The development of colorectal cancer is characterized by a multitude of molecular events that can occur through the pathways of loss of heterozygosity, microsatellite instability, and CpG-island methylation. The accumulation of these molecular events ultimately results in polyps formed from previously normal mucosa to develop the fundamental characteristics of cancerization: uncontrolled proliferation, growth, and invasion. Advances in the understanding of molecular events leading to colorectal cancer have led to the development of biomarkers, patient-specific and tumor-specific molecular signatures that have potential as tools for accurate risk assessment, personalized treatment planning, development of targeted agents, and evaluation of treatment response.
Key points
- •
Genetic mutations in colorectal cancer (CRC) result in oncogene activation with uncontrolled cellular proliferation (ras, myc, src, and erbB2), or tumor-suppressor gene deletion with uncontrolled cell growth (APC, DCC, and p53).
- •
Loss of heterozygosity is characterized by chromosomal deletions and tumor aneuploidy. A key example of this occurs in the chromosome 18q region, deleted in up to 70% of CRCs.
- •
CRCs can also arise from mutations in the microsatellite instability pathway, characterized by errors in mismatch repair during DNA replication; these are seen in both hereditary and sporadic tumors.
- •
In the CpG-island methylation pathway, genes do not accumulate mutations; instead they are activated or inactivated by methylation (epigenetic alteration).
- •
MicroRNAs are posttranscriptional regulators. Abnormal microRNA expression profiles accompany every aspect of CRC transformation.
Introduction
Significant advances in molecular biology have resulted in a better understanding of the genetic defects and molecular abnormalities associated with the development and progression of colorectal cancer (CRC). Efforts to translate this knowledge into clinical applications have led to exciting developments in biomarker development. The National Institutes of Health defines a biomarker as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention.” Patient-specific and tumor-specific molecular signatures may represent the ideal CRC biomarkers, by allowing :
- •
Risk stratification
- •
Accurate prognostic assessment
- •
Personalized treatment planning
- •
Development of targeted agents
- •
Accurate evaluation of treatment response
As multimodal treatment of colorectal cancer progressively shifts toward targeted therapy based on these molecular biomarkers, it is important for the cancer surgeon to have a thorough understanding of recent advances in colorectal molecular oncology. The purpose of the article is 3-fold:
- 1.
To provide a survey of the key molecular abnormalities relevant to CRCs
- 2.
To review details of the clinical relevance of these abnormalities
- 3.
To demonstrate through a specific example of a molecular abnormality the process of translational research
Introduction
Significant advances in molecular biology have resulted in a better understanding of the genetic defects and molecular abnormalities associated with the development and progression of colorectal cancer (CRC). Efforts to translate this knowledge into clinical applications have led to exciting developments in biomarker development. The National Institutes of Health defines a biomarker as “a characteristic that is objectively measured and evaluated as an indicator of normal biological processes, pathogenic processes, or pharmacologic responses to a therapeutic intervention.” Patient-specific and tumor-specific molecular signatures may represent the ideal CRC biomarkers, by allowing :
- •
Risk stratification
- •
Accurate prognostic assessment
- •
Personalized treatment planning
- •
Development of targeted agents
- •
Accurate evaluation of treatment response
As multimodal treatment of colorectal cancer progressively shifts toward targeted therapy based on these molecular biomarkers, it is important for the cancer surgeon to have a thorough understanding of recent advances in colorectal molecular oncology. The purpose of the article is 3-fold:
- 1.
To provide a survey of the key molecular abnormalities relevant to CRCs
- 2.
To review details of the clinical relevance of these abnormalities
- 3.
To demonstrate through a specific example of a molecular abnormality the process of translational research
Adenoma-carcinoma sequence
Colorectal carcinoma is thought to develop from adenomatous polyps following the accumulation of mutations in what has come to be known as the adenoma-carcinoma sequence ( Fig. 1 ). Adenomatous polyps arise when mechanisms normally regulating epithelial renewal are disrupted. Cellular proliferation usually occurs exclusively at the crypt base, and cells undergo terminal differentiation with eventual apoptosis as they move toward the surface of the lumen. As the polyp increases in size it becomes more dysplastic, and cells ultimately acquire invasive potential. In addition to animal models and numerous epidemiologic and clinical observational studies, the validity of this model is confirmed by large, well-designed clinical trials that demonstrate a reduction of CRC in patients having undergone endoscopic polypectomy.
Vogelstein and colleagues characterized the molecular basis for this multistep process whereby each additional genetic event confers a survival advantage to the epithelial cell. According to this model, the accumulation of genetic mutations rather than their specific sequence ultimately determines tumor behavior (see Fig. 1 ). Inherited colon cancer syndromes such as hereditary nonpolyposis colon cancer (HNPCC) and familial adenomatous polyposis (FAP) result from germline mutations, whereas sporadic cancers arise from the accumulation of multiple somatic mutations.
Types of mutations
Genetic mutations can result in either activation of oncogenes or inactivation of tumor-suppressor genes.
Oncogenes
Oncogenes are normal cellular genes involved in cell-cycle regulation and growth. After acquiring a mutation, these genes become constitutively activated and result in uncontrolled cellular proliferation. These mutations are referred to as “gain of function” mutations, because they activate what was initially a normal gene function. Oncogenes associated with sporadic CRC include ras, myc, src, and erbB2.
The ras oncogene
The ras oncogene exists in 3 variants, of which K-ras is the most commonly involved in CRC. Ras mutations are seen in 50% of adenomas larger than 1 cm and up to 50% of sporadic CRCs. A signaling molecule in the epidermal growth factor receptor (EGFR) pathway, K-ras regulates cellular signal transduction, by acting as a one-way switch for the transmission of extracellular growth signals to the nucleus. The K-ras gene product is a G protein involved in intracellular signal transduction. When active, K-ras binds guanosine triphosphate (GTP); hydrolysis of GTP to guanosine diphosphate (GDP) then inactivates the G protein. Mutation of K-ras results in an inability to hydrolyze GTP, thus leaving the G protein permanently active, which leads to uncontrolled cell division.
Tumor-Suppressor Genes
In their normal state, tumor-suppressor genes inhibit the cell cycle. Their deletion or loss of function results in uncontrolled cell growth. Unlike proto-oncogenes, tumor-suppressor gene function is lost only when both alleles of the gene are mutated. Common examples encountered in CRC include APC, DCC, and p53.
The APC gene
Defects in the APC gene (located on chromosome 5q) were first described in patients with FAP, and are now known to be present in 80% of sporadic CRCs as well. Loss of APC gene function appears to be a very early and critical event in the development of CRC. Mutations in both alleles are necessary to initiate polyp formation, leading to sporadic CRC. The majority of these mutations are premature stop codons, resulting in a truncated APC protein. In FAP, a single germline mutation is required. The site of mutation correlates with the clinical severity of the disease. For example, mutations in either the 3′ or 5′ end of the gene result in attenuated forms of FAP, whereas mutations in the center of the gene result in more virulent disease. Therefore, knowledge of the specific mutation in a family may help guide clinical decision making.
It is thought that the abnormal APC gene promotes tumor formation through the Wnt (Wingless-type) signal transduction pathway involved in supporting intestinal epithelial renewal ( Fig. 2 ). The mutation results in an abnormal accumulation of β-catenin in the cell’s nucleus, which binds and activates the transcriptional factor Tcf-4. Because the β-catenin/Tcf-4 construct is a switch controlling proliferation versus differentiation of intestinal crypt cells, overactivation of the switch prevents cells from either entering G1 arrest or undergoing terminal differentiation, and induces resistance to apoptosis.
APC inactivation alone does not result in a carcinoma. Instead, this mutation sets the stage for the accumulation of genetic damage that results in malignancy. Additional mutations may include activation or inactivation of a variety of genes.
The p53 gene
The tumor-suppressor gene p53 has been well characterized in several malignancies. It acts as a transcriptional activator of at least 20 inhibitory genes and seems to be crucial in initiating a variety of growth-limiting responses including cell-cycle arrest to facilitate DNA repair, apoptosis, and differentiation. Because of this critical function in preventing propagation of cells with damaged genetic material, p53 has been referred to as the “guardian of the genome.” Mutations in p53 are present in 75% of CRCs. Inactivation occurs by a mutation of one allele followed by loss of the remaining wild-type gene, and appears to be a late event in the majority of CRCs. In addition, according to an international study of 3583 CRCs, the frequency of p53 mutations increases with advancing disease stage.
The DCC gene
Point mutations in the DCC (“deleted in colon cancer”) gene have been identified on chromosome 18q21 in CRCs. DCC is thought to have a role in cell-cell or cell-matrix interactions. Loss of DCC expression may be of prognostic value in patients with node-negative CRC. Five-year survival rates for patients with stage II CRCs that lack DCC expression are worse than for those that express it, more closely approximating those of patients with stage III (node-positive) disease.
Molecular pathways to colorectal tumorigenesis
The mutations involved in CRC pathogenesis and progression are now recognized to accumulate via 1 of 3 major genetic pathways:
- •
The loss of heterozygosity (LOH)/chromosomal instability pathway
- •
The microsatellite instability (MSI)/defective mismatch repair (MMR) pathway
- •
The CpG-island methylation/serrated methylated pathway (CIMP)
These pathways are useful for understanding the mechanisms underlying carcinogenesis; however, they are not mutually exclusive.
Loss of Heterozygosity/Chromosomal Instability Pathway
First described in patients with FAP, the LOH pathway is characterized by chromosomal deletions and tumor aneuploidy. Most CRCs appear to arise from mutations through this pathway. A key example of LOH occurs in the region of chromosome 18q, which has been found to be deleted in up to 70% of CRCs. DCC and SMAD4 are located in this region. As described earlier, DCC is a tumor-suppressor gene thought to be involved in differentiation and cellular adhesion in CRC. SMAD4 functions in the signaling cascade of transforming growth factor β and β-catenin (also a downstream effector of the APC gene). Tumors arising from the LOH pathway tend to occur in the more distal colon, often have chromosomal aneuploidy, and are associated with a poorer prognosis.
Microsatellite Instability/Defective Mismatch Repair Pathway
Fifteen percent to 20% of CRCs arise from mutations in the MSI pathway, which is characterized by errors in mismatch repair during DNA replication. These errors were first described in HNPCC (Lynch syndrome), but are now known to be present in sporadic tumors as well. Several genes seem crucial in recognizing and repairing DNA replication errors. These MMR genes include MSH2, MLH1, PMS1, PMS2, and MSH6. A mutation in 1 of these genes predisposes a cell to additional mutations, which may occur in proto-oncogenes or tumor-suppressor genes. Most HNPCCs are associated with MLH1 or MSH2 gene abnormalities, whereas sporadic cancers are associated with mutations of the MLH1 gene. Accumulation of these errors leads to genomic instability and ultimately to carcinogenesis. Microsatellites are regions of the genome particularly susceptible to replication error, because short base-pair segments are repeated multiple times. A mutation in an MMR gene produces variable lengths of these repetitive sequences, a finding called MSI.
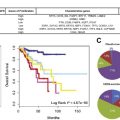
Tumors associated with a high degree of microsatellite instability (MSI-H) appear to have biological characteristics different to those of tumors that result from the LOH pathway. The majority of HNPCC as well as about 15% of sporadic CRCs have MSI-H tumors. MSI-H tumors are more likely to be right sided and are associated with a better prognosis than tumors that arise from the LOH pathway and are microsatellite stable, even if they more often are poorly differentiated.
CpG-Island Methylation Pathway
In the recently described CIMP pathway, genes do not accumulate mutations (deletions or insertions of bases); instead they are activated or inactivated by methylation. This process has been called epigenetic alteration to differentiate it from the more traditional genetic alterations or true mutations. In normal cells, methylation is a critical process for gene-expression regulation. In cancer, aberrant methylation (either hypermethylation or hypomethylation), usually of a promoter region, results in abnormal activation or inactivation of genes (including MMR enzymes). This abnormal gene silencing or activation results in a phenotype similar to that seen in the case of a true gene mutation. Consequently, CRCs with a high frequency of methylation of promoter islands are referred to as CIMP+ tumors. This pathway has also been called the serrated methylated pathway because of the observation that serrated polyps often harbor aberrant methylation, in contrast to adenomatous polyps that are more often associated with mutations in the APC gene (LOH pathway). In addition to abnormal methylation, this pathway is characterized by mutations in the BRAF kinase gene, which is an uncommon finding in traditional adenomas but a typical one in serrated adenomas.
Clinical implications
In addition to advancing our understanding of the pathogenesis of CRC, the characterization of these molecular pathways also has important clinical implications with regard to:
- •
Risk stratification
- •
Accurate prognostication
- •
Tumor-specific treatment planning
- •
Accurate evaluation of treatment response
- •
Targeted therapy
Risk Stratification and Prognostic Prediction
MSI-H CRCs have a distinct biological behavior: they are more often localized to the right colon, have a higher grade and mucinous component, have more necrosis, and bear a larger load of tumor-infiltrating lymphocytes. Thibodeau and colleagues and Lothe and colleagues initially observed that these tumors had a more favorable prognostic profile in 1993; however, these findings were based on small, retrospective series comprising patients with tumors of stage I to IV, without regard to adjuvant or palliative systemic therapy. Since then, well-designed, large studies of nonmetastatic CRC patients have shown that while MSI-H tumors were more often locally advanced (T4), they were less frequently associated with positive lymph nodes and metastatic spread. In a cohort of 2141 patients with stage II to stage III CRC, Sinicrope and colleagues showed that disease-free survival and overall survival were significantly better in MSI-H cases, with a hazard ratio of 0.73 (95% confidence interval [CI] 0.59–0.91) and 0.73 (95% CI 0.59–0.90), respectively. In addition, a large meta-analysis of 7642 patients with CRC from 32 studies confirmed the survival advantage of MSI-H tumors, regardless of stage (relative risk of death 0.65; 95% CI 0.59–0.71). As such, MSI-H status represents the best prognostic marker to date for CRC.
By contrast, other well-characterized molecular abnormalities in CRC have not been shown to have any prognostic value. For example, although K-ras mutations have consistently been shown to predict lack of response to anti-EGFR targeted therapy, they do not have any meaningful prognostic role in terms of clinical outcomes.
Tumor-Specific Treatment Planning
Emerging data about prognostic biomarkers suggest that that molecular abnormalities should have a predictive value in determining the efficacy of adjuvant systemic therapy in CRC. However, to date few of the known biomarkers have proved to be useful for predicting treatment response. MSI status has been most widely studied, and does appear to predict response to 5-fluorouracil (5-FU)-based chemotherapy. Kim and colleagues and Ribic and colleagues have demonstrated in retrospective studies that patients with MSI-H CRC experience no benefit with 5-FU–based regimens. The data from these studies showed that only patients with low-degree MSI CRC (microsatellite stable) had improved outcomes with the use of adjuvant 5-FU–based chemotherapy. Therefore, MSI testing is increasingly being performed on CRC tissue samples to help guide decision making about adjuvant therapy in stage II and stage III disease. A prospective randomized trial (ECOG 5202) is currently under way to determine the value of MSI and 18q LOH status in predicting response to therapy with FOLFOX6.
Although MSI-H is currently the only biomarker that predicts response to adjuvant therapy for stage III CRC, several other biomarkers are proving to be useful in predicting response to treatment in stage IV disease. Tyrosine kinase inhibitors (TKIs) are increasingly being used to treat metastatic CRC. Although some patients respond well to these agents, others do not. It is now known that K-ras status largely predicts response to anti-EGFR/TKI therapy (eg, cetuximab, panitumumab). Several trials have shown that the objective response in K-ras wild-type tumors can be as high as 44%, whereas the response in K-ras mutant tumors is essentially zero (CRYSTAL trial, OPUS trial). A recent meta-analysis of 12 trials confirmed the value of first-line, second-line, and even third-line therapy with anti-EGFR monoclonal antibodies combined with 5-FU exclusively in wild-type K-ras cases. As such, it is now considered standard of care to K-ras type all stage IV patients who are being considered for anti-EGFR therapy. Despite good response to anti-EGFR therapy in wild-type K-ras tumors, many of these patients fail to respond or develop resistance. Recent evidence shows that in addition to determining KRAS status, testing for BRAF, NRAS, and PI3KCA exon-20 mutations could improve response rates to cetuximab by identifying patients who would most likely benefit from the addition of this drug to systemic chemotherapy.
Other biomarkers also have been studied for the ability to predict response to therapy, but none have proved to be as robust as K-ras. For example, using archival material, Barratt and colleagues demonstrated that LOH at 1 or more chromosome 17p and 18q sites was predictive of FU-based treatment response. However, in the context of a prospective study assessing the relevance of irinotecan in 1264 patients with stage III colon cancer, Bertagnolli and colleagues showed only a statistically nonsignificant trend toward improved outcomes in MSI-H patients treated with irinotecan. Similarly, Kim and colleagues determined that MMR status and p53 positivity were not significantly predictive of outcomes in patients treated with 5-FU and oxaliplatin. These findings highlight the fact that molecular profiling for determination of systemic treatment requires a more refined understanding before mainstream clinical application is achieved. In particular, homogeneous groups of patients based on compatible risk profiles and equivalent cancer regimens need to be enrolled.
Molecular Profiling and Evaluation of Treatment Response
It is increasingly being recognized that no single biomarker will prove to be the “holy grail” for prognostic assessment, treatment planning, and response assessment. Rather, there is currently an intense research focus in identifying patterns of gene expression that are meaningful in terms of clinical outcomes. This type of molecular profiling has been most widely studied in breast cancer, but is rapidly growing to include a variety of other malignancies (including CRC), and the pharmaceutical industry has shown great interest developing products that predict prognosis and response to treatment. For example, OncotypeDx Colon (Genomic Health, Redwood City, CA) is a 12-gene profile that provides a composite prognostic recurrence score. Until recently, evidence was limited to validation studies presented mostly as meeting abstracts. These validation studies represent retrospective analyses on a subset of the patients from the prospectively designed QUASAR trial. Within the constraints of these limitations, recent publications have shown that the OncotypeDx Colon assay is a valid predictor of relapse-free survival but is not a valid predictor of treatment response. A similar product, ColoPrint (Agendia, Irvine, CA), is an 18-gene profile that stratifies CRC patients into high-risk and low-risk categories. Finally, other approaches such as improved detection of micrometastases have been proposed. Reverse transcriptase–polymerase chain reaction for guanylyl cyclase C (GUCY2C), for example, has been shown to “upstage” patients by detecting nodal metastases that were otherwise undetected by traditional pathologic methods. Although these new molecular profiling methods clearly hold promise in predicting prognosis, none have yet been shown to predict response to therapy. As such, their clinical utility in directing treatment decisions will require further study.
Targeted Therapy
In addition to identifying molecules that may predict prognosis and response to therapy, research efforts are increasingly focused on identifying molecular targets for tumor-specific therapy. Several molecular targets hold promise in CRC. TKIs (anti-EGFR and anti-BRAF), discussed earlier, have been the most widely studied. Angiogenesis inhibitors (anti–vascular endothelial growth factor [VEGF]) also have shown promise in treating a variety of cancers, but results in CRC have been mixed. Bevacizumab (Avastin), an anti–VEGF-A antibody, first showed efficacy in metastatic disease and has been used as both first-line and second-line therapy in stage IV CRC. The BRiTE (Bevacizumab Regimens’ Investigation of Treatment Effects) study recently examined the efficacy of bevacizumab combined with chemotherapy as first-line treatment for metastatic CRC. At 20 months, progression-free survival was observed in 22% of patients who had received bevacizumab, whereas disease progression was seen in 79% of the patients. In addition, 66% of patients died during the study period, and 12% either withdrew from the study or were lost to follow-up. In addition to these sobering outcomes, toxicity is not insignificant, and the long-term benefit of bevacizumab therapy in CRC remains to be seen.
Another recent molecule of interest is focal adhesion kinase (FAK). FAK is a nonreceptor tyrosine kinase that was first identified at the sites of adhesion between cells and the extracellular matrix. FAK is known to be overexpressed in metastatic colon cancer, and phosphorylated (activated) FAK is also increased in colorectal tumor cells. Given its apparent role in tumorigenesis and overexpression in many types of cancers, FAK inhibition seems an appropriate approach to targeted cancer treatment. Recent work has shown that FAK inhibition with small-molecule inhibitors decreases colon cancer cell growth both in vitro and in vivo. Moreover, dual inhibition with other molecules such as hyaluronan synthase (HAS) appears to have synergistic effects on growth. These preclinical data suggest that FAK inhibition may offer another therapeutic target for treating patients with CRC.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree