Assessment of the Breast
Triple assessment
|
Triple assessment is the combination of clinical, radiological, and pathological evaluation of a breast lesion (Table 2.1). Triple assessment should be used in all patients with a suspected breast lump and may be relevant in those with other symptoms. Imaging assessment consists of mammography (in those aged 35 years or over), and ultrasonography is recommended for all palpable and significant radiological abnormalities (at any age). Histological assessment usually involves core biopsy and/or fine needle aspiration (FNA) cytology. This combination of techniques increases the reliability of determining the cause of a clinical or image-detected abnormality (Tables 2.2, 2.3). It is
recommended that all elements of the assessment process are reported on a scale of 1-5 with increasing concern of malignancy. In a patient with a discrete breast mass or abnormality seen on imaging, some centres offer immediate reporting of imaging and cytology of fine needle aspirates or touch preparation cytology from a core biopsy. ‘One stop’ clinics have advantages for women with benign lumps who can be reassured and discharged after a single visit but are only likely to be cost effective in centres seeing large patient volumes.
recommended that all elements of the assessment process are reported on a scale of 1-5 with increasing concern of malignancy. In a patient with a discrete breast mass or abnormality seen on imaging, some centres offer immediate reporting of imaging and cytology of fine needle aspirates or touch preparation cytology from a core biopsy. ‘One stop’ clinics have advantages for women with benign lumps who can be reassured and discharged after a single visit but are only likely to be cost effective in centres seeing large patient volumes.
Table 2.1 Scoring system for triple assessment | |||||
|---|---|---|---|---|---|
|
Table 2.2 Accuracy of investigations in symptomatic breast clinic | ||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||
Table 2.3 Symptoms and cancer risk in those attending a symptomatic clinic | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Clinical history
A history is taken from the patient of the duration and nature of presenting symptoms. Further specific details of individual symptoms are of value and are outlined below. Past personal or familial breast problems should be elucidated. General factors such as past medical history, drugs, and allergies should be recorded. Hormonal risk factors for cancer such as age of menarche and menopause, parity, age of first birth, breast feeding, oral contraceptive or hormone replacement therapy use are traditionally documented, although they are of no value in achieving a diagnosis in an individual case. The history and examination findings should be recorded legibly and contemporaneously in the medical records, often on a standard form.
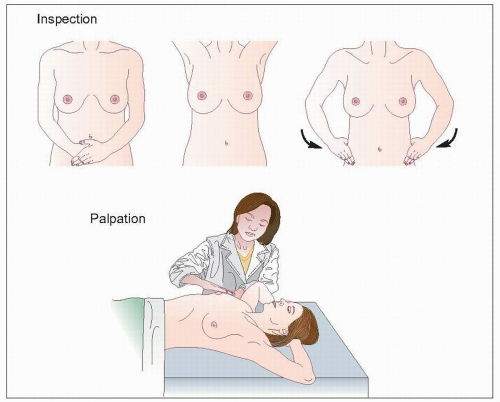
Breast examination should be conducted in a good light with the patient stripped to the waist in the presence of a chaperone. Initial examination is by inspection with the patient in the sitting position with hands by her side, paying particular attention to symmetry, nipple inversion, skin changes, and alterations in breast contour. The breast should also be inspected both with arms raised and with the chest wall muscles tensed and changes in the dynamic setting noted.
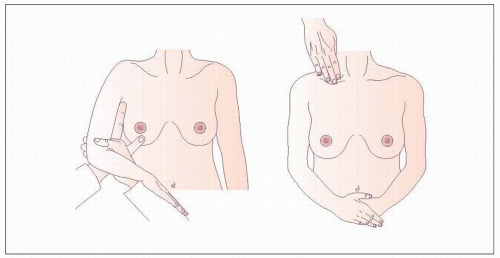
Palpation of the breasts is best performed in the supine position with the head supported and the arms above the head. Putting the hands above the head spreads the breast out over the chest wall and reduces the depth of breast tissue between the examiner’s hands and the chest wall, and makes abnormal areas much easier to detect and define. All the breast tissue is examined using the most sensitive part of the hand, the fingertips. If an abnormality is identified, then it should be assessed for contour, texture, and any deep fixation by tensing the pectoralis major. All palpable lesions should be measured with callipers.
If there is a history of nipple discharge, the nipple should be gently squeezed to determine whether a pathological discharge is present. Careful note should be taken of whether discharge is emerging from single or multiple ducts and whether blood is present either frankly or on dipstick testing.
All women complaining of breast pain or tenderness should be examined for tenderness of the chest wall. With the patient in the sitting position, the hand may be pushed up behind the breast from below with pressure on the chest wall. The patient may also be rolled onto their side, allowing the breast to fall medially, exposing the edge of the pectoral muscle to palpation. The patient should be asked to indicate if there is any localized tenderness on palpation of the chest wall, and whether any discomfort evident during examination is similar to the pain they normally experience. Allowing the woman herself to confirm that the site of maximal tenderness is in the underlying chest wall rather than the breast is effective in reassuring patients that there is no significant breast problem.
The axilla is best examined with the patient sitting. The
examiner’s ipsilateral arm supports the patient’s arm while the examiner’s contralateral hand is placed high in the axilla on the chest wall and run carefully downwards. The supraclavicular fossa is examined from behind with the patient in a sitting position. A general examination of the cardiovascular and respiratory systems is useful in those in whom surgery is contemplated. If metastatic disease is suspected, then examination for bony tenderness, hepatomegaly, and pleural effusion may be valuable.
examiner’s ipsilateral arm supports the patient’s arm while the examiner’s contralateral hand is placed high in the axilla on the chest wall and run carefully downwards. The supraclavicular fossa is examined from behind with the patient in a sitting position. A general examination of the cardiovascular and respiratory systems is useful in those in whom surgery is contemplated. If metastatic disease is suspected, then examination for bony tenderness, hepatomegaly, and pleural effusion may be valuable.