surgical excision alone, radiation therapy alone (external beam, or brachytherapy), or combined surgical excision and radiation therapy. Most studies have shown that surgery or radiation therapy produce similar cure and cosmetic results for small tumors.9 These types of therapy are discussed below.
Radiation Therapy
Radiation therapy may consist of brachytherapy, external beam, or a combination of the two. Brachytherapy is a method of radiation therapy that employs the use of interstitial placement of radioactive implants. These are placed directly into the cancer and are carefully positioned to give a planned therapeutic dose to all parts of the cancer. Current practice favors the use of lower-energy radioisotopes such as iridium-192. First, hollow, nonradioactive needles are placed and checked
radiographically for proper placement. The radioactive source is then placed. Placement of multiple needles during several treatment sessions may be required. It is important that accurate spacing of the needles be performed at each session, as overlapping of the radiation points creates problems of uneven distribution of the radiation. Brachytherapy has a reported local recurrence-free survival of 93% following treatment.9 However, due to the complexities associated with brachytherapy, it has largely given way to external radiation, which is more versatile and controllable.
radiographically for proper placement. The radioactive source is then placed. Placement of multiple needles during several treatment sessions may be required. It is important that accurate spacing of the needles be performed at each session, as overlapping of the radiation points creates problems of uneven distribution of the radiation. Brachytherapy has a reported local recurrence-free survival of 93% following treatment.9 However, due to the complexities associated with brachytherapy, it has largely given way to external radiation, which is more versatile and controllable.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree