Approach to the Patient with Recurrent Infections
Zuhair K. Ballas
INTRODUCTION
The environment is rife with multiple microorganisms. In addition to the microorganisms that surround us, microorganisms are an integral part of our biologic makeup. It is estimated that the microorganisms in a human outnumber the body cells by up to 10:1. Thus, for example, the skin supports a high density of microorganisms, the sinonasal tissue and the oral cavity are host to multitudes of organisms, and the colon is estimated to have as much as 1010 organisms per gram of tissue. It is therefore not surprising that humans get infected as much as it is surprising that normal subjects rarely get infected
I. PHYSICAL BARRIERS
While immune mechanisms are integral in the defense against infections, nonspecific defenses play an equally important role in the defense against infections. Thus, an intact skin is an essential part of the defense against infection, and it is well established that it takes very few bacteria to infect a wound compared to a multitude that is needed to infect an intact skin. The skin defends against infection not just by being a physical barrier but by the local production of fatty acids that have potent antimicrobial activity. Mucosal surfaces also have several molecules that are produced locally, such as defensins, which have antimicrobial activity. Other nonspecific local defenses include cilia, which act as a “mop” to sweep away microbes, and mucus, which serves as a “rinsing” agent. The importance of an optimal production and viscosity of mucus is best illustrated by cystic fibrosis where excessively viscous mucus is not efficient at cleaning mucosal surfaces. Acidic pH in the stomach acts as a potent antimicrobial agent; it is not unusual to hear of cases where the same load of bacteria may or may not produce food poisoning depending on whether it was consumed on an empty (acidic) or full (neutral or basic pH) stomach. Indeed, it has been known for some time that gastrectomy is associated with an increased incidence of mycobacterial infection. It is therefore important that the status of the various barriers be examined first in any patient with a history suggestive of recurrent infections especially if such infections are limited to one organ system.
II. COMORBIDITIES
Secondary immunodeficiencies leading to recurrent infections are much more common than primary immunodeficiencies. Worldwide, malnutrition is probably the most common cause of recurrent infections. In North America, primary malnutrition may not be as common, but malnutrition in the “older old” (those over 75 years of age) is becoming, and will continue to become, a common occurrence.
Other common causes of secondary immunodeficiency include:
HIV
Malignancy
Metabolic diseases (diabetes, severe liver disease, chronic kidney disease)
Immunosuppressive drugs (chemotherapy or antigraft rejection drugs in the setting of organ transplantation)
Immunomodulatory agents (e.g., TNF antagonists, rituximab, abatacept)
Drug-induced hypogammaglobulinemia (especially antiepileptics such as diphenylhydantoin, carbamazepine, valproate)
Protein loss through the GI tract or through the kidneys or secondary to severe burns
III. RECOGNITION OF VARIOUS MICROORGANISMS
The tug-of-war between host and pathogen has been going on for millennia. The phylogeny of primitive, nonspecific, or “innate” immune defenses predates the advent of antigen-specific immune responses. Nevertheless, innate immune mechanisms persist in humans and are the first line of defense against most microorganisms. Innate immunity has “sensors” which recognize molecular patterns rather than specific antigens as is the case with adaptive immunity. Redundancy is a well-known characteristic of adaptive immune responses, but redundancy is also prevalent in innate immunity in that a given molecular pattern may be recognized by more than one nonspecific innate immune “sensor.” A classically recognized innate immune “sensor” is mannose-binding protein on the surface of neutrophils and macrophages, which binds to mannose on the surface of gram-negative bacteria and some fungi. Another well-known innate sensor is the mannan-binding lectin pathway of the complement system. Several other innate “sensors” have been recognized recently, and they belong to distinct “families” (with more to be characterized):
Toll-like receptors (TLR)
C-type lectin receptors (CLRs)
Nucleotide-oligomerization domain (NOD) proteins
NOD-like receptors (NLR)
Retinoic acid-inducible gene I(RIG-I)-like receptors (RLR)
Binding to these pattern recognition receptors activates signal transduction pathways that result in the activation of cytoplasmic and nuclear factors that ultimately result in the transcription, translation and secretion of various inflammatory mediators, cytokines, and chemokines, and the generation of reactive oxygen species and various antimicrobial effectors. To date, TLR are the most extensively studied pattern recognition receptors. For example, endotoxin is expressed on gram-negative bacteria and is recognized by TLR4. Lipoteichoic acid is expressed on some gram-positive bacteria and is recognized by TLR2. A simplified pattern of recognition by the various TLR is shown in Table 19-1.
The function of innate sensors is to facilitate phagocytosis and intracellular killing by the elaboration of intracellular antimicrobial mechanisms. This process is probably of most importance in defense against pathogens that enter through mucosal surfaces. In addition to phagocytes, NK and NKT cells are part of the innate immune systems and are thought to be the major and earliest producers of interferon and IL4 which in turn activate the adaptive immune system.
Table 19-1 TLR and Their Recognition Pattern | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Other locally important mechanisms aimed at limiting pathogen invasion and spread include the coagulation pathway and the elaboration of vasoactive molecules leading to vasoconstriction.
One of the mechanisms by which ingested organisms are destroyed is the generation of reactive oxygen species (ROS) by macrophages or neutrophils. Some organisms produce catalase which inactivates ROS. Therefore, if the host’s oxidative pathway is suboptimal (as occurs in chronic granulomatous disease), there will be an increased incidence of infection by catalase-producing organisms such as Candida, Aspergillus fumigatus, Staphylococcus aureus, Klebsiella, Serratia, and Pseudomonas.
In the tug-of-war between microorganisms and host defenses, some bacteria evolved a “capsule.” Encapsulated bacteria use their polysaccharide capsules to hide some of their surface molecules. In response, the host adopted a new defense strategy aimed at recognition of the capsular polysaccharide with the same ultimate goal of promoting phagocytosis. This recognition is mediated by antibodies generated to recognize the capsule. The antibody-antigen complex will activate complement thus facilitating opsonization and the ingestion of the encapsulated bacteria. For reasons not entirely clear, the terminal complement components are important in defense against Neisseria species.
The primary strategy in the defense against gram-negative and encapsulated bacteria is to facilitate phagocytosis since once ingested, these organisms are readily digested. However, some organisms, such as mycobacteria, are resistant to intracellular digestion by resting macrophages. The strategy for such organisms is to activate the macrophages by marshaling T-cell responses, CD4 T cells in particular, which secrete cytokines such as interferon gamma (IFNγ). Once activated, macrophages are able to neutralize most intracellular organisms.
For viruses, a different strategy was needed since they do not usually infect professional phagocytes, so the macrophage activation approach is not feasible. For such organisms, the development of cytotoxic T lymphocytes (which can be CD4 but usually are CD8) was needed.
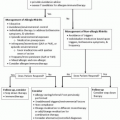
It is therefore apparent that the type of organisms seen in a patient with recurrent infections should give an indication as to which arm of the immune system is likely to be dysfunctional (Table 19-2).
The above scheme applies for most of the commonly encountered immunodeficiencies. Recent advances, however, suggest that the immune system is far




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree