Fig. 1.1
Key breast MRI pulse sequences. Thirty-nine year old woman presents for breast MRI to evaluate extent of disease for known invasive ductal carcinoma of the left breast (arrow). Basic sequences include three-plane localizer sequence (a), fluid-sensitive sequence (in this case, fast spin echo T2-weighted image with fat saturation) (b), non-fat suppressed T1- weighted sequence (c), multiphase dynamic contrast-enhanced T1-weighted series with representative pre-contrast (d) and first post-contrast (e) images presented. Note the enhancing mass (arrow), which represents the biopsy-proven invasive ductal carcinoma, with susceptibility artifact within, representing a biopsy marker clip. A silicone-weighted series (f) was also obtained in this woman with pre-pectoral silicone implants
Of the above sequences, the 3-plane localizer, T2-weighted sequence, and T1-weighted multi-phase (DCE) sequences (including a pre-contrast and an early and delayed post-contrast series) are required by the ACR Breast MRI Accreditation Program [9]. Although optional from an ACR accreditation standpoint, most complete breast MR examinations also include a non-fat suppressed T1-weighted sequence. Furthermore, a silicone sensitive sequence should also be obtained in women with silicone breast implants. The role and optimization of each individual sequence is discussed in detail below.
For all sequences except the three-plane localizer, the frequency encoding gradient is applied in the anterior-posterior (AP) direction to minimize artifacts due to cardiac motion that would project into the breasts and simulate or obscure suspicious enhancement if the phase encoding direction was AP [10]. Thus, for sagittal acquisition the preferred phase encoding direction is superior—inferior and for axial acquisition the preferred phase encoding direction is left–right.
1.3.1 Three-Plane Localizer
A scout or three-plane localizer is required on all systems to localize the breasts. This allows the technologist to select the appropriate FOV for the patient’s anatomy and scan acquisition plane (FOV considerations are discussed in more detail above).
1.3.2 T2-Weighted (Fluid-Sensitive) Sequence
A fluid-sensitive, typically T2-weighted, sequence is important for improved characterization of lesions and benign findings in the breast. For example, simple cysts, lymph nodes, and some fibroadenomas have high signal on the T2-weighted images. There are multiple acceptable sequence types for fluid-sensitive imaging. The most common are spin echo (SE), fast spin echo (FSE), and short tau inversion recovery (STIR) with an inversion time selected to null fat. These sequences are typically acquired as multi-slice 2D acquisitions because of the long repetition times required for T2-weighting and resulting longer acquisition times, which are more prohibitive for three dimensional (3D) imaging [10]. Thus, the T2-weighted images are typically unable to achieve spatial resolution equivalent to the T1-weighted sequences in a reasonable scan time with adequate SNR. Most protocols utilizing SE or FSE technique for T2-weighted imaging also perform fat suppression in order to readily differentiate bright fluid signal from fat. However, others choose to perform T2-weighted images without fat suppression because it can allow for acquisition of higher spatial resolution images and/or decreased scan times.
1.3.3 Non-fat Suppressed T1-Weighted Sequence
If active fat suppression is used for the DCE sequences (discussed below), it is recommended to perform an additional T1-weighted sequence without fat suppression prior to the multi-phase T1-weighted sequences. The sequence is fast, provides an overview of breast anatomy, can aid in assessing the amount of fibroglandular tissue in the breast, and is helpful in distinguishing fat from water-based tissues (such as fibroglandular tissue, breast lesions, etc.). Additionally, this sequence can aid in the identification of fat containing lesions, which is important because lesions containing fat (e.g. fat necrosis) are typically benign. This sequence should be performed with similar parameters and spatial resolution as the multi-phase T1-weighted sequences (as described below), but without active fat suppression, which allows for comparison of lesion characteristics across all the T1-weighted sequences.
1.3.4 Multi-phase T1-Weighted Sequences
The pre-and post-contrast multi-phase T1-weighted MRI images sequences are the most important images for identifying and characterizing lesions. It is imperative that identical scan parameters be used for the multi-phase T1-weighted images so that image registration can be performed, the pre-contrast images can be subtracted from the post-contrast images, and signal differences between sequences can be directly compared. Subtraction images are particularly useful for identifying signal from gadolinium contrast agents and are mandatory if active fat suppression is not utilized so that contrast-enhancement can be readily differentiated from the bright signal of fat (described further below).
The multi-phase T1-weighted images are used for lesion detection, assessment of lesion morphology, and evaluation of lesion contrast enhancement over time. Characterizing lesion morphology, such as shape, margin, and internal enhancement pattern, requires high spatial resolution images with in-plane resolution of ≤1 mm to depict fine features, such as lesion margins. Through-plane slice thickness should be ≤3 mm; however, thinner slices that approach in plane resolution size (i.e. closer to isotropic) decrease volume averaging in the through-plane direction, which can increase the contrast of small lesions compared with background tissue. Additionally, thin slices facilitate higher quality image reformats, eliminating the need to acquire additional images in different planes (discussed further below). Conversely, voxel size should not be so small that SNR suffers.
A 3D GRE pulse sequence is preferred for multi-phase T1-weighted imaging with a short TR. The GRE pulse sequence should be spoiled to avoid any confounding T2 contrast [11]. There are no consensus guidelines for the number of post-contrast acquisitions or total acquisition time for the multi-phase T1-weighted sequences, although at least two post-contrast sequences should be performed in order to allow for the most basic assessment of contrast enhancement kinetic features. Invasive cancers typically enhance early, peaking in enhancement approximately one to two minutes after contrast injection. Although breast cancers more frequently exhibit initial fast enhancement (increase in signal from pre-contrast to first post-contrast series of >100 %) and delayed washout (decrease in signal from first post-contrast to final post-contrast series of >10 %) than benign findings, there remains substantial overlap in the kinetics of malignant and non-malignant lesions of the breast [12]. The multi-phase T1-weighted MRI protocol should be constructed so that one of the early-phase post-contrast sequences will sample the high frequency data at the center of k-space (which defines image contrast) between one and two minutes. This is important to potentially capture the peak enhancement of invasive cancers, but also to differentiate lesions from benign BPE, which typically increases over time (Fig. 1.2). For the majority of Cartesian sequences with rectilinear k-space sampling, the center of the sequence captures the high frequency data. However, Cartesian sequences with elliptical centric k-space sampling and other k-space sampling trajectories, such as radial, may acquire the center of k-space near the beginning of the sequence. Knowledge of the sampling pattern is thus important to properly time the post-contrast sequences.
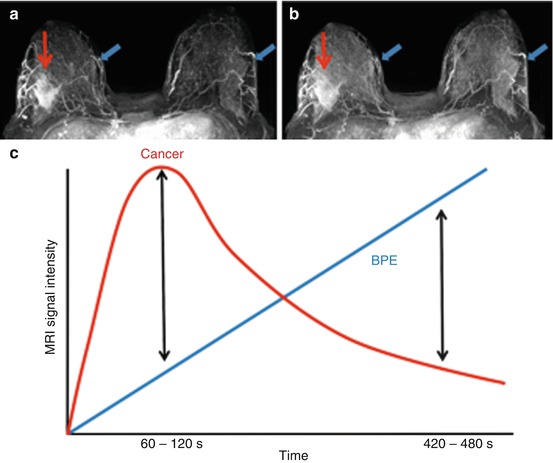
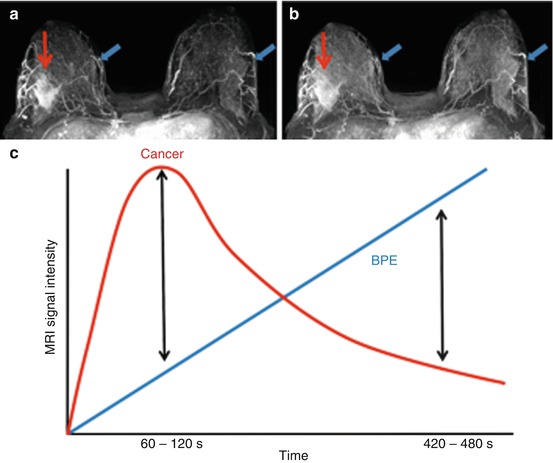
Fig. 1.2
Lesion conspicuity based on dynamic contrast enhanced (DCE) imaging timing. Early-phase 3D subtraction MIP images obtained in the early-phase post-contrast between 60–120 s (s) (a) demonstrates the patient’s outer posterior right breast cancer (red arrow), easily differentiated from the moderate benign background breast parenchymal enhancement (BPE, blue arrow). Delayed-phase 3D subtraction MIP image obtained between 420–480 s demonstrates that the cancer (red arrow) is less conspicuous because it has begun to washout while BPE (blue arrows) has increased in both breasts (b). Since in general, cancers tend to washout over time while BPE tends to increase (c), it is recommended that early phase DCE images be utilized for breast cancer detection
1.3.5 Silicone Implants
Silicone, like water, has a longer T2 relaxation time than fat. Thus, on a standard T2-weighted sequence without fat suppression, water will be brighter than silicone, which is brighter than fat [13]. For evaluation of silicone implant rupture, it is often ideal to have a sequence that suppresses both the water and fat, leaving silicone as the only material remaining bright on imaging. This is possible using a T2-weighted FSE pulse sequence with water suppression and an inversion pulse with an inversion time to null fat [13].
1.4 Balancing Spatial and Temporal Resolution
High spatial resolution and high temporal resolution are typically competing demands of MR acquisition. High spatial resolution imaging results in longer scan times, decreasing the temporal resolution. High spatial resolution is critical for accurate assessment of lesion morphologic features, but high temporal resolution is necessary for accurate depiction of lesion enhancement curves over time. Studies have shown that when forced to compromise, spatial resolution and accurate depiction of lesion morphology is more important to diagnostic accuracy than characterization of the signal enhancement curve. Thus, when creating a breast MRI protocol, spatial resolution is often prioritized over temporal resolution [14].
In general, the compromises between spatial and temporal resolution have decreased with state-of-the art MR systems and breast coils. The ACR Breast MRI Accreditation Program [9] requires that the early-phase post-contrast sequence be completed by four minutes after contrast injection; however, three minutes or less is most desirable [14, 15] and should be achievable without difficulty on modern scanners. Parallel imaging is now standard on modern MRI systems and also helps to shorten scan times [16–19]. There has been much research in recent years to develop novel accelerated MRI acquisition techniques to provide simultaneously high spatial and high temporal resolution scans. These include techniques such as novel k-space sampling schemes and reconstruction using high spatial frequency k-space data from adjacent time frames (view-sharing) [20–23]. Some of these methods are being used to obtain hybrid high spatiotemporal resolution imaging protocols [24, 25], although their exact benefit in the routine clinical setting is not known.
1.5 Methods of Fat Suppression
Either passive (image subtraction) or active removal of fat from the DCE MR images is necessary to ensure detection of contrast-enhancement separate from the bright signal of fat. The benefit of utilizing subtraction for fat suppression is that it allows for higher temporal resolution as well as potentially more complete fat suppression since it does not rely on B0 homogeneity and shimming. Relying only on image subtraction for detection and characterization of enhancing lesions also has drawbacks—misregistration resulting from interscan motion can result in “pseudoenhancement” and lead to diagnostic errors. Furthermore, subtracted images are prone to degradation of image quality [26]. Thus, it is the authors’ preference to perform active fat suppression for the T1-weighted DCE MRI images and additionally perform image subtraction. Using this approach allows an examination to be interpreted solely from the acquired T1-weighted fat suppressed images if the subtraction images are degraded by motion artifact.
Multiple methods exist for active fat suppression, exploiting the small differences in resonant frequency between lipid and water protons and/or the difference in T1 relaxation times between adipose tissue and water to suppress the fat signal. Intermittent fat suppression with a frequency selective fat saturation pulse to eliminate fat signal is commonly employed for T2-weighted SE and FSE sequences and T1-weighted GRE sequences. Inversion pulses and water only excitation pulses are also possibilities. More recently, fat-water separation techniques such as two-point Dixon based methods [27], including Iterative Decomposition of water and fat with Echo Asymmetry and Least squares estimation (IDEAL) [28], have become more common. These methods acquire multiple echo times (two or more) allowing separation of water and fat and result in water-only and fat-only images. A longer minimum TR is required to acquire the multiple echo times, thus acquisition time is longer. However, uniform suppression of fat signal is challenging in breast MRI due to B0 inhomogeneity given the complex anatomy and variation in tissue types across the FOV. Dixon methods improve the robustness of fat removal in the presence of B0 inhomogeneity [29]. Additionally, Dixon methods also provide fat-only images, eliminating the separate non-fat suppressed T1-weighted MRI acquisition and saving overall scan time.
1.6 Image Reformats
Subtraction of post-contrast images from the pre-contrast T1-weighted images is required to remove bright signal from fat (if active fat suppression is not used) so that contrast-enhancing lesions can more easily be seen. However, regardless of the use of active fat suppression for the DCE MR images, the use of image subtraction can be helpful since it removes non-enhancing fibroglandular tissue and other non-enhancing anatomy (besides adipose tissue), enabling easier visualization of potential suspicious areas of contrast enhancement. Subtraction images are most valuable for accentuating enhancing lesions that are evident on the early-phase (for the same reasons described above) DCE images, but can be performed for any of the post-contrast sequences by simply subtracting the pre-contrast images’ signal from the desired post-contrast images. One of the most commonly used subtraction reformats is a 3D subtraction maximum intensity projection (MIP) that is created from an individual subtraction series (most frequently the first post-contrast DCE series). The MIP is valuable clinically as an “overview” image that allows for quick assessment of symmetry, BPE, and the presence of suspicious findings.
If the acquired images have sufficient spatial resolution and thin slices, multi-planar reformats (MPRs) can be performed (Fig. 1.3). MPRs allow suspicious findings to be evaluated in multiple planes, aiding detection and characterization, as some lesion types such as non-mass enhancement can be at times easier to detect in a second plane. Also, creation of MPRs eliminates the need to acquire additional sequences in perpendicular planes, saving overall scan time.
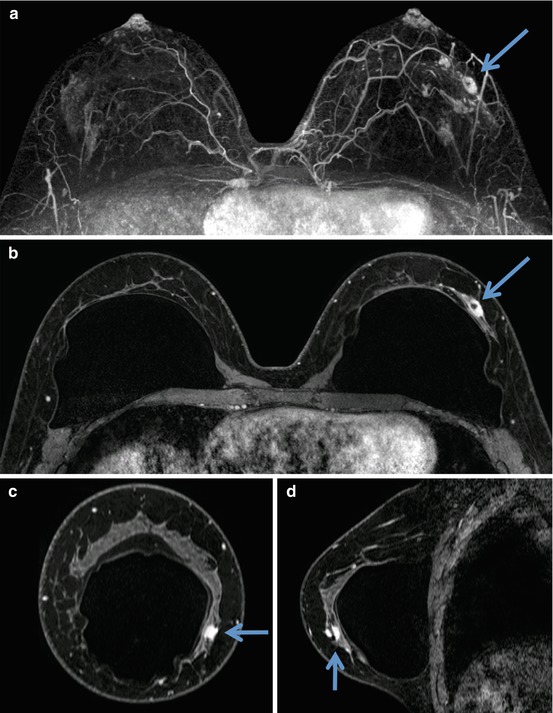
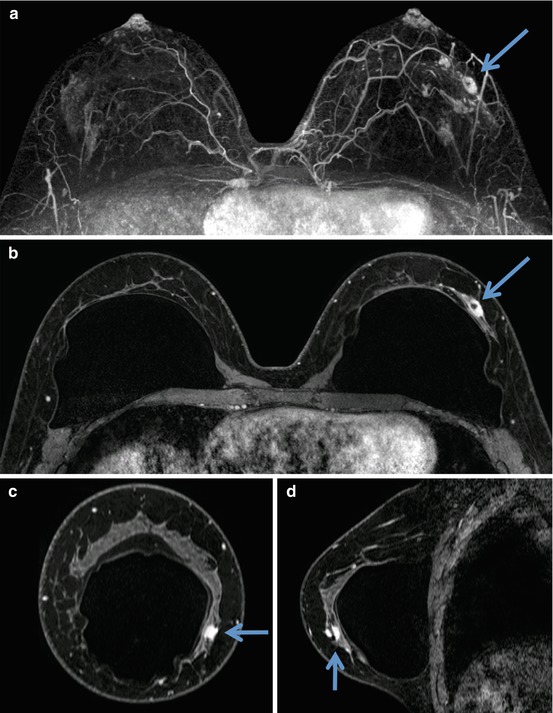
Fig. 1.3
Subtracted maximum intensity projection (MIP) and multi-planar reformats (MPRs) in a 39 year old patient with biopsy proven left invasive ductal carcinoma (arrows, same patient as in Fig. 1.1). Patient with biopsy-proven invasive ductal carcinoma (arrow) with evidence of multifocal malignancy on MIP (a). Known malignancy is evident as a mass (arrow) on the source first post-contrast T1-weighted dynamic contrast enhanced (DCE), which was acquired in the axial plane (b). Multi-planar coronal (c) and sagittal (d) reformats from the source first post-contrast DCE image (a) provide improved characterization and localization of the known malignancy
1.7 Attaining Consistency and Addressing Challenges
There are inherent challenges to performing breast MRI that must be addressed to obtain consistent high quality breast MR examinations. First and foremost, a quality breast MRI program includes highly trained technologists who regularly perform breast MRI and are comfortable with appropriate patient positioning and communication. Protocol sequences and sequence timings should be as consistent as possible from patient to patient, regardless of breast size or body habitus. However, the FOV can be adjusted for body habitus for image optimization and reduction of artifact as needed. Finally, there are technical and physical challenges to obtaining high quality breast MRI, some of which are accentuated at higher magnetic field strength, which require attention and are discussed in greater detail below.
1.8 Artifacts
Imaging artifacts can occur in breast MRI scans from a variety of sources. Such artifacts are important to recognize as they can cause misinterpretation by obscuring and/or mimicking pathology. Several of the most common artifacts affecting clinical breast MRI are summarized here.
1.8.1 Motion Artifacts
Both physiologic and non-physiologic movement during image acquisition can cause artifacts. Sources of physiologic motion commonly impacting breast MRI are blood flow and vessel pulsation, respiration, and cardiac motion. Motion artifacts propagate in the phase-encoding direction; therefore, the direction of the phase-encoding gradient must be selected to minimize detrimental effects of such motion on the diagnostic quality of the images. In order to minimize physiologic motion artifacts across the breasts, the phase-encoding gradient should be left—right for axial imaging and superior—inferior for coronal or sagittal imaging (Fig. 1.4).
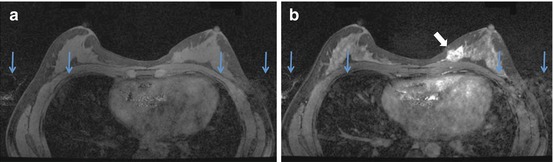
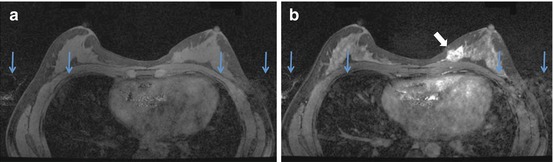
Fig. 1.4




Cardiac motion artifact evident in the phase encoding direction on 1.5 T MR images in a 38 year old woman with a newly diagnosed invasive cancer in the left breast. Pre-contrast (a) and initial phase (b) post-contrast T1-weighted MR images (axial primary acquisition) demonstrate cardiac motion artifact in the phase encoding (right—left, vertical blue arrows) direction in a 44 year old patient with known invasive ductal carcinoma (angled white arrow) in the left breast. Note that due to gadolinium concentrating in the heart and great vessels, this effect is accentuated on the post-contrast images (b). Alternate selection of anterior-posterior as the phase encoding direction could cause the cardiac motion artifact to overlay and obscure much of the lesion and surrounding area. As a result, it is recommended that the phase encoding direction be left—right for primary axial acquisitions and superior—inferior for primary sagittal or coronal acquisitions
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree