Anterior Flap Hemipelvectomy
Martin M. Malawer
James C. Wittig
BACKGROUND
The anterior flap hemipelvectomy is a modified version of the classic posterior flap hemipelvectomy. Instead of using the traditional posterior skin flap of the gluteal region, a myocutaneous flap from the anterior thigh is used to close the peritoneum after amputation through the sacroiliac joint and the pubic symphysis. This modification has permitted the treatment of difficult buttock and pelvic tumors where the posterior flap was involved or contaminated by tumor.
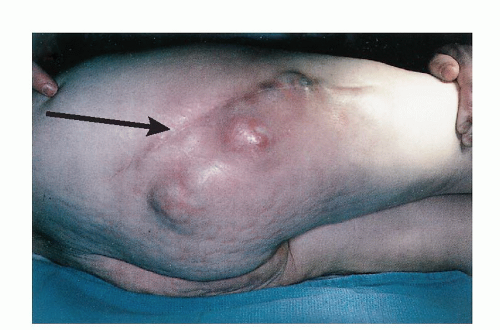
Patients with extensive soft tissue sarcomas of the buttock or bone sarcomas of the pelvis that extend posteriorly, once thought to be incurable by standard posterior flap hemipelvectomy, can often be treated with an anterior flap hemipelvectomy.
The procedure, which originally entailed use of an anterior skin flap raised off a portion of the superficial femoral vessels,1 was modified to include a full-thickness myocutaneous flap raised from the anterior thigh.2,7
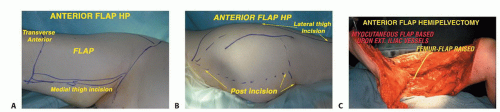
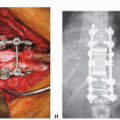
The major advantage of anterior flap hemipelvectomy is the creation of a large vascularized myocutaneous flap that is ideal for closure of significant posterior defects (FIG 1). As much of the anterior thigh compartment may be saved as needed, depending on the size of the defect being closed. As always, careful patient selection is critical in ensuring that an acceptable outcome is achieved. For example, elderly patients and diabetics with silent atherosclerotic disease of femoral vessels must be carefully evaluated with preoperative angiography.
The hemipelvectomy procedures described in the previous chapter require a flap of buttock skin to cover the surgical defect. Anterior flap hemipelvectomy allows sacrifice of the entire buttock and all the overlying skin and soft tissue to the midline. Even patients who have a tumor-contaminated buttock to the midline may have a potentially curative procedure.11,12
If possible, tumors in this area, especially those of low histologic grade, should be treated with an excision of the gluteus maximus muscle (buttockectomy). However, if tumor extends through the gluteus maximus muscle to involve the gluteus medius or minimus, if tumor encases the sciatic nerve, or if tumor is directly adjacent to the pelvic bones, a radical amputation using an anterior myocutaneous flap is indicated.
ANATOMY
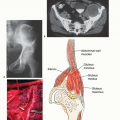
The surgeon must be familiar with the pelvic anatomy as well as the thigh musculature and femoral vessels. The anatomic key to this procedure is the major vascular pedicle of the pelvis and extremity. Oncologic considerations for tumor involvement of the bone or soft tissues in the pelvis are identical to those discussed in the chapter on posterior flap hemipelvectomy.
The external iliac vessels leave the pelvis and cross through the femoral triangle where they become the common femoral vessels. A single branch supplying the iliac crest may be encountered along the medial aspect of the external iliac vessel just below the inguinal ligament. The superficial femoral vessels travel underneath the sartorius muscle along most of the length of the thigh; they pass through the adductor hiatus and become the popliteal vessels behind the knee. The major branch in the femoral triangle is the profunda femoris, which arises from the posterior aspect of the superficial femoral vessel and passes deep to the posterior surface of the femur. Ligation of the profunda femoris is required to elevate the anterior flap. The common femoral and superficial femoral vessels are preserved.
The (four) quadriceps muscles, the adductor muscles, and the sartorius muscle all have a vascular supply that arises from pedicles off the superficial femoral artery. Perforating branches from the profundus are present in the vastus lateralis and may be encountered as they pass through the intramuscular septum.
The entire anterior and medial compartments can be elevated off the femur by dividing the quadriceps tendon above the patella and peeling the full-thickness myocutaneous flap off the anterior femoral periosteum.3,4,6 To prevent hemorrhage, care must be taken to properly ligate all perforating vessels, as well as the superficial femoral vessels, at the level of the adductor hiatus.
Division of the skin at the inguinal canal and skeletonization of the external iliac vessels permit the entire flap to be rotated as necessary to cover the defect created by the amputation.
Use of this flap for closure results in improved cosmesis and facilitates fitting of a prosthesis for an improved functional result.9,10,11 In addition, this flap permits radiation therapy to the remaining pelvis without any wound complications. The nature of the flap available for closure permits greater posterior resection than that possible during a traditional posterior flap hemipelvectomy.
The entire buttock compartment (ie, the gluteal muscles, sciatic nerve, sacrospinous ligaments, and sacral alar) can be safely removed.
The anterior myocutaneous flap consists of a portion of or the entire quadriceps muscle group on its vascular pedicle, the superficial femoral artery.4 This flap covers the entire peritoneal surface and generally heals with minimal problems.
IMAGING AND OTHER STAGING STUDIES
In addition to the routine radiographic evaluation of the pelvis (radiography, computed tomography [CT] and magnetic resonance imaging [MRI], and bone scanning) necessary
to determine the patient’s suitability for a hemipelvectomy, angiography of the femoral vessels is essential for patients undergoing anterior flap hemipelvectomy.
The variable nature of the profunda femoris, as well as the frequent presence of silent atherosclerosis of the superficial femoral artery in elderly patients or in patients with a history of smoking, can greatly affect the outcome of this procedure. In addition, visualization of the pelvic vessels can help to ensure that they are not involved with the tumor.
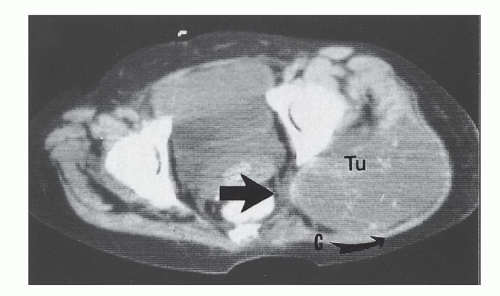
CT and MRI are required to determine whether the tumor involves the sacrum or the vertebra. Spinal involvement is a contraindication to this procedure (FIG 2).
INDICATIONS
Anterior flap hemipelvectomy is indicated for tumors involving the buttock that cannot be resected with a less radical procedure. Patients who have failed to respond to prior attempts at limb-sparing surgery, with or without radiation, or who have tumors that primarily involve the posterior thigh and sciatic nerve are also candidates for this procedure.
This procedure may also be indicated after failed attempts at limb-sparing surgery5 as well as for patients with nononcologic indications for amputation8 (eg, uncontrollable sepsis from sacral or trochanteric osteomyelitis).
Nononcologic indications include selected paraplegics with uncontrollable chronic osteomyelitis of the pelvis or hip joint.
SURGICAL MANAGEMENT
Preoperative Planning
Careful presurgical planning is necessary to achieve optimal results. The planned surgical incision is drawn before any cutting to visualize the separate components of the anterior flap hemipelvectomy incisions (FIG 3).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree