There is a wide variation in the recommended minimum interval between donations. For example in the US, in line with World Health Organization (WHO) recommendations, the interval can be as short as 8 weeks and a maximum of 3 litres of blood per year may be collected (American Association of Blood Banks 2003). Premenopausal women should not donate as frequently as men (see below). In the Netherlands, men are bled every 3 months and women every 6 months.
Because few red cells are lost during platelet and plasmapheresis, these procedures may be performed more often and at shorter intervals. Standards vary by country; in the USA plateletpheresis donors may be drawn every 48 h up to twice per week and 24 times per year. Commercial plasmapheresis donors are bled even more frequently; however, physical examination is more rigorous and laboratory testing more extensive for these donors. As combinations of components, such as two-unit red cells, are drawn by apheresis, volumes and intervals become individualized, but generally limited by the loss of red cells.
Effect of Blood Donation on Iron Balance
Failure to meet the Hb standard is the most common reason for donor disqualification and iron deficiency, as a result of frequent donation, most often causes rejection.
Kinetics of Iron Loss
More than one-half of the total iron in the body is in the form of Hb. Adult males have approximately 1000 mg of storage iron, whereas adult females typically have only 250–500 mg. A twice-per-year blood donor loses more blood than does the average menstruating woman, whose annual loss does not normally exceed 650 ml. In men, iron lost from a 450-ml donation (242 ± 17 mg) is made up in about 3 months by enhanced absorption of dietary iron. For women (217 ± 11 mg), almost 1.5 years would be required to replace iron lost at donation. Based on these data, the interval between donations would appear to be no less than 3 months for men and 6 months or more for women (Finch 1972). However, even when these intervals are observed, blood donation seems to cause iron deficiency. Generally, iron stores are adequate between the first and second donations. Thereafter, an increase in iron absorption is necessary to sustain the increased plasma iron turnover and maintain iron balance (Garry et al. 1995). In total, 8% of males who donate four or five times per year and 19% of those who donate every 8 weeks will become iron deficient. If these male donors continue to donate, some may still meet the Hb and/or Hct standard for donation, but develop red cell indices consistent with iron deficiency. Some men will qualify to donate even although their Hb is substantially below their baseline value; others will be deferred as their Hb level drops below the 12.5-g requirement (Simon et al. 1981). In a group of healthy young men who gave blood every 2 months and received no iron therapy, one-third had no stainable iron in the marrow after four donations (Lieden 1975). In another study of donors deferred because of low Hb concentration, more than 70% had evidence of iron deficiency (Finch et al. 1977). Similarly, even male donors who gave blood only twice per year had a significant fall in mean ferritin levels accompanied by a lower Hb, red cell count and mean corpuscular Hb concentration (MCHC) if they had donated more than 10 times (Green et al. 1988). Iron stores are exhausted in virtually all female donors regardless of the frequency of blood donations (Conrad et al. 1981).
Oral Iron Supplementation
The suggestion that repeat blood donors receive iron supplementation raises a number of scientific, medical and ethical questions of which the scientific ones are most easily answered. Oral iron supplementation, if prescribed in sufficient doses and if taken by the donor, can increase annual donation frequency without the risk of iron deficiency (Bianco et al. 2002). The suboptimal doses found in daily multivitamins will not. In a study of donors who had given blood either 15 times or 50 times at the rate of five donations per year and had received a supplement of 600 mg of Fe2+ after each donation, about 75% had no stainable iron in the marrow (Lieden 1973). These subjects were not anaemic and had normal serum iron levels. In a further study in which blood was donated every 2 months, resulting in an average daily loss of 3.5 mg of iron, iron stores were not maintained at the initial level, even when the subjects received 100 mg of iron per day (Lieden 1975). On the other hand, in 12 regular blood donors with subnormal serum ferritin levels who gave blood every 8 weeks, the ingestion of 5600 mg of iron between phlebotomies was sufficient to restore serum ferritin levels to normal and to provide a small store of iron in the bone marrow (Birgegard et al. 1980). Despite this finding, some experts believe that frequent bleeding even with iron supplementation is not justified and that the maximum annual rate of donation should be twice for men and once for women (Jacobs 1981).
When the interval between donations is 3 months or less, iron supplementation in the form of ferrous iron may be given to try to prevent iron deficiency. In the past, ferrous sulphate and ferrous gluconate have been prescribed but some preparations are not well-absorbed, cause gastrointestinal disturbances in many donors, and are potentially fatal if ingested in large doses by children. For all of these reasons, carbonyl iron, a small particle preparation of highly purified metallic iron with high bioavailability and almost no risk of accidental poisoning in children, seems better suited for this purpose. A series of studies by Gordeuk and co-workers (1990) showed that, with a regimen of 100 mg of carbonyl iron taken daily at bedtime for 56 days, the minimum interval between donations in the US is well-tolerated and provides enough absorbable iron to replace whatever is lost at donation in 85% of donors. A higher dose of carbonyl iron given for a shorter period of time (600 mg of iron three times daily for 1 week) caused gastrointestinal side-effects similar to those seen with ferrous sulphate (Gordeuk et al. 1987). In a controlled trial designed to prevent iron deficiency in qualifying female blood donors, women who received carbonyl iron (100 mg at bedtime for 56 days) increased their mean number of donations per year from 2.4 to 3.6 while increasing their iron stores (Bianco et al. 2002).
Iron supplementation programmes are difficult to implement and maintain (Skikne 1984). Even ongoing programmes may have limited effectiveness if the iron preparation is unpalatable or poorly absorbed (Monsen et al. 1983). Many blood collectors remain reluctant to become ‘community clinics’, whereas others raise concerns about prescribing medication for normal volunteers in order to extract additional donations. Finally, some physicians are concerned about overlooking occult gastrointestinal malignancy as the stool turns dark with the iron preparation and occult blood may be lost without the resulting anaemia. This has been estimated to be a very low risk (Bianco et al. 2002).
Laboratory Monitoring of Iron Status
Laboratory monitoring can help manage the repeat blood donor. In normal, well-nourished subjects, serum ferritin concentration is a good indicator of iron stores (Worwood 1980), although red cell ferritin may be a better indicator of body iron status (Cazzola and Ascari 1986). Red cell ferritin is affected only slightly by factors other than tissue iron stores (e.g. inflammation, increased red cell turnover), whereas these factors may cause a rise in serum ferritin. Several studies of ferritin estimations in large series have confirmed that iron stores may be seriously depleted in blood donors (Finch et al. 1977; Bodemann et al. 1984; Skikne 1984). For serial blood donors who have complete blood counts performed, a progressive drop in the red cell indices [mean cell volume (MCV), MCHC] provides an even easier and less expensive method of following functional iron status (Leitman et al. 2003). An isolated low MCV determination may result from a haemoglobinopathy rather than iron deficiency more than 30% of the time depending upon the ethnicity of the donor population (Bryant et al. 2009).
Screening Test to Detect Anaemia
Subjects should be tested before donation to make sure that they are not anaemic. A common test is to allow a drop of blood to fall from a height of 1 cm into a selected solution of copper sulphate and thus to determine its Hb concentration from the specific gravity. A more accurate, portable photometric method avoids some of the environmental hazards of the copper sulphate technique at a higher cost (James et al. 2003). In some countries, such as France, the Hb level is no longer determined before donation. Instead, the Hb level and the packed cell volume (PCV) of blood donations are estimated. Donors found to be anaemic are recalled for investigation.
The lowest acceptable Hb levels for male and female blood donors, defined by the specific gravity of whole blood, correspond reasonably well with limits defined by conventional spectrophotometric analysis of venous samples. In a series of 200 healthy subjects, the range (mean ± 2 SD) was 121–165 g/l for males and 120–147 g/l for females (Bain and England 1975). Similar values were reported in a review of normal Hb concentrations based on published data (Garby 1970). Haematologic differences have been found between African–Americans and white people; reference standards for Hb, PCV and MCV differ among ethnic groups (Beutler and West 2005).
A common practice is to accept male donors whose blood contains at least 135 g Hb/l as judged by a copper sulphate solution of specific gravity 1.055, and female donors whose Hb concentration is not less than 125 g/l as measured by a copper sulphate solution of specific gravity 1.053. If a donor fails the copper sulphate test, rapid microhaematocrit or Hb determinations can be done at the donor station from skin-prick blood, using accurate portable photometry instruments (Cable 1995). In London, these supplementary determinations revealed that in approximately 50% of cases a donation can be taken, thus saving the donor from unnecessary anxiety (James et al. 2003). When donors are found to be anaemic (2–3% of London donors, mostly women), venous samples are taken and retested by conventional haemoglobinometry. Donors who are confirmed as anaemic should be referred to their general practitioner. In the US, the minimum acceptable level of Hb for donors is 125 g Hb/l (American Association of Blood Banks 2003).
The copper sulphate technique, although easy and convenient is being phased out, in part because of the environmental hazard and risk to screening personnel, and in part because of its poor accuracy and reproducibility. Errors in technique in using the copper sulphate method include incorporation of air bubbles or the use of an inadequate height for dropping the blood, which tend to underestimate the Hb concentration so that donors may be rejected unnecessarily. On the other hand, in rare cases in which the plasma protein concentration is greatly raised, anaemic donors may be accepted as normal, each extra g/dl of plasma protein being equivalent to 0.7 g/dl Hb (Mannarino and MacPherson 1963). Falsely high positive results in the copper sulphate method may also be due to a high white cell count associated with granulocyte mobilization or leukaemia.
The source of the blood sample may determine acceptance or rejection of a donor in borderline cases. Based on microhaematocrit methods, blood obtained by ear lobe puncture was found to give values about 6% higher than those obtained simultaneously by fingerprick puncture (Avoy et al. 1977), and blood from fingerprick was found to have an Hb value 2% lower than that of venous blood obtained simultaneously (Moe 1970). Ear lobe sampling is unreliable and is now considered obsolete in the US.
Noninvasive technology using reflectance spectroscopy for estimating hemoglobin concentration has been introduced as a possible screening technique. If successful, the method may eliminate the fingerstick and change the process of donor screening.
Hb Regeneration After Normal Blood Donation
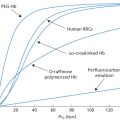
In 14 normal healthy subjects bled of about 400 ml of blood (8% of their blood volume), circulating reticulocytes increased minimally but significantly, and peaked on the ninth day after bleeding. The Hb level was lowest 1 or 2 weeks after bleeding, and increased rapidly thereafter, reaching predonation levels at 3–4 weeks (Figure 1.1). In a study in which total red cell volumes were measured in subjects who had donated about 190 ml of red cells, about 50 ml of red cells were restored after 1 week and restoration was almost complete at 6 weeks (Heaton and Holme 1994).
Untoward Effects During or Shortly After Venesection
When light-headedness and bruising at the venepuncture site are included, some 11–36% of blood donors will suffer a phlebotomy-related reaction (Newman 1997; Trouern-Trend et al. 1999; Newman 2003). The majority of these reactions are mild. However, a small number, some of which are avoidable, result in donor injury and disability. Reaction rates are higher in autologous donors, some of whom have significant degrees of medical debility (see Chapter 17).
Blood Pressure and Pulse Measurement: Predictive and Protective?
Blood pressure and pulse in the normal range have been traditional screening standards for assuring that prospective blood donors are healthy and for predicting donors at increased risk for cardiovascular and neurovascular adverse events. ‘Normal’ for this purpose has relied more on consensus definition than on scientific rationale. The older literature is equivocal. Poles and Boycott (1942) reported no relationship between low initial blood pressure and syncopal episodes, whereas other studies reported weak correlation (Boynton and Taylor 1945; Callahan 1963). Recent studies have not confirmed a relationship between blood pressure and fainting at the extremes of the range used for accepting donors (Wiltbank et al. 2008; Trouern-Trend et al. 1999; Eder et al. 2009). However before discarding blood pressure measurement as one indicator of donor health, consider that the recent studies were conducted in the era when AABB standards for blood pressure were in place and few data concerning donors with systolic pressure >180 or diastolic pressure <80 are available. Prospective donors who fell outside of this range were deferred.
Fainting or the Vasovagal Attack
Syncope, the sudden brief loss of consciousness caused by diminished cerebral blood flow, occurs at least once in almost 22% of the population, and 9% have recurrent syncope (Lu et al. 2003). Syncope occurs in both children and adults and is responsible for about 6% of emergency room visits and 3% of hospitalizations. Most syncopal events are triggered by standing or emotion and are often referred to as vasovagal reactions. The mere sight of blood being taken from another person can precipitate a ‘vasovagal attack’ in certain subjects. Withdrawing a sufficient quantity of blood will provoke syncope in everyone. After the loss of as little as 400 ml of blood, some subjects remain predisposed to faint even several hours later if they rise suddenly from a sitting or lying position, or if they remain standing for prolonged periods. In view of this risk, all donors should be observed for at least 15 min after donation and should be questioned about their occupation. Donors in whom fainting would be especially hazardous to themselves or to others (e.g. pilots, surgeons and bus drivers) should probably refrain from work or potentially dangerous hobbies for up to 12 h after giving blood. Donors who experience a delayed faint should be indefinitely deferred from blood donation, regardless of their occupation (Kamel et al. 2010).
Pathophysiology
The vasovagal attack appears to be a hypothalamic response mediated by either a central neural pathway or a peripheral pathway associated with the baroreceptors. While blood is being drawn, warning of oncoming fainting may be presaged by a decline in bloodflow rate, as already noted in the seventeenth century (Harvey 1628). Vasovagal reactions are typically biphasic, originating with a stress-induced elevation in pulse and blood pressure, and rapidly followed by the commonly recognized signs and symptoms of fainting. As the syndrome develops, the donor feels weak and dizzy. Clinical characteristics include sweating and pallor, cool extremities, strikingly slow and faint pulse, low or undetectable blood pressure, vomiting and, less commonly, tetany and urinary and faecal incontinence. Loss of consciousness may follow and convulsions are seen occasionally. These effects result primarily from the action of the autonomic system, causing slowing of the heart, vomiting and sweating and, perhaps most important, dilatation of the arterioles, leading to a sudden fall in blood pressure (Barcroft et al. 1944). The slow pulse rate (30–60 per min) in the vasovagal attack is the most useful single sign in differential diagnosis.
Donor Characteristics and Frequency
Estimates of the frequency with which fainting occurs in blood donors vary according to the definition of the term ‘faint’. In the Medical Research Council’s inquiry (1944), ‘fainting’ was defined as the manifestation of any of a series of signs or symptoms such as pallor, sweating, dimness or nausea. By this definition, some 5–6% of donors fainted. A similar frequency of vasovagal symptoms (5.3%) was noted by interviewers who solicited this information from 1000 donors 3 weeks after blood donation (Newman 2003). In a series of 10 000 cases, only 2.8% of donors fainted, but the term ‘fainting’ was applied only to those who lost consciousness or could not stand or sit without doing so (Poles and Boycott 1942). Moderate to severe reactions are reported in 0.08–0.34% of donations (Newman 1997). In a retrospective analysis of 793 293 allogeneic whole blood and apheresis donations in a single year, the prevalence of reactions classified as moderate or severe was 41 in 10 000 donations; 24% of these reactions were delayed (>15 min) and 12% occurred off-site (Kamel et al. 2010). Delayed reactions were associated with female sex and with low estimated blood volume. First-time donors were about twice as likely to have reactions as were repeat donors (see also below). Off-site reactions, particularly in female donors, were more likely to be associated with a fall, with head trauma, with other injury, and with the use of outside medical care.
Vasovagal reactions occur more commonly on the first occasion of giving blood. Of course those with severe reactions are frequently deferred from further donations, and thus the ‘repeat donor’ is in a selected group. Among 1000 donors studied over a period of several years, more than one-half experienced their only symptoms at the time of their first donation; the incidence of reactions fell progressively over a period of 6 years (Beal 1972). In 40 437 donations studied, fainting was found to be more common in female donors; 4.9% of first-time female donors suffered vasovagal reactions compared with 3.8% of first-time male donors. The figures were less than half in repeat donors of both sexes, 1.9% and 1.1% respectively (Tomasulo et al. 1980). However, gender may be a surrogate measure for body weight. In a case–control study, age, weight and first-time donor status were significant predictors of syncope (Trouern-Trend et al. 1999).
One early study noted a relation between the incidence of fainting and the amount of blood donated. The incidence was 3.8% in those giving 440 ml, but 8.5% in those giving 540 ml (Poles and Boycott 1942). In normal males from whom 800–1000 ml of blood was taken, the incidence was 11 out of 28, and in those from another series, loss of consciousness was observed in 5 out of 6 (Ebert et al. 1941). In experiments in which up to 1500 ml of blood was withdrawn from normal volunteers, fainting could be produced in all subjects if enough blood was withdrawn within a limited time (Howarth and Sharpey-Schafer 1947).
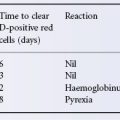
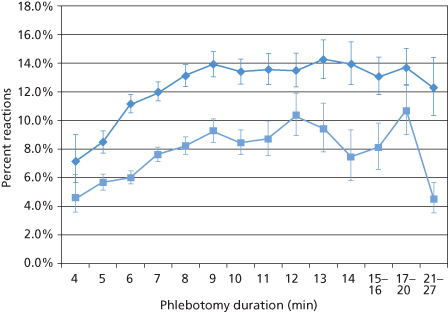
Rapid phlebotomy would seem to be a factor in syncopal reactions, but the opposite appears to be true. Newman et al. (2008) compared the rate of vasovagal donor reactions with the duration of whole-blood collections in first-time high school donors. A total of 126 195 first-time, 17-year-old Caucasian donors in 35 American Red Cross blood centres, donated a volume 525 ml, whole blood with phlebotomy intervals ranging from 4 to 27 minutes (velocity, 131–19 ml/min). Vasovagal reactions were higher in females than in males at all duration times (Figure 1.2). The reaction rates increased with longer phlebotomy durations in both females and males, a seeming paradox. It is not clear whether these observations can be extended to other donor populations, age groups, or repeat donors; however deferring young donors with low estimated blood volume represents one approach to protecting donors at increased risk of reactions without jeopardizing the adequacy of the blood supply (Rios et al. 2010).
Figure 1.2 Vasovagal reactions in first-time, 17-year-old, Caucasian female blood donors ( ) and in first-time, 17-year-old Caucasian male blood donors (
) and in first-time, 17-year-old Caucasian male blood donors ( ) at different phlebotomy durations
) at different phlebotomy durations
(Source: Newman et al. 2008. Reproduced with permission of John Wiley & Sons Ltd.).
Management of Vasovagal Reactions: Science, Custom and Myth
Subjects who display these signs but who have not lost blood recover rapidly when they are placed supine and positioned so that the head is lower than the rest of the body (Trendelenburg position). Time-honoured measures include applying an ice pack or cold towel to the (donor’s) forehead or back of the neck or using a paper bag rebreathing technique to elevate CO2 and cerebral blood flow. The effectiveness of such techniques is unknown. Inhalation of ammonia salts adds very little other than irritating the respiratory membranes and the blood donor. Intravenous infusion, inotropic agents and cholinergic blockade are rarely necessary. Donor room personnel should be cautioned against the precipitous use of external defibrillation and cardiopulmonary resuscitation, as these techniques will invariably cause more harm than good to a donor suffering from a vasovagal attack.
Some Consequences of Syncope
Syncope can have serious consequences. Seizure activity and tetany have been reported in about 25% of syncopal reactions. Skull and facial bone fractures, scalp lacerations, chipped teeth and extremity fractures have all been reported (Boynton and Taylor 1945; Kamel et al. 2010). A retrospective analysis of 178 vasovagal reactions from 194 000 donations found that 10% of these donors sustained a head injury and 6% required additional medical care in an emergency room. One injured donor developed post-concussion syndrome and suffered headaches and other symptoms for more than 1 year (Newman and Graves 2001). Although 12% of the reactions occurred off site, the majority within 1 h of donation. More than 60% occurred at the refreshment table, an observation that should stimulate serious thought about the design and oversight of the donor recovery area.
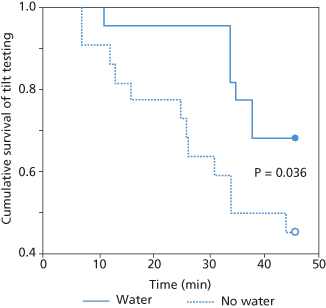
Pre-donation water ingestion has been used as a simple prophylaxic measure against vasovagal reactions in blood donors. Water ingestion has a pressor effect, enhances tolerance of upright posture by increasing peripheral vascular resistance, and reduces the chance of syncope during orthostatic stress (Lu et al. 2003). Using a tilt-table orthostatic stress system, Lu et al. (2003) found that drinking 473 ml water enhanced tolerance of upright posture in 22 subjects with no prior history of syncope (Figure 1.3). A 16 oz (473-ml) water drink decreased the vasovagal donor reaction rate in high-school donors by 21%, but to varying degrees in different subpopulations (Newman et al. 2007).
Figure 1.3 Cumulative proportion of subjects remaining free of presyncopal episodes with and without water. At 30 minutes, 95% of those with water compared with 63% of those without water were able to tolerate tilt. At completion of study (45 minutes), 69% with water compared with 45% without water were able to tolerate tilt
(Source: Lu et al. 2003. Reproduced with permission of Lippincott Williams & Wilkins.).
Some Other Untoward Effects
Bruising
Bruising is one of the commonest complications of blood donation, and is reported in 9–16% of donations (Boynton and Taylor 1945; Newman 1997). In the majority of cases, the haematoma is restricted to a small area in the antecubital fossa. However, very large, incapacitating and painful haematomas develop occasionally following blood donation. Inattention to an enlarging haematoma can result in a forearm compartment syndrome with consequent neural and vascular compromise and massive tissue necrosis. Instruction regarding pressure dressing, cold compresses and medical follow-up can prevent a large bruise from turning into a medical emergency.
Phlebitis and Cellulitis
Mild phlebitis at the venepuncture site in the antecubital fossa is common, self-limited and usually of little consequence. Mild discomfort, warmth and local linear or surrounding erythema may be difficult to distinguish from mild cellulitis or reaction to the topical antiseptic, particularly if the latter contains iodine. Despite a seemingly benign appearance, local reactions merit close medical follow-up to prevent extension of these lesions to abscess formation or septic phlebitis. Early application of warm compresses, oral anti-inflammatory agents and administration of antibiotics when indicated are prudent. Newman reports an incidence of local reactions of 1 in 50 000 to 1 in 100 000 (Newman 1997).
Nerve Injury
The proximity of cutaneous branches of the medial and ulnar nerves to the large-bore needle access to the antecubital vein makes occasional injury to these structures inevitable. The injuries are generally transient and rarely a source of donor distress. In most instances the donor reports a localized area of numbness or tingling (paraesthesia). In 419 000 donations over a 2-year period, Newman and Waxman (1996) reported an incidence of peripheral nerve injury of 1 in 6300, with 78% of donors reporting their injury on the day of donation. Symptoms were almost evenly divided between paraesthesias and radiating pain, although eight donors reported loss of arm strength. Almost one-quarter of these reports were associated with haematoma formation at the venepuncture site. In total, 70% of donors recovered completely within 1 month; 52 out of 56 recovered completely and four donors reported a small area of persistent numbness.
Puncture of an Artery
This leads to an unusually rapid flow of bright red blood; when the needle is withdrawn, there may be severe leakage of blood, followed by extensive bruising. If an arterial puncture is suspected, the needle should be withdrawn immediately and firm pressure applied for at least 10 min, followed by a pressure dressing. If the radial pulse is not palpable, the donor should be referred to a vascular specialist. Rare complications of arterial injury include pseudoaneurysm formation and development of an arteriovenous fistula (Lung and Wilson 1971; Popovsky et al. 1994).
Tetany
Tetany is occasionally observed in blood donors (incidence 1 in 1000), characteristically in nervous subjects, and is thought to be due to hyperventilation. Manifestations may include carpopedal spasm, laryngismus, stridulus and a positive Chvostek’s sign. Rapid relief can be obtained by rebreathing from a paper bag or inhaling 5% CO2 from a cylinder, an unlikely method of management in the modern blood centre (Frazer and Fowweather 1942). In an apheresis donor, tetany is almost invariably preceded by tingling and paraesthesias, is the consequence of citrate-induced hypocalcemia, and should be managed by reducing the flow of citrated blood and administration of oral calcium.
Convulsions
These are uncommon. If seizures occur, the donor should be immobilized on the bed or on the floor to prevent injury, and an open airway ensured.
Air Embolism During Blood Donation
When blood is taken into plastic bags that contain no air, there is no possibility of air embolism. On the other hand when blood is drawn into glass bottles (as is still the practice in some countries), air embolism may occur. The prime cause of air embolism in this circumstance is obstruction to the air vent of the bottle (for details and further references, see seventh edition, p. 6). Apheresis devices include inline filters and air detector alarm systems to prevent air from a defective seal from being pumped into a donor.
Fatalities Attributed to Blood Donation
In 1975, the Food and Drug Administration of the USA published regulations requiring the reporting of deaths associated with blood collection, plasmapheresis and transfusion. In the 10 years from 1976 to 1985, three deaths attributed to blood donation were reported out of 100 million units of donated blood. Two deaths were due to myocardial infarction and one was in a patient with phaeochromocytoma (Sazama 1990). In 1999, of 48 deaths reported to the FDA in some 20 million donations, four fatalities occurred in donors. Two of these were donors of autologous units and all deaths were attributed to underlying disease. In 2009, three fatalities following whole blood donation were reported. In two of these cases, donation was ruled out as the cause of death, and in the third case, although the donation could not be definitively eliminated as related to the donor’s death, no evidence supported a causal relationship between the donation and subsequent death of the donor.
Potential Health Benefits of Blood Donation
For the volunteer donor, the chief benefit lies in the satisfaction of selfless concern for the welfare of others. An obvious potential benefit is the unexpected clue to the diagnosis of a disorder that may be treatable, such as iron deficiency, chronic hepatitis, or in the case of pathogeneic bacteria detected by platelet culture, an underlying infection or occult tumour (Haimowitz et al. 2009). However, two studies suggest that there may be more tangible health benefits, particularly for middle-aged men, such as lowering the risk of cardiovascular disease (Meyers et al. 1997; Salonen et al. 1998). The proffered explanation derives from the so-called ‘iron hypothesis’: menstrual iron loss protects women against cardiovascular disease; iron stores correlate with cardiovascular disease across European populations and heart failure is a hallmark of disorders of iron surplus (Sullivan 1981). One proposed mechanism for this association is generation of oxygen-free radicals that induce oxidation of lipids (McCord 1991). However the Johns Hopkins Hospital autopsy registry found less coronary artery disease in hearts from patients with haemochromatosis and haemosiderosis than in hearts of age- and sex-matched controls (Miller and Hutchins 1994).
Salonen and co-workers (1998) conducted a prospective 9-year follow-up study of 2862 men aged 42–60 from eastern Finland, who had participated in the Kuopio Ischemic Heart Disease Risk Factor Study (Salonen et al. 1998). Only one man out of 153 who had donated blood in the 24 months prior to baseline examination suffered a myocardial infarction, compared with 316 (12.5%) of the 2529 non-donors. Meyers and co-workers (1997) compared the rate of cardiovascular events of 665 blood donors with that of 3200 non-donors in a telephone survey of a cohort selected from the Nebraska Diet Heart Survey. By multivariate analysis, non-smoking men who had donated at least once in the previous 3 years had a significantly lowered risk of cardiovascular events; no additional benefit was derived from longer or more frequent donation. Numerous cofactors confound these studies, and the validity of this statistical association has been questioned (Ford 1997).
Although the hypothesis remains intriguing, it is premature to suggest that health benefits, other than those attributable to altruism, will derive from blood donors – even for non-smoking middle-aged men.
Directed Donations
Directed donations are those given exclusively for named patients, usually by relatives or friends. The use of directed donations contravenes the normal principles of voluntary blood donation, fails to increase safety (Cordell et al. 1986; Strauss 1989) and finds medical justification in vanishingly few circumstances: (1) in patients with rare blood groups when the only available compatible donors may be close relatives; (2) in occasional patients awaiting renal transplants, for whom donor-specific transfusions may still play a role (Salvatierra et al. 1981; Anderson et al. 1985; see also Chapter 14); (3) in infants with neonatal alloimmune thrombocytopenia or haemolytic disease of the newborn, for whom maternal platelets or red cells are occasionally invaluable; (4) in children requiring open-heart or extensive orthopaedic surgery, for whom the total requirements for blood and components can be collected preoperatively, as for autologous transfusion but from designated relatives or parents, thus minimizing the number of donor units to which the children are exposed (Brecher et al. 1988); and (5) in patients with leukaemia in relapse after bone marrow transplantation, for whom donor leucocytes are used as adoptive immunotherapy to induce graft-versus-leukaemia (GvL) effect (Sullivan et al. 1989; Kolb et al. 1990).
The practice of transfusing parental blood to premature newborn infants is not without risks. Mothers may have antibodies against antigens (inherited from the father) on the infant’s red cells; platelets or white cells and maternal plasma should not be used. Fathers should not serve as cell donors because they may have antigens present on their red cells, which are incompatible with maternally derived antibodies present in the fetus. Moreover, in view of partial histocompatibility, transfusion of cells from parents and close relatives may result in graft-versus-host disease (GvHD) in the infants, or older children, especially if the infants are immunodeficient (Bastian et al. 1984; Strauss 1989). Circumstances such as these, in which blood or platelet suspensions should be irradiated, are described in Chapter 15.
The practice of transfusing parents with blood from their offspring can also be dangerous. Fatal GvHD occurred in two immunocompetent adult patients who were transfused with fresh whole non-irradiated blood from their children during cardiac surgery. In both cases, one of the donors was homozygous for one of the recipient’s HLA haplotypes (Thaler et al. 1989). When such transfusions are indicated, and except for instances in which adoptive immunotherapy is intended, the components should be treated with 25 Gy gamma irradiation (see Chapter 15).
People who donate for friends and family lose their anonymity and may be subject to influences not placed upon community donors. Such donors may provide less than candid answers to sensitive donor questions, either because they believe that unsafe blood will inevitably be detected by testing procedures or because they wish to conceal information from the recipient or the blood collector. Two examples follow:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree