FIGURE 5.1
The measurement of LDL-C has major limitations, which have not received the attention the issue deserves. If LDL-C is calculated by the Friedewald formula, as it is in the majority of laboratories, a fasting blood sample is necessary and the measurement is, unfortunately, as evaluated by the American Association Clinical Chemistry, often not acceptably precise.199 Not only is the measurement of LDL-C imprecise, it is also not standardized,199 which means the results from one laboratory will not necessarily be the same as the results from another, which means that tracking and interpreting the results of therapy or even of spontaneous changes over time will be difficult, if not impossible. Importantly, these errors are random and random errors due to imprecision of measurement cancel out in large surveys. Thus, the limitations that make LDL-C so poor a clinical tool for individual patients do not matter for the large studies that led guideline groups to recommend LDL-C as the standard of care.
On the other hand, if LDL-C is directly measured, as recommended by some guideline groups, there are multiple disadvantages199: 1) additional cost is added; 2) these methods are not standardized; 3) they are not validated in dyslipidemic serum; and 4) there is no epidemiological evidence that directly measured LDL-C is a more accurate measure of cardiovascular risk than the conventionally calculated LDL-C. Indeed the limited evidence available suggested the opposite to be the case.200
5.2.2 Non-HDL-C
Non-HDL-C is the arithmetic sum of the cholesterol in VLDL, IDL and LDL particles and, therefore, apoB and non-HDL-C seem like mirror images of each other with apoB measuring all the atherogenic particles and non-HDL-C measuring all the atherogenic cholesterol (Figure 5.1 ). No wonder so many argue that non-HDL-C is an acceptable surrogate for apoB and, given that no extra charge is required to calculate non-HDL-C, they conclude that non-HDL-C is superior to apoB. Furthermore, fasting samples are not required for non-HDL-C measurements and so apoB has no advantage on that front either.
Given that non-HDL-C includes the cholesterol in VLDL particles and given the high prevalence of hypertriglyceridemia in patients with vascular disease, it is not surprising that many experts attribute the increased cardiovascular risk in hypertriglyceridemic patients to so-called remnant particles within the VLDL density range. Unfortunately, the evidence that triglycerides increase risk remains incomplete. To be sure, recent Mendelian randomization studies suggest they do.201-203 However, we are not sure confounding with LDL particle number has been ruled out in these analyses. There is certainly no linear relation between plasma triglyceride levels and risk, not surprising, since the highest levels are associated with increases in chylomicron number not VLDL particle number. Moreover – and this is a fundamental limitation – no evidence has yet been presented from any of the fibrate or niacin or even the statin clinical trials that any clinical benefit follows lowering of triglycerides or VLDL-C.
Finally, apoB48 and apoB100 abnormal remnant lipoprotein particles only accumulate in large numbers in patients with remnant lipoprotein disorder, when they can equal or exceed the normal VLDL particle number. In all other subjects the number of atherogenic remnant particles is indeed very low. Let us do an easy calculation: The normal fasting concentration of apoB48 is approximately 0.5 mg/ml and doubles in the peak postprandial period. The normal concentration of VLDL particles is 10 mg/dl, a value that also rises postprandially. Thus, normally, there are 10 to 20 times more VLDL particles than remnant particles. Remnant particles are atherogenic but the risk attributable to remnants must relate to their number and, if the number is not markedly increased, the risk attributable to remnants should not be markedly increased. Indeed, in healthy subjects, there are never very many atherogenic remnant particles. Only in remnant lipoprotein disorder is the concentration of abnormal VLDL and chylomicron remnants 40-50 mg/dl and therefore there are 20 to 40 times more in those with remnant lipoprotein disorder than in other subjects.204 It is not surprising these patients have such an increased atherogenic risk.
Why Does VLDL-C not Explain Why non-HDL-C is a Better Marker of Cardiovascular Risk than LDL-C?
Based on our meta-analysis,205 as well as other evidence, we have concluded that non-HDL-C is a more accurate marker of cardiovascular risk than LDL-C. However, not all studies, the Emerging Risk Factor Collaboration (ERFC)206,207 for example, support this view. Those who conclude that non-HDL-C is superior to LDL-C assume this is due to the fact that non-HDL-C includes the cholesterol in VLDL and this increases the atherogenic risk. We will now try to demonstrate why this argument, which seems so common sense as to be inarguable, is more complex and less persuasive than it seems.
To begin with, since non-HDL-C is the simple sum of VLDL-C and LDL-C, this argument presumes the cholesterol in VLDL is as atherogenic as the cholesterol in LDL. But there is no direct evidence this is the case and given that LDL particles are so much smaller than VLDL particles and that there are so many more of them – 9 times more generally – the proposition the cholesterol in the much smaller number of the much larger VLDL particles is as dangerous, mmol for mmol, as the cholesterol in the much larger number of much smaller LDL particles seems, on the surface of it, unlikely. Nevertheless, let us examine in more detail the argument that the cholesterol in VLDL explains why non-HDL-C is a better marker of cardiovascular risk than LDL-C. The conventional method to express the risk attributable to any marker is the hazard ratio (HR), which is the increase in risk for one standard deviation increase in that marker. If non-HDL-C is a more accurate marker of cardiovascular risk than LDL-C, the HR for non-HDL-C must be greater than the HR for LDL-C. If the cholesterol in VLDL is the reason for this difference, then the HR of VLDL-C must be greater than the HR of LDL-C. Indeed, the HR VLDL-C must be greater than the HR of non-HDL-C.
The conclusion that follows from this elementary mathematics is that the cholesterol in VLDL poses a greater risk than the cholesterol in LDL. This seems highly improbable since LDL particles are so much smaller than VLDL particles and there are nine times more LDL particles than VLDL particles. Moreover, if this were actually true, based on the same elementary mathematics, it is easy to show that as VLDL-C gets less and less, it gets more and more dangerous.208 If the answer, which seems so obvious, is wrong, what is the right answer?
Non-HDL-C is a Better Marker of Cardiovascular Risk than LDL-C Because it is an Indirect Way of Measuring LDL Particle Number
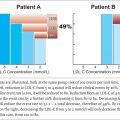
Let us start with what happens when VLDL particles interact with LDL particles in the presence of cholesterol ester transfer protein (CETP) as illustrated in Figure 1.12 and Figure 5.2 . CETP promotes the exchange of the core lipids – cholesterol esters and triglyceride – between VLDL and LDL with the result that cholesterol ester is transferred in net amounts from LDL to VLDL and triglyceride from VLDL to LDL. The transfer of the cholesterol ester from LDL to VLDL produces the cholesterol-depleted LDL particle and because the LDL particle is cholesterol depleted, LDL-C underestimates the number of LDL particles. On the other hand, the cholesterol that has been removed from LDL particles reappears within the VLDL particles, thus increasing the VLDL-C. Accordingly as illustrated in Figure 5.2 , non-HDL-C before the transfer is the same, at least hypothetically, as the non-HDL-C after the transfer because the lower LDL-C after transfer is balanced by the higher VLDL-C after transfer. This means that non-HDL-C restores the relation between LDL-C and LDL particle number and that the increase in non-HDL-C due to the transfer of cholesterol ester from LDL to VLDL restores the total relation of cholesterol within the apoB particles to the number of LDL particles.


FIGURE 5.2
Once this is grasped, it is not surprising that the correlation between non-HDL-C and apoB is significantly greater than the correlation between LDL-C and apoB and even more tellingly, the correlation between non-HDL-C and LDL particle number is greater than the correlation between LDL-C and LDL particle number. The bottom line, therefore, is that the reason that non-HDL-C is a more accurate marker of risk than LDL-C is that non-HDL-C is, in fact, just a backwards and indirect way of measuring LDL particle number. Accordingly, the superiority of non-HDL-C over LDL-C in no way supports the argument that lowering VLDL-C will produce clinical benefit. This may be so, but it has yet to be shown, and it needs to be shown before acting as if it were true.
5.2.3 ApoB
Total plasma apoB includes all the apoB particles, such as the VLDL and IDL particles and the Lp(a) particles as well as the LDL particles (see Figure 5.1 ). With few exceptions, there are 9 times more LDL than VLDL apoB particles and the two exceptions can be recognized. These are remnant lipoprotein disorder and when plasma triglycerides are > 3.0 mmol/l.88,209 Thus, in the vast majority of individuals, plasma apoB is determined by LDL apoB. LDL apoB can be measured directly but this requires isolation of the LDL from plasma by ultracentrifugation and therefore is not clinically practical. However, LDL apoB can be calculated from total cholesterol, HDL-C and triglyceride so long as plasma triglycerides are <3.0 mmol/l.204 Given there is no evidence we are aware of that total apoB is a significantly stronger predictor of risk than LDL apoB, therefore, we believe that plasma apoB is acting as a surrogate for LDL apoB.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree