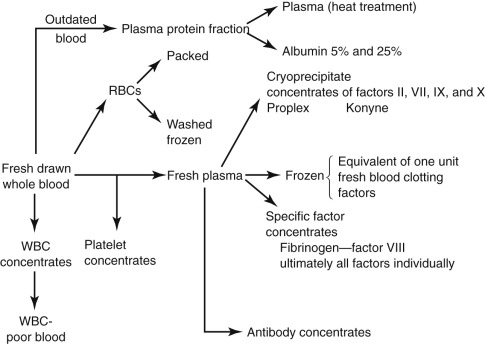
Despite the recent increase in the use of hematopoietic growth factors, transfusion therapy plays an important role in caring for oncology patients, particularly now that more effective treatment regimens have led to longer survival. In many instances, a patient with cancer behaves like a patient with a chronic disease requiring frequent blood components caused by disorders secondary to the disease, treatment, or both. Whole blood is separated into cellular and noncellular components, including red blood cells (RBCs), platelets, and plasma.
- 1.
Blood component: A portion of blood is separated by physical and mechanical means, such as differential centrifugation ( Fig. C.1 ). Cell separation technology, capable of collecting platelets, plasma, granulocytes, peripheral blood stem cells, and RBCs, has an increasingly important role in transfusion medicine. Anticoagulants and other additives used in blood collection containers allow storage of liquid red cells for up to 42 days.
- a.
Packed red blood cells (PRBCs): These cells are prepared from whole blood by centrifugation and subsequent removal of plasma.
- (1)
Hematocrit: 60% to 80%
- (2)
Indications
- (a)
Replacement of hemoglobin-containing cells in an anemic patient with heart failure, renal failure, burns, or bone marrow failure
- (b)
Debilitated patients
- (c)
Elderly patients
- (d)
Patients with liver disease
- (a)
- (3)
Recommend to use PRBCs for losses of blood less than 1000 to 1500 mL/70 kg; with greater losses, other blood components should be used
- (4)
Therapeutic effect: In a 70-kg adult, each unit should increase the hematocrit by 3% to 4%.
- (1)
- b.
Frozen RBCs: Long-term preservation of frozen RBCs without damage can be accomplished by the addition of glycerol; before transfusion, the RBCs should be thawed and washed to remove glycerol
- (1)
Advantages
- (a)
Blood of rare types can be stored for long periods.
- (b)
2,3-Diphosphoglycerol and adenosine triphosphate levels remain the same as they were on the day that the blood was frozen.
- (c)
Free of plasma protein, platelets, white blood cells, and fibrin
- (d)
Has been claimed to reduce the incidence of hepatitis acquired from a blood transfusion
- (a)
- (2)
Disadvantages
- (a)
Expensive
- (b)
Outdated in 24 hours after thaw
- (c)
Takes time to thaw and deglycerolize
- (a)
- (1)
- c.
Buffy coat: poor erythrocytes; would reduce the incidence of febrile transfusion reaction
- (1)
Indications
- (a)
Patients with repeated febrile nonhemolytic transfusion reaction caused by leukocyte antibody
- (b)
Hematopoietic growth factors applied to oncologies from transfusion therapy is designed to limit the exposure of patients to allogenic blood with its innate risks. The synthesis of erythropoietin (EPO) by recombinant technology was a very important advance in decreasing RBC transfusions. EPO has also been used to increase the yield of autologous donations and to stimulate erythropoiesis after surgery.
- (a)
- (1)
- d.
Platelet concentrates
- (1)
One unit of platelet concentrate contains 5.5 × 10 10 platelets suspended in 30 to 50 mL of plasma
- (2)
Shelf-life: 72 hours at room temperature
- (3)
Thrombocytopenia does not usually produce serious bleeding unless the platelet count is below 20,000, except if there is a platelet function defect, a coagulation defect, or local cause of hemorrhage (e.g., trauma, surgery)
- (1)
- e.
Fresh-frozen plasma (FFP)
- (1)
Contains albumin, globulin, active coagulation factors, complement, and electrolytes
- (2)
Should be type specific
- (3)
Shelf life: 12 months at −20° to −30°C; should be used within 2 hours after thawing
- (4)
Indications
- (a)
Deficiency in coagulation factors
- (b)
Situation with plasma loss
- (c)
Rapid reversal of oral anticoagulant therapy
- (a)
- (1)
- f.
Cryoprecipitate: Cold insoluble precipitate remains when FFP is allowed to thaw at 4°C; it contains factor VIII with fibrinogen and factor XIII
- (1)
Indications
- (a)
von Willebrand disease
- (b)
Replacement of fibrinogen, factor XIII
- (a)
- (1)
- a.