6
BASIC TREATMENT PLANNING
Question 2
What is the main advantage of treating patients in the prone position with a belly board for patients with rectal cancer?
Question 3
What is bolus?
Question 4
What is the definition of a hot spot in an external beam plan?
With a patient in supine position, a 5° posteriorly titled gantry angle resulting in 275° gantry angle from the patient’s right and 85° gantry angle from the patient’s left, will avoid the divergence of the beams into the lenses and minimize the lens dose.
Answer 2
A belly board has an indented space for the entire abdomen to fall into, displacing the small bowel more anteriorly and further separating it from the tumor target volume, and minimizing the radiation dose to the small bowel. Another frequently used technique that also decreases the amount of small bowel in the field is to treat the patient with a full bladder. The full bladder will push the tumor volume inferiorly and separate the small bowel away from the tumor volume.
Answer 3
Bolus is any material (typically water equivalent) added on or near the patient surface. The use of bolus is to increase the surface (skin) dose when the tumor volume is located superficially. Sometimes bolus is also used to compensate for missing tissue such as in the treatment of an orbit when the eye has been removed.
Answer 4
A hot spot is a small volume that receives the highest radiation dose, higher than the prescribed dose of the target volume. In conventional radiation therapy, prior to the use of three-dimensional (3D) images and dose calculation, a hot spot was defined as an area encompassing 2 cm2 contiguous area that receives the highest radiation dose. In 3D conformal therapy (3DCRT), a hot spot is defined as a volume (0.03 mL) receiving the highest radiation dose.
When parallel opposed fields (anterior-posterior and posterior-anterior [AP/PA]) are used to treat a tumor in the chest region and the isocenter is located at mid-depth, in which field is the length of cord treated longer?
Question 6
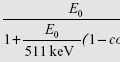
What is the geometric penumbra (P) at the skin given the following data: source size = 2 cm, source to skin distance (SSD) = 100 cm, source to collimator distance (SCD) = 56 cm?
Question 7
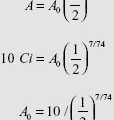
What happens to the size of the penumbra at a depth of 10 cm? (Assume the other parameters from Question 6 remain the same.)
Question 8
What would be the equivalent square for an open 8 cm × 24 cm field size?
The cord is located posteriorly in the patient body. Therefore, the length of cord included in the anterior field is greater than that in the posterior field due to beam divergence. The two beams treat the same area only at the depth of the isocenter.
Answer 6
Use the following formula:
Answer 7
Penumbra (P) width increases with an increase in depth assuming source to skin distance (SSD), source to collimator distance (SCD), and source size remain the same.
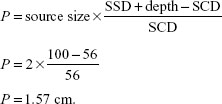
Answer 8
Use the following formula:
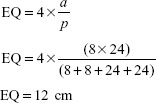
Where a is the area and p is the perimeter. The equivalent square has the same percent depth dose (PDD) as the rectangle, and can be used for monitor unit calculation for the rectangle. The formula is based on equating the ratio of area/perimeter between the square and rectangle.
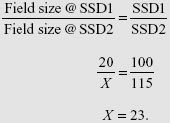
A 20 cm × 20 cm field size at 100 cm source to skin distance (SSD) will be projected to what size at a depth of 15 cm from the skin?
Question 10
What is the principal advantage of isocentric techniques over source to skin distance (SSD) technique for a treatment with multiple fields?
Question 11
What is the wedge transmission factor if the output without the wedge is 222 cGy/MU and the output with the wedge at the same point is 125 cGy/MU?
Question 12
An object that measures 4 cm is placed on the patient’s skin at 100 cm source to skin distance (SSD). Its image on the radiograph measures 5.4 cm. What is the target to film distance (TFD)?
The field size at a depth of 15 cm will be projected to 23 cm × 23 cm using the following similar triangles formula:
Answer 10
The isocentric technique eliminates the need to move the patient between fields. The isocenter is placed within the patient at a planned depth and the beams are directed from different directions. This technique relies primarily on the accuracy of machine isocentricity and not on the skin marks which can be unreliable points of reference.
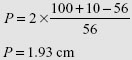
Answer 11
The wedge transmission factor is 0.563 using the following formula:
![]()
The wedge transmission factor (or simply wedge factor) is defined as the ratio of output with the wedge divided by the output without the wedge. Due to the large thickness of the wedge, the wedge factor makes a substantial adjustment in monitor units.
Answer 12
The TFD is 135 cm using the following formula:
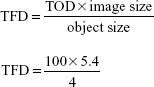
where TOD is the target object distance. As the object is on the skin, the TOD equals the SSD.
What is the main advantage for treating patients with breast cancer in a prone position?
Question 14
When planning for whole breast treatment using tangent fields, how is the separation defined? At what separation should one consider increasing the beam energy from 6 to 10 MV to maintain a uniform dose distribution?
Question 15
Calculate the field gap on the patient’s skin surface for the following two fields to be matched at a depth of 5 cm from the skin surface.
12 cm W × 20 cm L at 100 cm source to skin distance (SSD)
12 cm W × 24 cm L at 100 cm SSD
Question 16
Calculate the angle of the lateral tangent beam for a breast treatment if the medial tangent beam is at the gantry angle of 56° and a symmetric field size of 10 cm (Width) and 18 cm (Length) at 100 cm source to axis distance (SAD) is used.
For patients with the tumor cavity away from the chest wall or for patients with pendulous breasts, treating these patients in a prone position decreases the radiation dose to the lungs and heart. Another method to reduce radiation dose to the heart for patients with left-sided breast cancer is to treat patient with a breath-hold technique.
Answer 14
The separation is measured as the distance between the entrances of two tangential beams. If the separation exceeded 23 cm, increasing the beam energy from 6 to 10 MV can improve dose uniformity inside the breast (<110% of the prescription dose).
Answer 15
The gap would be 1.1 cm on the skin surface for these fields using the following formula:
![]()
where L1 is the length of the first field, L2 is the length of the second field, and d is the depth at which the fields are to be matched
![]()
Answer 16
According to the formula, ![]()
Opposed tangent angle = Angle + 180° − (2 × divergence)
![]()
56°+180°− (2×2.86)=230.28°.
A physician wants to treat a patient with medulloblastoma using four craniospinal fields (two lateral brain fields and two spinal fields). The brain field is 20 cm long with a source to skin distance (SSD) of 100 cm and designed using a half beam block technique. The spinal fields are 40 and 20 cm with a skin gap between them. Both spinal fields are designed at SSD of 100 cm. The junction point is at depth of 7 cm. Where do the hot and cold spots happen?
Question 18
What can be done to avoid or minimize the effects of cold and hot spots?
Question 19
What is the dose from each field at the junction point?
Question 20
Draw a diagram and calculate the skin gap for the spinal fields.
The cold spots happen between the gap left on the skin surface and junction point. The hot spot occurs where the beams overlap at depth.
Answer 18
A procedure called “feathering” is usually performed by changing the position of field edges between fractions during the course of the treatment. This way hot and cold spots are moved around and their effects are diffused.
Answer 19
The dose from each field is 50% of the prescribed dose at the same depth for each field. This way a uniform dose is achieved throughout the treatment area at the same depth.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree