Despite strong evidence supporting the use of breast conservation therapy (BCT) in the treatment of breast carcinoma, the actual rates of use remain low. This article is a retrospective review of a sample of patients from the cancer registry of the Carolinas Medical Center (CMC), comparing breast conservation and mastectomy rates during an 11-year period. BCT rates have increased in CMC during this time frame and have reached national levels. Further research is needed to determine whether BCT rates can be used as a benchmark for the care of patients with cancer.
The beginning of the twenty-first century saw the further disappearance of surgical procedures such as the Halsted radical mastectomy, which the newest generation of surgeons will never see, much less perform, except in the occasional rare circumstance. The publication of several prospective, randomized studies demonstrating no difference in survival between mastectomy and breast-conserving surgery, coupled with the paradigm shift to breast carcinoma being considered a systemic disease at the time of diagnosis, led to the promulgation of breast conservation surgery combined with local radiotherapy as a valid treatment modality. Low rates of breast conservation therapy (BCT) were initially reported with what seemed to be a slow gain in acceptance of the practice across the United States. A multitude of reasons, ranging from surgeon preference to limited access to radiation facilities, were found to influence the choice of surgery in the treatment of early-stage breast cancers. Whereas more recent studies have noted a much higher rate of BCT, at least one study found mastectomy rates increasing for women with stage I and stage II cancers.
Regional differences have been detected in the use of BCT since its inception. Studies in the 1990s found that women in the northeast United States had much higher rates of BCT than those in the southeast, southwest, or midwest. The south, in particular, has stood out as having one of the lowest rates of BCT. A statewide analysis of North Carolina on the rates of BCT for 6 years found that the rates of BCT range from 7.3% in 1988 to 14.3% in 1993. The reasons cited in the literature for this variation included regional differences in both physician attitudes and patient preferences, as well as older patient age; however, over time, this discrepancy has somewhat diminished.
Most cases of breast cancer in the United States are treated in the community setting. Of the more than 1500 programs accredited by the Commission on Cancer, a consortium established by the American College of Surgeons in 1922 dedicated to improving survival and quality of life for patients with cancer, approximately 70% were community based. The Carolinas Medical Center (CMC), located in Charlotte, North Carolina, is one of the major teaching hospitals in the state with 11 different residency programs and many fellowship training programs. A large academic community hospital and tertiary referral center, CMC treats a large number of patients with breast carcinoma each year. Of the 29,458 new cases of cancer at CMC between 1999 and 2009, breast cancer cases made up almost one-fifth of the total. The authors conducted a retrospective review of the hospital cancer registry to analyze whether mastectomy and BCT rates had changed over the past 11 years at CMC and to determine the factors that may have contributed to this change.
Methods
The study was conducted at CMC, an 874-bed community hospital. CMC is part of the Carolinas HealthCare System that includes 32 affiliated hospitals in North and South Carolina. The North Carolina Central Cancer Registry collects, processes, and analyzes data on all cancer cases diagnosed among North Carolina residents. Reporting this information is mandatory for all health care providers, although most of the data are furnished by hospitals. The CMC Cancer Registry was established in July 1987 and initially collected data only from the main hospital. The registry obtained network status during the Commission on Cancer accreditation program in 2004 and was expanded to include cancer data from other hospitals in the Carolinas HealthCare System.
The CMC tumor registry was queried to identify patients diagnosed with breast carcinoma from January 1, 1999, through December 31, 2009, who underwent their initial surgical therapy at the main hospital. A sample of approximately one-fourth of the cases identified was reviewed. From this sample, the authors excluded patients who did not complete definitive surgical therapy by December 31, 2009, and those patients with cancers that did not fall within the American Joint Committee on Cancer (AJCC) staging guidelines. Demographic, clinical, and treatment variables of patients were recorded, including age at diagnosis, race, sex, marital status, date of treatment, clinical and pathologic staging, type of surgery, and location of surgery. The clinicopathologic variables recorded included tumor malignancy type, tumor size, histologic subtype, location of tumor, nodal status, and metastatic status.
The study population included women diagnosed with AJCC stage 0, stage I, or stage II breast cancer, who had undergone either BCT or mastectomy. Clinical staging was used in decision making for classification of patients unless full pathologic staging was available. Breast conservation procedures included lumpectomy, quadrantectomy, partial mastectomy, and segmental mastectomy. Mastectomy procedures included simple (total) mastectomy, modified radical mastectomy, radical mastectomy, and bilateral mastectomy. Surgical treatment was categorized by the intent to treat. Patients who underwent BCT initially but later went on to have mastectomy as their definitive procedure were placed in the BCT category.
Descriptive statistics including either mean and standard deviations or counts and percentages were calculated. For data measured on the interval scale, the Student t test was used. If the data were ordinal or not normally distributed, the Wilcoxon rank sum test was used. For nominal data, the chi-square test or the Fisher exact test was used. SAS, version 9.2, was used for all analyses. A 2-tailed P value of less than .05 was considered statistically significant. A multivariate logistic regression, with whether a mastectomy or BCT was performed as the independent variable, was conducted to determine the selection criteria for mastectomy.
Results
The tumor registry identified a total of 4799 patients diagnosed with breast carcinoma between 1999 and 2009, from which the authors took a sample of 1199 patients for their analysis ( Table 1 ). However, 228 patients were excluded from the analysis (exclusion criteria included male patients; patients with stage III or stage IV breast cancer; patients who did not complete definitive surgery by December 31, 2009; and those who underwent surgical procedures other than BCT or mastectomy). Some of the patients met the criteria for more than 1 exclusion category. The remaining 971 patients were women with AJCC stage 0, stage I, or stage II breast carcinoma, who underwent BCT or mastectomy, and they were the study population for the analysis.
| Characteristic | No. of Cases (%) |
|---|---|
| Sex | |
| Female | 1186 (98.9) |
| Male | 13 (1.1) |
| Menopausal status (age, y) | |
| <55 | 572 (47.7) |
| ≥55 | 627 (52.3) |
| Race a | |
| White | 950 (79.2) |
| Black | 194 (16.1) |
| Other | 16 (1.3) |
| Marital status b | |
| Single | 156 (13.0) |
| Married | 742 (62.0) |
| Separated/divorced | 123 (10.3) |
| Widowed | 136 (11.4) |
| Tumor size (cm) c | |
| <2 | 606 (61.3) |
| 2–5 | 315 (31.9) |
| >5 | 67 (6.8) |
| Histologic subtype d | |
| Ductal | 934 (78.0) |
| Lobular | 83 (6.9) |
| Ductal and lobular | 49 (4.1) |
| Mixed | 30 (2.5) |
| Other | 102 (8.5) |
| Location | |
| Upper outer quadrant | 427 (35.6) |
| Upper inner quadrant | 126 (10.5) |
| Lower outer quadrant | 127 (10.6) |
| Lower inner quadrant | 70 (5.8) |
| Central/nipple | 47 (3.8) |
| Overlapping lesion | 286 (23.9) |
| Other (NOS, axillary tail) | 116 (9.7) |
| Grade e | |
| Well differentiated | 207 (20.0) |
| Moderately differentiated | 506 (48.9) |
| Poorly differentiated | 321 (31.0) |
| AJCC stage f | |
| Stage 0 | 244 (21.2) |
| Stage I | 463 (40.3) |
| Stage II | 325 (28.2) |
| Stage III | 88 (7.7) |
| Stage IV | 29 (2.5) |
Patient and tumor characteristics of the study population are detailed in Table 2 . BCT was performed in 75% of the patients. Mean age at diagnosis for the BCT group was 57.3 years compared with 54.1 years for the mastectomy group (range, 26–95 years; P = .0008). Postmenopausal women (older than 55 years) made up 55.2% of the BCT group. More than 78% of the total number of women older than 55 years underwent BCT as opposed to 71% of women younger than 55 years. The racial makeup in the BCT group was 81.7% white, 14.6% black, and 3.7% other ethnic categories. The mastectomy group had 82.5% white, 16.3% black, and 1.3% other ethnic categories. Most of the tumors in the BCT group were small (71.9% of cases vs 47.1% in the mastectomy group). Conversely, the mastectomy group had tumors that were predominantly in the larger size ranges; 47.6% in the 2 to 5 cm range and 5.2% in the larger than 5 cm group. Ductal tumors were the most represented histologic subtype in both the groups (78.8% in the BCT group and 76.7% in the mastectomy group). A histologic grade was assigned to 89.1% of cases, and 25.2% were well differentiated in the BCT group compared with 14.3% in the mastectomy group. Poorly differentiated tumors accounted for 39.2% of the mastectomy group. Stages 0 and I carcinomas were more common in the BCT group (combined total of 70% of cases) and represented only half of the cases in the mastectomy group.
| Characteristic | No. of Cases | P Value | |
|---|---|---|---|
| BCT (%) (n = 721) | Mastectomy (%) (n = 240) | ||
| Menopausal status (age, y) | |||
| <55 | 323 (44.8) | 132 (55.0) | .0061 |
| ≥55 | 398 (55.2) | 108 (45.0) | |
| Mean age at diagnosis (y) | 57.3 | 54.1 | .0008 |
| Race | |||
| White | 589 (81.7) | 198 (82.5) | .1390 |
| Black | 105 (14.6) | 39 (16.3) | |
| Other | 27 (3.7) | 3 (1.3) | |
| Marital status a | |||
| Single | 83 (11.5) | 32 (13.4) | .0576 |
| Married | 461 (64.1) | 150 (62.8) | |
| Separated/divorced | 69 (9.6) | 29 (12.1) | |
| Widowed | 88 (12.2) | 25 (10.5) | |
| Tumor size (cm) b | |||
| ≤2 | 455 (71.9) | 99 (47.1) | <.0001 |
| 2–5 | 161 (25.4) | 100 (47.6) | |
| >5 | 17 (2.7) | 11 (5.2) | |
| Histologic subtype c | |||
| Ductal | 567 (78.8) | 184 (76.7) | .04876 |
| Lobular | 45 (6.3) | 19 (7.9) | |
| Ductal and lobular | 28 (3.9) | 13 (5.4) | |
| Mixed | 17 (2.4) | 8 (3.3) | |
| Other | 63 (8.8) | 16 (6.7) | |
| Location | |||
| Upper outer quadrant | 264 (36.6) | 79 (32.9) | .6612 |
| Upper inner quadrant | 93 (12.9) | 22 (9.2) | |
| Lower outer quadrant | 78 (10.8) | 32 (13.3) | |
| Lower inner quadrant | 47 (6.5) | 15 (6.3) | |
| Central/nipple | 25 (3.5) | 12 (5.0) | |
| Overlapping lesion | 158 (21.9) | 58 (24.2) | |
| Other (NOS, axillary tail) | 56 (7.8) | 22 (9.2) | |
| Grade d | |||
| Well differentiated | 161 (25.2) | 31 (14.3) | <.0001 |
| Moderately differentiated | 317 (49.5) | 101 (46.5) | |
| Poorly differentiated | 162 (25.3) | 85 (39.2) | |
| AJCC stage | |||
| Stage 0 | 176 (24.4) | 43 (17.9) | <.0001 |
| Stage I | 358 (49.6) | 82 (34.2) | |
| Stage II | 187 (25.9) | 115 (47.9) | |
| Lymph node status | |||
| Mean number of nodes examined | 7.5 | 10.6 | <.0001 |
| Mean number of nodes positive | 0.4 | 0.70 | .0002 |
a Unknown or not specified in 24 cases.
A univariate analysis of patient and tumor characteristics in the study population was performed to determine the factors that may be predictive of BCT. Patients with favorable prognostic characteristics such as stage 0 or stage 1, less than 2 cm, and well-differentiated tumors were found to be positively associated with the likelihood of undergoing BCT. Postmenopausal women were found to be more likely to undergo BCT than mastectomy. Race and marital status were not found to be significantly associated with either procedure. Location of tumor and histologic subtype did not show any significance. Positive lymph node status, regardless of the number of positive nodes, was found to be a predictor of mastectomy.
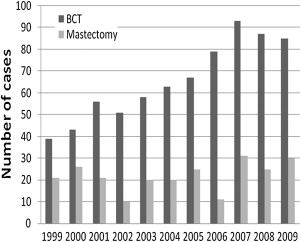
In the 11 years evaluated, there was a steady increase in the number of operations performed at CMC ( Fig. 1 , Table 3 ). The BCT rate increased from 65% in 1999 to 73.9% in 2009, with a peak rate of 87.7% in 2006. The mastectomy rate was cut by almost one-third, dropping from 35% in 1999 to 26% in 2009 ( Fig. 2 ). The BCT rates at CMC in the years 2000 and 2008 were compared with those of both North Carolina and the United States. The BCT rate of 61% at CMC in 2000 was right at the national average of 62%, with North Carolina lagging behind at 54%. By 2008, the rates of BCT had increased to 78%, 64%, and 59%, respectively, with North Carolina BCT rate still less than the national average.