and Paul Telfer2
(1)
Department of Haematology, Guy’s and St Thomas’ Hospital, London, UK
(2)
Department of Haematology, Royal London Hospital, London, UK
Avascular Necrosis
Chronic bone damage is one of the most important causes of long-term morbidity. Avascular necrosis (AVN) of the hip is a common complication in adults with HbSS and other genotypes of SCD. AVN of the hip, shoulder or spine results in chronic pain and loss of mobility and function.
Incidence
The incidence of asymptomatic disease is around 26 % in children and 41–80 % in young adults. Symptomatic disease is present in up to 50 % of adults. The hip is the most commonly affected joint followed by the shoulder and spine, and bilateral involvement is common.
Pathogenesis
Vaso-occlusion affecting the blood supply to the bone underlying the articular surfaces leads to ischemia and osteocyte necrosis. The ends of long bones (in particular the femur and humerus) are particularly susceptible to AVN, leading to a loss of structural integrity with eventual collapse of bone. Collapse of the articular surfaces is not reversible and leads to incongruity and severe joint damage. There is also a loss of adhesion between the bone and overlying articular cartilage, which can result in severe musculoskeletal pain.
Clinical Presentation
Patients usually present with increasing joint pain and stiffness. Symptoms may originate with an acute painful crisis which fails to settle. Mild groin pain on mobilization is a common early feature of hip AVN. Later, symptoms progress with pain at rest, night pain and eventually a painful immobile hip.
Asymptomatic shoulder AVN is also common and also tends to progress to a stiff, painful shoulder. The pain occurs initially on movement, but later patients develop rest pain. Although the rate of progression is slower than with hip AVN, one longitudinal study showed that over 80 % of patients had progressive disease during a mean follow-up of 20 years. In the same study over 60 % of patients with symptomatic shoulder disease required surgical intervention.
AVN is also commonly seen in the lumbosacral spine, resulting in back pain and stiffness.
Classification
There are several classifications used to monitor the progression of AVN which for clinical utility can be simplified into (i) precollapse and (ii) collapse. In pre-collapse, plain X-rays are normal or show sclerosis, however, bone infarction is apparent on MRI (Fig. 9.1). The development of subchondral fracture can be demonstrated on X-ray as the ‘crescent sign’. In later stages, collapse is visible on plain X-ray with flattening of the femoral head, osteoarthritic changes and decreased joint space. The most advanced stage is complete joint destruction (Fig. 9.2).
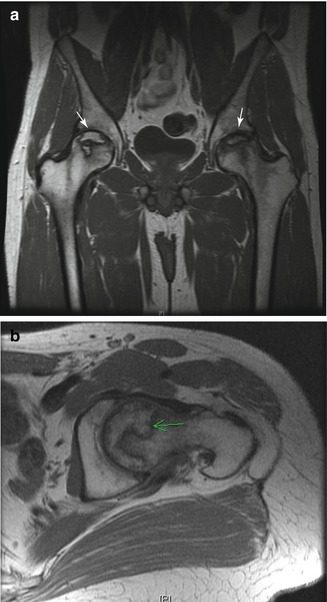

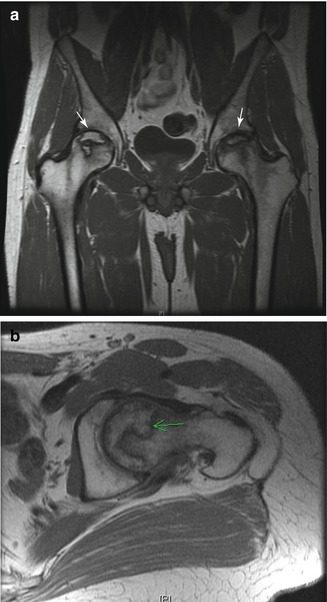
Figure 9.1
(a) MRI showing areas of avascular necrosis in both hips (arrows), but no evidence of collapse. This patient had bilateral hip pain, but hip X-Ray was normal. (b) MRI of the same patient showing an area of avascular necrosis without collapse (arrow)

Figure 9.2
Bilateral advanced AVN. On the right side there is extrusion of the femoral head due to severe collapse and deformity. On the left there is a milder collapse, loss of joint space and a degenerative cyst in the roof of the acetabulum giving further indication of end-stage degeneration
Investigation
Plain X-Ray can be requested for initial investigation of patients presenting with chronic joint pain. If there is radiological evidence of AVN and collapse, no further radiological investigation is necessary. Xray may be normal in early disease and MRI may show the classical appearance of segmental collapse (Fig. 9.1), but may also show multiple small infarcts.
Management
Patients with AVN suffer from chronic musculoskeletal pain. An important goal of management is to develop an effective and acceptable analgesia regime, and this may require input from a chronic pain specialist.
Hip AVN: Early surgical intervention has not been shown to prevent progression, and screening of asymptomatic patients to identify early asymptomatic disease is not currently recommended. The only exception is in patients with AVN of one hip when it may be helpful to identify early AVN in the other. Patients with very early disease may benefit from non-weight-bearing exercise. Surgical core decompression of the hip has been advocated for AVN in other clinical settings, but was not shown to have any advantage over intensive physiotherapy in a randomised trial in SCD, and is not currently recommended as part of routine management for early AVN. It may be useful, however, in selected young patients with early disease (pre-collapse) and can reduce pain and prolong the time before hip replacement surgery is needed.
Once the hip has collapsed, a total hip replacement is usually needed and this should be performed in a center with experience in SCD. Early studies showed a high risk of prosthetic failure, with loosening of the implant and need for revision surgery. There were also high rates of surgical complications, including infection and intra-operative femoral fractures. These complications have reduced as specialist orthopaedic surgeons become more experienced in operating on SCD patients and with use of modern techniques and implants. The best contemporary outcomes have been obtained using cementless ceramic-on-ceramic implants. In one of our centers, the current failure rate is <5 % at 7.5 years.
Shoulder AVN: Early stage disease can be treated with analgesia and physiotherapy, although arthroscopy and decompression may be of benefit. End stage disease requires shoulder hemiarthroplasty. Fewer cases of shoulder AVN need implant surgery because the shoulder is not a weight bearing joint and collapse is less commonly seen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree