Fig. 18.1
Demonstrating the six approaches to the SMA. S superior approach, P posterior approach, R right/medial uncinate approach, M mesenteric approach, L left posterior approach, A anterior approach
18.1.1.1 Posterior Approach
The first technical description of AFA was described in 2003 by Pessaux et al. [8], and this was for a posterior approach to the SMA. The posterior approach is the most commonly performed technique, and there have been several modifications [9–11]. Following an initial exploratory laparotomy, an extended kocherization of the duodenum is performed exposing the inferior vena cava, left renal vein and abdominal aorta. This is assisted by full mobilization of the right colon and hepatic flexure to the left of midline. The pulsations of the SMA are identified in front the left renal vein, and the perivascular connective tissue is incised to expose the adventitia of the SMA. The dissection on the adventitia of the SMA is continued in a caudal direction posterior to the pancreatic head to where it crosses the third part of the duodenum further dividing the attachments between the SMA and uncinate process to expose the border of the PV–SMV. The origins of the superior pancreaticoduodenal and inferior pancreaticoduodenal (IPDA) arteries are divided as they enter the pancreatic head and uncinate process, respectively. Care must be taken to identify a replaced right hepatic artery that usually arises 1–2 cm from the origin of the SMA. By now, all of the connective tissue attachments between the PV and the SMA have also been divided, and a negative SMA margin confirmed, with frozen section if necessary.
18.1.1.2 Medial or Uncinate Approach
In 2010, Hackert and co-workers [12] described a medial or ‘uncinate-first’ approach to the SMA. Following an initial extended kocherization, a Cattell–Braasch manoeuvre is performed, which involves dissection along the right-sided white line of Toldt and then across the small bowel mesenteric root, which allows the colon and small bowel to be retracted well to the left, facilitating exposure of the SMV as it passes over the third part of the duodenum. The pancreas is dissected free from the SMV, often requiring the division of two or three venous tributaries. The duodenojejunal (DJ) flexure is then mobilized, and the proximal jejunum transected and transposed to the right abdomen by passing it behind the superior mesenteric vessels. Further exposure of the SMA and SMV is facilitated by division of proximal jejunum although this is not always necessary. The Cattell–Braasch manoeuvre facilitates retraction of the right colon and small bowel to the left, which lifts and rotates the SMV up and to the left, and with retraction of the third and fourth parts of the duodenum to the right, the SMA is rotated into view under the SMV. It is then possible to dissect down on the medial aspect of the SMA in a cephalad direction under the neck of the pancreas. The IPDA and RRHA are encountered and divided on the way, similar to the posterior approach.
A modified medial uncinate approach is described by Shukla and colleagues [13] in 2007 which entails division of the ligament of Treitz and translocation of the proximal jejunum with its intact mesentery into the supracolic compartment, by passing it to the right under the superior mesenteric vessels. This is said to facilitate alignment of the uncinate process with the jejunal mesentery, enabling easier dissection of the SMV and SMA.
18.1.1.3 Inferior Infracolic Approach (Mesenteric Approach)
In 2010, Weitz and co-workers [14] coined the term ‘artery-first approach’ and described the inferior approach to the SMA from the infracolic compartment, at the base of the transverse mesocolon. Mobilization of the DJ flexure is performed initially, and the peritoneum is divided over the palpable SMA. The SMA is exposed, with the SMV to the right. The middle colic artery is identified arising from the SMA and coursing anteriorly within the transverse mesocolon. The IPDA is identified on the right aspect of the SMA as it enters the uncinate process under the SMV. The IPDA is divided, and dissection continues up and along the anterior and right medial aspect of the SMA to its origin, under the neck of the pancreas and splenic vein. This approach exposes the SMA in the infracolic compartment at the root of the mesentery.
18.1.1.4 Left Posterior Approach
Kurosaki and colleagues in 2011 [15] described the left posterior approach to the superior mesenteric vascular pedicle. Following division of ligament of Treitz, the proximal jejunum is pulled to the left exposing the first and second jejunal arteries which are divided at their origin from the SMA. Further traction on the proximal jejunum produces a counterclockwise rotation to the SMA that allows identification and division of the IPDA, arising from the posterior surface of the SMA in addition to enabling clearance of the posterior and right aspects of the SMA. With the SMA freed and retracted to the right, and with the proximal jejunum still retracted to the left, the SMV appears under the SMA, and the first jejunal branch of the SMV is divided. The SMV is then skeletonized up to its confluence with the splenic vein. This frees the superior mesenteric pedicle from the uncinate process and the mesentery of the proximal jejunum. The jejunum is then divided and the duodenum transposed to the right, allowing exposure and division of the remaining connective tissue where it attaches to the superior mesenteric pedicle.
18.1.1.5 Inferior Supracolic Approach (Anterior Approach)
Hirota and co-workers [16] described the inferior supracolic approach in 2011. An initial division of the gastric antrum is described; however, it is possible to expose the pancreatic neck by cephalad retraction of the stomach after division of the gastrocolic ligament without division of the gastric antrum. The next step in this technique is to divide the pancreatic neck to expose the SMV–PV junction, but it is worth doing as much dissection as possible by elevating the inferior edge of the pancreas to determine resectability before division of the pancreas. The authors then describe the ‘hanging manoeuvre’, which involves passing a tape along the right surface of the aorta to the origin of the SMA and coeliac trunk, and then passing it between the CHA and the superior margin of the pancreatic neck, after first dissecting this area. Traction on this tape exposes the peripancreatic retroperitoneal margin with the neural plexi and lymphatics and facilitates their division. The next step is a ‘reversed kocherization’ with en bloc mobilization of the duodenum and pancreatic head, in a medial to right lateral direction, in a plane deep to Gerota’s fascia and anterior to the left renal vein and inferior vena cava. The disadvantage of the technique as originally described is the (irreversible) transection of the stomach and pancreatic neck at an early stage to achieve adequate exposure of the SMA, but this is not always necessary.
Inoue and colleagues [17] more recently described the supracolic anterior approach to the superior mesenteric artery with an aim to undertaking systematic mesopancreas dissection to achieve adequate clearance of perineural and lymphatic tissue and negative margins along the SMA. After an initial extended kocherization, the right side of the SMA root is identified in front of the LRV. The gastrocolic ligament and greater omentum are then dissected until the pancreas head is well exposed. The duodenum is dissected to the left, exposing the superior mesenteric vein (SMV) from the right side. The SMV is dissected and taped, and Henle’s gastrocolic trunk and inferior pancreaticoduodenal vein are sacrificed. By retracting the SMV leftward, the first jejunal vein is identified. This also enables visual inspection and palpation of the SMA. The mesopancreas division is initiated from the caudal end anteriorly to the immediate right of the JV, which would be preserved throughout dissection. The mesopancreas is divided layer to layer exposing the IPDA. In cases where the uncinate process extends to the left of the SMA, the first jejunal vein is divided at its origin from the SMV to gain more access. If there is SMV involvement by the tumour, the dissection plane around the SMA is just outside of the adventitia usually from 11 to 5 o’clock, peeling off the nerve plexus around the SMA like a plate. In cases where there is a common trunk of IPDA and first jejunal artery, the common trunk is divided at its root. After separation of the SMA from the pancreatic head, the dissection is carried caudally until it reaches the left renal vein completing the SMA artery-first dissection.
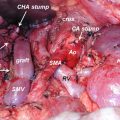
18.1.1.6 Superior Approach
In this approach, the hepatoduodenal ligament is dissected first to expose the CHA and the gastroduodenal artery by dissecting from right to left to remove the anterior lymph nodes en bloc or separately. The dissection is then carried down the coeliac trunk, inside the perineural and lymphatic tissue, on to the aorta and origin of the SMA, aided by caudal retraction of the pancreas.
18.1.2 Technical Description of Artery-First Approaches to Cancer of Pancreatic Body
More recently, an AFA has been described for borderline resectable pancreatic cancer of the body of the pancreas during the radical antegrade modular pancreatectomy (RAMP) [18, 19]. This facilitates the identification and dissection of the SMA behind the body of the pancreas. Following an initial exploratory laparotomy, the ligament of Treitz is divided to expose the left side of the DJ flexure, and further dissection is carried out to expose the anterior surface of the aorta, IVC and left renal vein together with the origin of the SMA from the aorta. This enables adequate clearance of posterior surgical margin. The dissection is then directed to the supracolic compartment with division of the gastrocolic ligament thereby exposing the inferior border of the pancreas. The middle colic artery in the transverse mesocolon is traced caudally to help identify the SMA. The SMA is then fully exposed from the origin of the middle colic artery to the origin of the SMA. If there is tumour infiltration of the MCA and transverse mesocolon, resection of these should be undertaken, and in the majority of cases, the marginal artery of Drummond is sufficient. Following confirmation of clear SMA margins, the PV–SMV trunk is freed from the posterior aspect of the pancreas. This will enable passage of a dissecting forceps from the inferior border of the pancreas, anterior to the SMA towards the inferior border of the coeliac trunk. This technique termed as the pancreas hanging manoeuvre enables or allows elevation of the pancreas away from the SMA to obtain a wide view of the anterior surface of the SMA. A standard radical antegrade modular pancreatosplenectomy (RAMPS) procedure is then undertaken to complete the pancreatosplenectomy (Ref).
Indications, advantages and disadvantages of the AFAs are summarized in Table 18.1.
Table 18.1
Summary of indications, advantages and disadvantages of various ‘artery-first approaches’
Approach | References
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|
|---|