Asthma Diagnosis
Stephen C. Lazarus
I. INTRODUCTION
Asthma is among the most prevalent chronic diseases in the United States and most of the developed world. Although the absence of a widely accepted definition of asthma makes it difficult to compare epidemiologic reports from different geographic regions, estimates suggest that there were 300 million people with asthma worldwide in 2010. Prevalence is greater in the United States than in developing countries, though the rate is increasing in both.
Asthma prevalence in the United States increased since the 1980s across all age, sex, and racial groups. The average prevalence in the United States in 2008 was 8.5%; in 2009, there were 250,000 deaths from asthma worldwide. In the United States, annual deaths from asthma increased from 2,598 in 1979 to 5,438 in 1998 before decreasing to 3,613 in 2006. Women account for 65% of all asthma deaths, and African Americans are three times more likely to die from asthma. The annual cost for asthma care is approximately $18 billion.
II. DEFINITION
Once thought of as a disease of abnormal airway smooth muscle with psychological overlay, the definition of asthma has changed with greater understanding of the inflammatory pathophysiology underlying the disease. There are too many mast cells, eosinophils, T lymphocytes, macrophages, and neutrophils in the airway epithelium and submucosa of people with asthma—even when their asthma is well controlled. This inflammation is linked causally to the nonspecific bronchial hyperresponsiveness that is ubiquitous in asthma. In addition, if the inflammation is not adequately treated, it leads in some patients to deposition of collagen in the subepithelial reticular layer (“remodeling”) and fixed (nonreversible) airflow obstruction. In its 2010 update, the Global Initiative for Asthma (GINA) program describes asthma as follows:
“Asthma is a chronic inflammatory disorder of the airways in which many cells and cellular elements play a role. The chronic inflammation is associated with airway hyperresponsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness, and coughing, particularly at night or in the early morning. These episodes are usually associated with widespread, but variable, airflow obstruction within the lung that is often reversible either spontaneously or with treatment.” (Global Strategy for Asthma Management and Prevention, used with permission from the Global Initiative for Asthma (GINA), http://www.ginasthma.org/)
This new definition, with its emphasis on inflammation, leads to increased emphasis on understanding and treating the airway inflammation that occurs in asthma.
III. CLINICAL FEATURES THAT DIAGNOSE ASTHMA
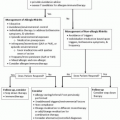
There is no one test that establishes the diagnosis of asthma. As a result, the diagnosis depends on clinical observations, including history, physical examination, and laboratory tests. Symptoms, physical findings, and laboratory results in asthma can overlap with other conditions (e.g., chronic obstructive pulmonary disease (COPD), congestive heart failure (CHF), vocal cord dysfunction), and at times the diagnosis of asthma cannot be confirmed until these other diagnoses are excluded. When the clinical features are straightforward, clinicians can make the diagnosis of asthma with minimal need for specific testing; when there is a question, pulmonary function tests and bronchoprovocation testing may be required.
IV. HISTORY
By definition, the clinical manifestations of asthma vary over time, and because of recall issues, many patients may not provide a classical description of asthma on their own. In addition, some symptoms are so nonspecific that patients attribute them to other conditions (e.g., age, smoking, infection, allergies). Targeted questioning can be revealing and should ask not only about wheezing and shortness of breath but also about cough, chest tightness, triggers, nocturnal symptoms, and prolonged coughing after “colds.”
A. Common symptoms
The most common symptoms of asthma are recurrent chest tightness, wheezing, and cough. Shortness of breath is frequent. Approximately 80% of patients with asthma produce sputum at some point, often during the most severe part of an exacerbation or immediately thereafter. However, mucus hypersecretion and hypertrophy of mucus secretory cells (e.g., goblet cells, mucus glands) can occur in nonexacerbated asthma and are seen even in mild asthma. Asthma exacerbations are usually characterized by cough, wheezing, and dyspnea, but any one of these can predominate.
Chest tightness, wheezing, cough, and dyspnea are all manifestations of the change in airway caliber (“bronchoconstriction”) that occurs in asthma. Wheezing results from turbulent flow through constricted airways, and cough usually results when stimulation of sensory nerves, found throughout the larger, central airways at bifurcations, occurs as a result of bronchoconstriction and mucosal folding. The pattern of symptoms can be an important variable and is often critical in differentiating asthma from other diseases that cause similar symptoms.
B. Symptoms with upper respiratory infections
Because patients with asthma have increased bronchial reactivity, anything that irritates the airway has the potential to cause bronchoconstriction. In addition, a number of respiratory viruses will increase bronchial reactivity, causing a significant shift in the dose-response to methacholine or histamine. Thus, many patients will report worsening of asthma symptoms that is triggered by respiratory infections, or cough, chest tightness, and wheezing that only occurs in the context of a respiratory infection.
C. Prolonged cough following an upper respiratory infection
Many patients with asthma are diagnosed after a number of years in which they report that routine respiratory viral infections “go to the chest,” and that cough following a minor respiratory illness frequently persists for
weeks to months. The diagnosis of asthma should be entertained when these symptoms are elicited, and either empiric therapy or diagnostic testing for asthma (e.g., spirometry, bronchoprovocation) should be considered. Respiratory viral infections can increase bronchial reactivity within 2 to 3 days, and this hyperreactivity can last for up to several months.
weeks to months. The diagnosis of asthma should be entertained when these symptoms are elicited, and either empiric therapy or diagnostic testing for asthma (e.g., spirometry, bronchoprovocation) should be considered. Respiratory viral infections can increase bronchial reactivity within 2 to 3 days, and this hyperreactivity can last for up to several months.
D. Symptoms at night
Asthma symptoms at night are common yet frequently overlooked. Unless they dramatically interfere with sleep, many patients neglect to report them. Thus, clinicians should specifically ask about cough and wheeze at night. Nocturnal symptoms are likely due to a combination of diurnal variation in systemic cortisol and catecholamine levels, increased allergen levels in the bedroom, and gastroesophageal reflux. Studies using bronchoscopy with bronchoaleolar lavage and endobronchial biopsies demonstrate that increased airway inflammation peaks at about 4 a.m. Most deaths from asthma outside of hospitals occur at night, especially in the predawn hours.
E. Symptoms with exertion
Exercise-induced bronchoconstriction is a well-described entity (see below), but not all exercise-associated dyspnea is due to exercise-induced bronchoconstriction. Individuals with preexisting obstructive or restrictive lung disease can develop dyspnea with exertion, without a change in lung function. Similarly, dyspnea with exertion can be a manifestation of deconditioning or cardiac disease.
F. Response to bronchodilator
The classic definition of asthma described bronchoconstriction that was variable and reversible either spontaneously or with bronchodilators, and most patients with asthma were expected to have normal or near-normal lung function between exacerbations. We now know that some asthmatics develop “remodeling” and that as a result their airflow obstruction may not reverse fully. Nevertheless, we expect that most asthmatics will demonstrate significant reversal of airflow obstruction with associated reduction in symptoms after aerosolized albuterol is administered. If the clinical picture highly suggests asthma, a clinical response to empiric bronchodilator treatment can confirm the diagnosis.
G. Cough variant asthma
In some patients with asthma, cough is the major, or only, symptom, and wheezing is absent. When this occurs, it is referred to as cough variant asthma. In these patients, baseline airway function is usually normal, but there is significant variability in peak expiratory flow or FEV1, and there is heightened airway reactivity. Monitoring daily peak expiratory flow, or performing bronchoprovocation testing with methacholine, can be helpful in making this diagnosis.
H. Childhood versus adult onset
Although asthma may develop at any age, epidemiological studies show that onset of symptoms in childhood is more common. Twin studies suggest that early-onset asthma has a greater genetic component than does late-onset asthma. Asthma is more common in male children, perhaps because they have smaller airways and more atopy. In adults, asthma prevalence is greater in women, and the greater risk of adult-onset asthma in women is likely due, at least in part, to sex hormones.
V. RISK FACTORS
Numerous factors, including genetics, perinatal exposures, sex, atopy, respiratory infections, aeroallergens, tobacco smoke, and environmental pollutants, are all associated with the development of asthma. There is growing evidence that asthma is phenotypically heterogeneous, and different factors may be more important in different asthma phenotypes. Similarly, it is likely that different phenotypes are associated with different genotypes. Gene-by-gene and gene-by-environment interactions combine to determine asthma susceptibility and asthma phenotype. The “Asthma Predictive Index” identifies risk factors for the development of persistent asthma after the age of 5. Children younger than three who have had ≥4 episodes of wheezing in the previous year are significantly likely to develop persistent asthma if they have any of the following:
A parental history of asthma
A physician diagnosis of atopic dermatitis
Evidence of sensitization to aeroallergens
Two (or more) of the following:
Sensitization (antigen-specific IgE) to foods
≥4% Eosinophilia
Wheezing (apart from respiratory viral infections)
The validity of this predictive index is being tested in many large cohorts and studies.
A. Family history and genetics
Asthma is more common in children whose parents have asthma, but a clearly heritable genetic component has not been identified. Inheritance of asthma does not follow a simple Mendelian pattern, suggesting that multiple genes are involved. Genes associated with atopy and production of IgE are localized to the long arm of chromosome 5, where genes associated with TH2 cytokines, the beta2-adrenergic receptor, and with the development of airway hyperresponsiveness are also located. Despite these associations, specific asthma susceptibility genes have not been identified.
B. Environmental factors
Environmental exposures such as air pollutants and aeroallergens play an important role as triggers of asthma symptoms, but their role in the pathogenesis of asthma is less clear. Sensitization to common indoor allergens such as house dust mite, mold, and dog and cat dander is an independent risk factor for wheezing in young children; however, the link with development of asthma is tenuous. In fact, in some studies, children who were exposed to dogs or cats in the first years of life were actually protected against allergic sensitization and the development of asthma. Exposure to tobacco smoke in utero and in early infancy increases fourfold the risk of developing asthmalike symptoms (wheezing) in the first year of life. Both indoor (e.g., smoke from biomass fuels) and outdoor (e.g., smog) air pollutants are associated with asthma symptoms in patients with established disease, but their role as a cause of asthma has not been proven. Epidemiologic studies demonstrate a link between outdoor exercise in communities with high ambient ozone levels and the risk of asthma among school-age children. Occupational asthma is defined as asthma caused by an exposure to an agent encountered in the work environment. The list of agents is long and includes highly reactive molecules such as isocyanates (manufacture of plastics, automobile
painting), irritants (detergent enzymes, disinfectants, manufacturing), and immunogens. Frequently, workers are not aware of the specific chemicals to which they are exposed, and targeted questions may be required to uncover the nature of their work exposures (e.g., “Describe exactly what you do at work.”) Also, office workers in factories may not realize that they share some exposures with the factory workers. Although most occupational asthma is immunologically mediated, a latency period of months to years is common.
painting), irritants (detergent enzymes, disinfectants, manufacturing), and immunogens. Frequently, workers are not aware of the specific chemicals to which they are exposed, and targeted questions may be required to uncover the nature of their work exposures (e.g., “Describe exactly what you do at work.”) Also, office workers in factories may not realize that they share some exposures with the factory workers. Although most occupational asthma is immunologically mediated, a latency period of months to years is common.
C. Atopy and eczema
Atopy refers to the predilection to develop IgE-mediated responses to environmental allergens. It is identified by the presence of elevated serum IgE, peripheral blood eosinophilia, and skin test reactivity to specific allergens. Atopy is associated with asthma, allergic rhinitis, and atopic dermatitis (eczema). The latest revision of the National Heart Lung Blood Institute’s Guidelines for the Diagnosis and Management of Asthma (EPR3) describes atopy as the strongest identifiable predisposing factor for developing asthma. Although this association is strong, the mechanisms by which atopy and asthma are linked are not well understood. As described above, genes associated with atopy colocalize with genes linked to TH2 differentiation and to bronchial hyperreactivity. Elevated IgE in young children is a risk factor for the subsequent diagnosis of asthma, and asthma prevalence is correlated with serum IgE levels and positive allergen skin tests.
D. Infection
The role of respiratory infections in the pathogenesis of asthma is unclear. Respiratory syncytial virus and parainfluenza virus are frequently associated with wheezing in infants, and approximately 40% of children hospitalized with respiratory syncytial virus infection will continue to wheeze or have asthma after age 7. In contrast to these data are those suggesting that respiratory infections early in life may actually provide protection against the development of asthma. The observation that asthma is less common in younger siblings, in children who attend group daycare, and in rural and underdeveloped communities has led to the “hygiene hypothesis” that suggests that childhood respiratory infections and/or regular exposure to endotoxin from farm animals may drive undifferentiated (null or TH0) T cells toward a TH1 and away from a TH2 phenotype (see Chapter 1). TH2 cells, defined by their cytokine profile (IL-3, IL-4, IL-5, GM-CSF), can be thought of as proallergic or proatopic and are found in increased numbers in the airways of asthmatics. There is a linear inverse relationship between the diversity of bacteria collected in bedroom dust and the prevalence of asthma in children.
VI. TRIGGERS
Asthma symptoms or exacerbations can be provoked by a number of triggers that can be either specific (e.g., specific allergens to which an individual is sensitized) or nonspecific (e.g., respiratory infection, air pollution). The initial history should solicit information about pets in the home, exposure to mold or dust, and occupational exposures. Although many patients can easily identify allergic triggers, others may require allergy skin tests to identify potential triggers. It is important to note that demonstrating allergen-specific sensitization does not prove that a given antigen is responsible for asthma symptoms. It can,




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree