13 Breast Reconstruction after Mastectomy
Introduction
Breast reconstruction after mastectomy remains an essential part of the treatment for breast cancer. The improvements in the outcomes of breast cancer treatment lead more women to be concerned about the appearance of their breasts when treatment is complete. Also, with the increase in screening for genetic mutations of the BRCA1 and BRCA2 genes, reconstruction after prophylactic mastectomy has become more common. Studies have demonstrated that most women desire surgical breast reconstruction after mastectomy. Furthermore, since 1998, federal law has mandated that insurance companies cover breast reconstruction.1,2 Therefore, all health care providers who treat patients with breast cancer need to have a basic knowledge of the different types of breast reconstruction and inform their patients that such options are available. This will aid in the understanding and treatment of the “whole patient,” coordination of treatment with the ablative and reconstructive surgeons, and surveillance of local recurrence.
Excellent aesthetic results have been obtained with many types of breast reconstruction (Fig. 13-1). Breast reconstruction has also been shown to provide psychological and emotional benefit to reconstructed patients.3,4 Despite these facts, breast reconstruction rates after mastectomies are surprisingly low. Only 8.1% of patients in the United States undergo breast reconstruction, and these rates are lower in patients older than 50 years.5 This may be due in part to the lack of knowledge about breast reconstruction by oncologists and general surgeons who may incorrectly believe that it interferes with adjuvant treatment and detection of local recurrences.6 Proper knowledge of the benefits and risks of breast reconstruction should improve the rates of referral of mastectomy patients to plastic surgeons and the rate of reconstruction.
Reconstruction of the breast after mastectomy is an option that should be given to all breast cancer patients. Breast reconstruction should be discussed with any patient who is considering the treatment options of lumpectomy versus mastectomy. It should also be part of every discussion about prophylactic mastectomy. The knowledge of reconstruction options gives patients the information they need to make an educated decision about their choices in breast cancer therapy. The federal law mandating that insurance companies cover mastectomy be required to also cover reconstruction should alleviate patient concerns over the cost of reconstruction.1
The choices for breast reconstruction are numerous and involve many factors. Breast reconstruction involves either volume replacement (e.g., implant or autologous breast reconstruction) or volume-displacing procedures (e.g., local tissue rearrangement for partial mastectomy defects). In addition, breast reconstruction can be further categorized into (1) immediate versus delayed reconstruction and (2) prosthetic versus autologous reconstruction. It is important for health care providers to know that there is no single best choice for breast reconstruction. Each patient has a best option based on her needs, wishes, and the size and shape of her breast. Ultimately, the decision regarding the optimal type of breast reconstruction for an individual should be made between the patient and the reconstructive surgeon. The need for adjuvant therapy and the desire to augment the contralateral breast in unilateral mastectomy are also important factors in determining the best option for patients. All of these issues, the risks and benefits of each, and the expectations of the patient should be fully discussed with a plastic surgeon before a decision is made about the type of breast reconstruction.
The options for patients who choose breast reconstruction have increased over the last four decades. Implant reconstruction has been available since the 1960s, and the cosmetic results have improved with new plastic surgery techniques and improvements in newer generation of breast implants. In the 1970s and 1980s, pedicled flaps were developed and used in breast reconstruction. Over the last two decades, advancements in microsurgical techniques have led to free tissue flaps and perforator tissue flaps in which a portion of the body and its blood supply are detached, transferred to the chest, and reconnected to blood vessels at the recipient site. These advancements have helped to reduce donor site morbidity and to increase the options for patients pursuing breast reconstruction.
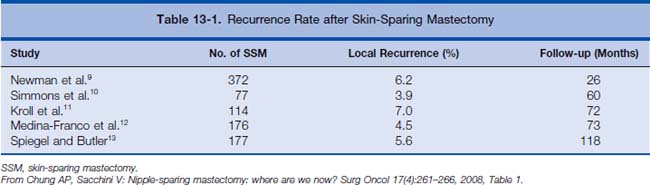
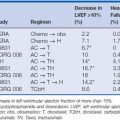
Regardless of the reconstruction method, the technique used during mastectomy is important in achieving adequate symmetry. Maintaining the skin envelope and the inframammary fold guides size and preserves landmarks for breast positioning. Three types of mastectomy techniques allow this. Skin-sparing mastectomy is resection of the breast tissue and the nipple-areola complex that still preserves the breast skin envelope and inframammary fold. Areola-sparing mastectomy is similar, but also preserves the areola with resection of the nipple. Subcutaneous mastectomy, which is offered in prophylactic mastectomy, preserves the entire nipple-areola complex. Note that skin-sparing mastectomy does not increase the incidence of local recurrence rates when compared with simple mastectomy7,8 (Table 13-1).
Immediate versus Delayed Reconstruction
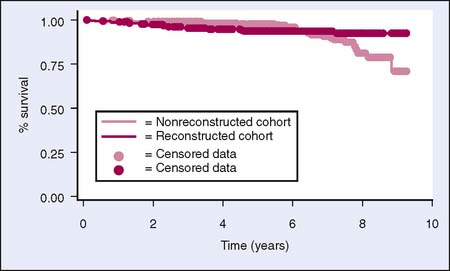
The decision to have immediate reconstruction after mastectomy involves the preference of the patient, the availability of the plastic surgeon, and the anticipated postoperative chemotherapy and radiation therapy that are part of the oncologic treatment. Immediate breast reconstruction has been shown to be cost-effective, to have psychological and cosmetic benefits, and not to increase operative or oncologic risk.3 Patients who receive immediate reconstruction feel that it aids in the emotional healing of mastectomy. It leads to improved self-esteem, sexuality and femininity, and less depression.4,14 It also improves postoperative breast symmetry and sensation.15 It is important that immediate reconstruction does not increase the risk of local recurrence or difficulty with surveillance16,17 (Fig. 13-2). It has also been shown not to delay further treatment of breast cancer.18
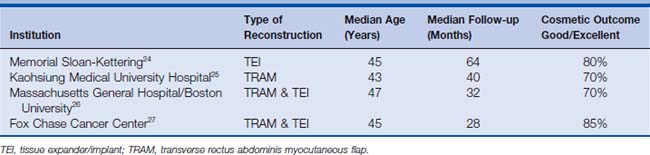
Patients with a relative contraindication to immediate breast reconstruction are patients who will receive postoperative radiation as part of their oncologic treatment. Radiation therapy after implant reconstruction has been shown to cause increased rates of severe capsular contracture and overall increased perioperative complications, including infections and exposure of the implant.19,20 In addition, studies have also demonstrated that autologous breast reconstruction leads to poorer aesthetic outcomes and higher complications in patients receiving postmastectomy radiation after immediate reconstruction compared with those with delayed reconstruction21–23 (Table 13-2). In one study comparing immediate and delayed free TRAM (transverse rectus abdominis myocutaneous) reconstruction in patients receiving postmastectomy radiation, the authors found that the incidence of late complications was significantly higher in the immediate reconstruction group compared with the delayed reconstruction group.23 Overall, close to one third of patients in the immediate reconstruction group required an additional flap to correct the radiation-induced distortion from flap shrinkage and contraction.23
Oftentimes, if it is unclear whether the patient will require postmastectomy radiation, immediate tissue expanders can be placed at the time of the mastectomy. After review of permanent sections, a determination is made about whether postmastectomy radiation is needed. If radiation therapy is needed, standard delayed reconstruction is carried out. However, if no radiation therapy is necessary, then the reconstructive surgeon will proceed with definitive breast reconstruction. Using this delayed-immediate approach allows patients who do not need postmastectomy radiation to achieve aesthetic results comparable to immediate breast reconstruction without significant sequelae.28
Prosthetic Reconstruction
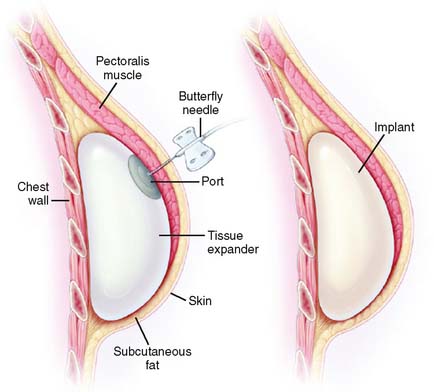
Prosthetic implant reconstruction is the most common form of breast reconstruction in the United States (Fig. 13-3). Implant reconstruction is appealing to patients who do not want autologous tissue removed from other portions of their body. It is also the recommended method for thin women who do not have adequate tissue volume in potential donor sites. Implant reconstruction requires a shorter operation and gives a good cosmetic result with symmetry, but usually requires a two-stage operation. The first operation is the placement of a tissue expander. This is a submuscular implant that can be placed immediately after mastectomy. It has a port that can be serially inflated during postoperative office visits (Fig. 13-4). The expander is inflated to a size symmetric to the contralateral breast—or in the case of bilateral mastectomy with reconstruction—to the patient’s desired size. When the desired size is reached, the expander is exchanged for the implant in a second operation.
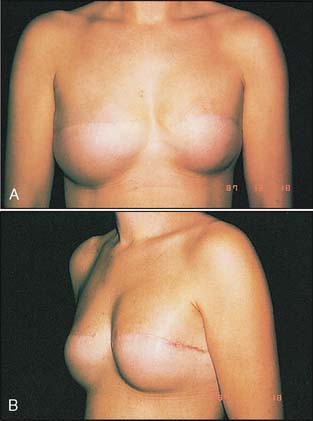
Figure 13-3 Frontal and side views of a patient after bilateral implants.
(From Eberlein TJ, Tsangaris TN: Breast cancer surgery. In Hayes DF (ed): Atlas of Breast Cancer, 2nd ed. London: Mosby, 2000, Figure. 6.23.)
The disadvantages of implant reconstruction are mostly due to foreign body implant. Early after implant placement, patients may develop exposure, extrusion, or infection of the implant. Implant contracture, rupture, rippling, migration, or pain may also develop over time with breast implants. The overall complication rate for implant reconstruction in a nonirradiated breast is less than 10%.29 In patients who undergo postoperative radiation, this rate increases to 18% to 50%.29,30 A recent study identified smoking, obesity, hypertension, and age over 65 as independent risk factors for perioperative complications after expander/implant breast reconstruction.31 Significantly, active smokers were twice as likely to develop perioperative complications and five times more likely to fail reconstruction compared to non-smokers31 (Table 13-3).
Table 13-3 Factors Associated with Poor Outcome with Tissue Expander/Implant Reconstruction
| Risk Factor | Relative Greater Risk of Complications | Relative Greater Risk of Implant Failure |
|---|---|---|
| Smoking | 2.2 | 4.9 |
| Age over 65 years | 2.5 | NS |
| Obesity | 1.8 | 6.9 |
| Hypertension | 1.8 | 4.3 |
From McCarthy CM, Mehrara BJ, Riedel E, et al: Predicting complications following expander/implant breast reconstruction: an outcomes analysis based on preoperative clinical risk. Plast Reconstr Surg 121(6):1886–1892, 2008.
The two options for implants that patients can choose from are saline and silicone gel. The Food and Drug Administration (FDA) put a moratorium on silicone gel implants in 1992 and allowed their use only in breast reconstruction patients who entered a clinical trial. This was due to concerns that silicone gel implants cause other medical problems. Studies now have proved that these implants do not increase the risk for patients to develop cancer or connective tissue diseases.32–38 As a result of these findings, the FDA lifted this restriction in November 2006. Silicone gel implants are now being evaluated in post-approval studies to confirm their safety.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree