8
BRACHYTHERAPY
8.2 LOW-DOSE-RATE BRACHYTHERAPY
8.3 HIGH-DOSE-RATE BRACHYTHERAPY
Question 2
What are the types of brachytherapy?
Question 3
What are different types of brachytherapy loading systems?
Question 4
What are permanent versus temporary implants in brachytherapy?
Brachytherapy is a special procedure in Radiation Oncology that uses radioactive sources placed at short distances (hence brachy) from the target. Brachytherapy generates highly conformal dose distributions in a target volume because radioactive seeds (or sources) are placed directly within or in the vicinity of the target tissue.
Answer 2
Interstitial brachytherapy—radioactive sources are placed in the target tissue directly either permanently or temporarily.
Intracavitary brachytherapy—radioactive sources are contained in an applicator that is inserted into body cavities such as the vagina or uterus.
Intraluminal brachytherapy—subclass of intracavitary brachytherapy in which the radioactive sources are inserted in the lumen of the patient such as the blood vessel, bronchus, esophagus, or bile duct.
Surface–Radioactive sources (or seeds) are placed in the surface plaques or molds, which are then placed on the treatment area such as the eye or skin.
Answer 3
Manual “hot” loading: used for low dose rate seeds such as prostate or eye plaque.
Manual afterloading: this technique is not frequently used anymore.
Remote afterloading: most frequently used for high dose rate treatment.
Answer 4
Permanent implants—the radioactive sources are permanently implanted into the tumor, the patient is released from the hospital with radioactive materials in them.
Temporary implants—the radioactive material is implanted into or close to the tumor and is removed once the prescribed radiation dose has been delivered.
What are the dose rate ranges for low-, medium-, and high-dose-rate brachytherapy according to International Commission for Radiation Units and Measurements (ICRU) Report No. 38?
Question 6
What radionuclides are currently most used for brachytherapy treatments?
Question 7
What types of radiation are used in brachytherapy?
Question 8
How is radiation source strength typically specified in clinic?
Low-Dose-Rate (LDR): 0.4 to 2.0 Gy per hour—used for permanent and manually afterloaded brachytherapy
Medium-Dose-Rate (MDR): 2 to 12 Gy per hour. Pulsed dose rate (PDR) brachytherapy afterloaders were developed in this dose rate realm to replicate the LDR experience in terms of total treatment duration but with the source exposed in pulses for only 5 to 10 minutes per hour
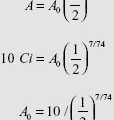
High-Dose-Rate (HDR): more than 12 Gy per hour—HDR brachytherapy utilizes very high activity sources, typically a 10 Ci Ir-192 source. Treatment is delivered by remote-control techniques. The usual dose rate is about 100 to 300 Gy per hour.
Answer 6
Gamma emitters: Cs-137 and Ir-192 for high energy gammas, or I-125 and Pd-103 for low energy gammas
Beta emitters: P-32, Ru-106, Sr-90, and Y-90.
Answer 7
Photons, electrons (betas), and rarely neutrons (Cf-252) and alpha particles are used.
Answer 8
For photon emitters, air kerma strength (U) is commonly used; for electron emitters, Becquerel (usually MBq or GBq) is typically used. Curie (Ci) and mCi are older units that are still commonly used for photon emitters.
You receive an Ir-192 seed with an air kerma strength of 6.25 μGy m2/h. What is the strength of the source in mg-Ra equivalent?
Question 10
The apparent activity for the Ir-192 source is measured to be 20 mCi. Calculate the air kerma strength in cGy cm2/h (The exposure rate constant of Ir-192 is 4.69 R cm2/mCi h).
Question 11
What are the physical states of radionuclides used in brachytherapy?
Question 12
What are the advantages of the high-dose-rate (HDR) brachytherapy compared with low-dose-rate (LDR) brachytherapy?
1 mg-Ra equivalent is defined as 8.25 × 10−4 R/h. Using the Roentgen to rad conversion factor for air 0.876 rad/R and converting Rad (cGy) to μGy, we obtain 8.76 × 103 μGy/R.
Thus 1 mg-Ra eq at 1m = 8.25 × 10−4 R/h × 8.76 × 103 μGy/R = 7.23 μGy m2/h
Dividing the air kerma strength of our source by this conversion factor gives us the result. 6.25/7.23 = 0.864 mg-Ra eq.
Answer 10
Air kerma strength = Exposure rate constant (R cm2/mCi h) × Apparent activity (mCi) × Roentgen to cGy conversion factor for air of 0.876 cGy/R
= 4.69 R cm2/mCi h × 20 mCi × 0.876 cGy/R
= 82.2 cGy cm2/h
Answer 11
Solids, liquids, and gases (Xe-133). Solid sources are sealed (encapsulated in a metal shell).
Answer 12
Out-patient procedure
Safety—reduction or elimination of radiation exposure to the radiation therapy staff
Optimization—moving source allows optimization of the dose distribution by adjustment of the dwell times for each dwell position in each channel (catheter or needle), permitting very fine control of the dose distribution
Stability—HDR intracavitary treatments take less time (usually under an hour), and the movement of the applicators during treatment is minimized.
Dose reduction to normal tissue—shorter duration of HDR treatments allows for physical displacement of normal tissue structure during treatment
Applicator size—the small size of the HDR source permits the use of smaller applicators
What are the disadvantages of the high-dose-rate (HDR) brachytherapy compared with low-dose-rate (LDR) brachytherapy?
Question 14
What are the safety features and operational interlocks of the high-dose-rate (HDR) afterloader?
Question 15
What is the current method for calculating dose rate in tissue from a radioactive source?
Question 16
What is anisotropy with respect to radioactive sources?
Investment—machine’s cost can be anywhere between $1M and $2M.
Radiobiology—as the dose rate increases, the radiosensitivity (damage per unit dose) increases for both normal tissues and tumors, the radiosensitivity for the normal tissue increases faster, increasing the likelihood of injuring the patient while controlling the tumor. Overcoming this requires the use of the advantages of optimization, geometry, stability, and dose reduction to normal tissues, and multiple fractionation treatment.
Safety—if the HDR machine has a malfunction or if a patient has an emergency situation, the risk of accidental radiation exposure to the patient and the staff is much higher in HDR than in LDR.
Answer 14
Audio/visual system
Radiation monitors and treatment on indicator
Door interlock
Emergency shut-offs
Emergency crank
Backup battery
Answer 15
The TG-43 formalism with no heterogeneity corrections is the current standard.
Update of AAPM Task Group No. 43 Report: a revised AAPM protocol for brachytherapy dose calculations. Med Phys. 2004;31:633–674.
Answer 16
Anisotropy refers to the directional dependence of the fluence from a source due to the location of the radioactive material within the source and differences in wall thickness and construction.
Question 18
What instrument would you use to locate a missing source?
Question 19
What instrument would you use to survey a patient before release?
Question 20
What are the requirements regarding calibration of new sources?
Answer 18
A Geiger–Muller (GM) counter.
Answer 19
A sensitive, calibrated ion chamber (eg, one with a large, pressurized gas-filled chamber) is typically used.
Answer 20
New sources must be calibrated before treating patients using a dosimetry system that has a National Institute of Standards and Technology (NIST) traceable calibration. The dosimetry system typically comprises a well-chamber and an electrometer capable of reading in the current mode. For the source activity in mCi range, the typical current readings from the electrometer are on the order of 10−11 A (ampere). For an HDR source (about 10 Ci activity), the current is 10-7 A. This current is then converted into the activity of the source.
What are the corrections applied to the electrometer readings when performing a calibration check?
Question 22
What are the rules regarding a radioactive materials (RAM) inventory?
8.2 LOW-DOSE-RATE BRACHYTHERAPY
Question 1
What isotopes are used for permanent implants and what are the reasons for choosing them?
Question 2
What are the typical dosimetric parameters for a prostate implant?
If the well chamber is open to the atmosphere, as most are, a temperature and pressure correction must be applied. In addition, there may be an electrometer scale reading correction.
Answer 22
The Nuclear Regulatory Commission (NRC) requires a licensee to maintain an inventory log for all radioactive materials. The log must contain the type of source (isotope), source strength, and its location. Permanent sources implanted in a patient are not subject to this inventory control once the patient has been released from the facility.
Answer 1
The isotopes most commonly used are I-125, Pd-103, and Cs-131. They are used because of their low average photon energies (0.028, 0.021, and 0.029 MeV) so that they will treat only the tumor, and have relatively short half-lives (59.4, 17, and 9.7 days).
Answer 2
For I-125, the prescription dose is 144 Gy to cover the prostate delineated on the ultrasound images. V150 (volume of the prostate receiving 150% of the prescription dose of 144 Gy) values ranging from 40% to 50% of the prostate and V200 from 10% to 20% of the prostate are acceptable. Although there may be no explicit margin contoured, the implant volume receiving 144 Gy is approximately twice that of the prostate itself. For Pd-103, the prescription dose is 125 Gy.
Question 4
What is the release criterion for a prostate seed implant patient?
Question 5
What is the purpose of postimplant dosimetry?
Question 6
A patient undergoes a low-dose-rate (LDR) prostate brachytherapy implant with Pd-103 to a prescription dose of 125 Gy. What is the initial dose rate (cGy/h) of the implant?
Per Radiation Therapy Oncology Group (RTOG) protocols, the source is modeled as a point and the anisotropy as a function of distance (r) only with no directional information about seed orientation within the implant.
Answer 4
Per Nuclear Regulatory Commission (NRC) regulations (hence also agreement states), “a licensee may authorize the release from its control of any individual who has been administered unsealed radioactive material or implants containing radioactive material if the total effective dose equivalent to any other individual from exposure to the released individual is not likely to exceed 5 millisieverts (0.5 rem).” For prostate patients, this is satisfied if the exposure rate measured at 1 m from the patient is <1 mR/h.
Answer 5
CT-based postimplant dosimetry is usually conducted roughly 30 days after a prostate seed implant procedure. This allows for gland swelling due to edema to subside. The postimplant dosimetry is primarily performed as a quality assurance measure for the implant procedure. It has also been used for regulatory purposes (ie, defining a “medical event”).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree