The prostate is composed of tuboalveolar glands surrounded by fibromuscular stroma. This stroma is composed of collagen and smooth muscle fibres that contract during ejaculation to express prostatic secretions into the urethra [2].
Prostatic Capsule
The so-called prostatic capsule is a condensed layer of fibromuscular tissue that encloses most of the external surface and determines the outer limits of the prostate. This structure is an important landmark in the pathological staging of prostate cancer, determining if the disease is still organ-confined. The capsule cannot be distinguished on the anterior aspect of the prostate, where the anterior fibromuscular stroma and detrusor apron are found. Moreover the capsule is absent at the apex and the base of the gland, where the prostate stroma blends with the muscle fibres of the urinary sphincter and detrusor muscle respectively [3–5].
Several authors have questioned the term “prostatic capsule” since the fibromuscular band is not a real anatomic capsule in the true sense of the word: first because it is incomplete at the apex and base, second because the fibromuscular band shows great homogeneity with the muscle content and muscle density of the prostatic stroma. Therefore is considered an extension of the parenchyma itself, rather than a distinct structure (Fig. 2) [3, 4, 6].
Fig. 2
Periprostatic fasciae. Axial section of prostate and periprostatic fascias at midprostate: (a) anatomic (reproduced with permission from the Mayo Foundation for Medical Education and Research). (b) schematic. AFS anterior fibromuscular stroma, C capsule of prostate, DA detrusor apron, DVC dorsal vascular complex, ED ejaculatory ducts, FTAP fascial tendinous arch of pelvis, LA levator ani muscle, LAF levator ani fascia, NVB neurovascular bundle, PB pubic bone, PEF parietal endopelvic fascia, PF prostatic fascia, pPF/SVF posterior prostatic fascia/seminal vesicles fascia (Denonvilliers’ fascia), PZ peripheral zone, R rectum, TZ transition zone, U urethra, VEF visceral endopelvic fascia. Reprinted [6] with permission
Zonal Anatomy of the Prostate
In 1968 McNeal introduced the concept that the glandular elements of the prostate can be divided into discrete regions or zones, each of which arises from a different part of the prostatic urethra (Fig. 3) [7]. Every zone has its specific architectural and stromal features and specific pathological lesions. The different glandular zones of the prostate can usually be visualised by transrectal ultrasound (Fig. 4) [2].
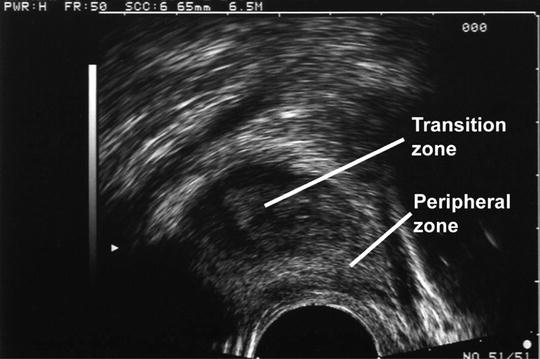
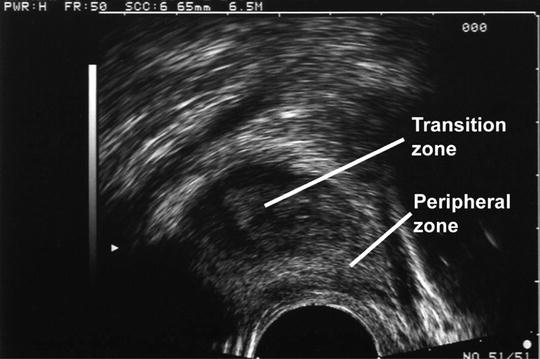
Fig. 4
Ultra sound image. Sagital view of the prostate
Peripheral Zone
The peripheral zone comprises the bulk of the glandular tissue (70 %) at the lateral and posterolateral side of the gland. Its ducts drain into the posterolateral recesses of the urethral wall as a double row extending from the base of the verumontanum to the prostate apex (Figs. 2–4) [2, 7].
This zone is most susceptible region for (chronic) prostatitis. Moreover, it is the site of origin of 70 % of prostatic carcinomas.
Central Zone
The central zone accounts for about 25 % of the volume of the prostate gland. Its ducts arise from a small focus around the ejaculatory duct orifices. These ducts branch directly towards the base of the prostate as a cone around the ejaculatory ducts (Fig. 3). The base of the cone comprises almost the entire base of the prostate. The central zone is quite resistant to inflammation and carcinogenesis. Only 1–5 % of prostate cancers have their origin in this zone, although cancers from adjacent zones may infiltrate it more frequently [2, 7].
Transition Zone
The glandular tissue of the transition zone constitutes only 5–10 % of the prostate gland in early adulthood, but comprises an increasing portion of the gland in ageing men that develop benign prostatic hyperplasia (BPH). The ducts arise at a single point just proximal to the urethral angle that divides the proximal and distal prostatic urethra. The ducts then pass laterally, around the distal border of the preprostatic sphincter, a sleeve of smooth muscle surrounding the proximal prostatic urethra, to travel on its lateral and posterior sides as two independent small lobes (Figs. 2 and 4). A discrete layer of fibromuscular tissue separates the transition zone from the remaining glandular zones, facilitating its visualisation by transrectal ultrasound. The transition zone is the site of origin of BPH and about 20 % of prostate adenocarcinomas arise in the zone [2, 7].
Anterior Fibromuscular Stroma
The anterior fibromuscular stroma is a non-glandular region on the anteromedial aspect of the prostate from the bladder base to the apex, where the stroma blends with the external urethral sphincter. Its lateral margins are continuous with the prostatic capsule (Fig. 5). It is composed of elastin, collagen and smooth muscle, although considerable portions of it may be replaced by glandular tissue in BPH. This zone is very rarely affected by prostate cancer [2, 7].
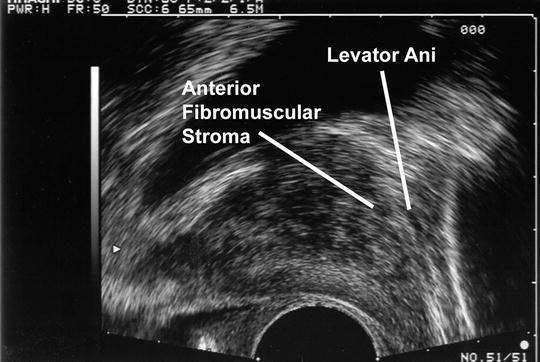
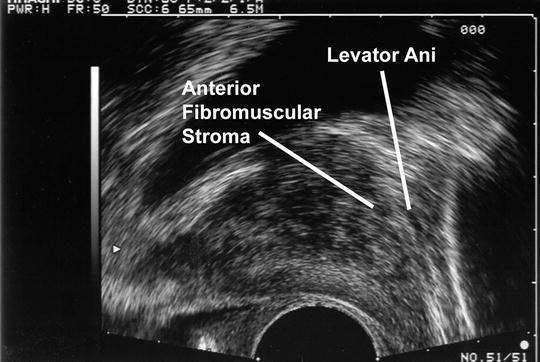
Fig. 5
Ultrasound image. Sagital view
Seminal Vesicles
The seminal vesicles (SVs) are coiled sacculated tubes of approximately 5 cm long. The tubes are lined by a columnar epithelium and enclosed by a thin layer of smooth muscle. The vesicles lay extraperitoneally at the bladder base, lateral to the termination of the vasa. Each vesicle joins its corresponding vas deferens to form the ejaculatory duct, which transverses the posterior prostate to drain into the verumontanum (Figs. 2 and 6) [2].
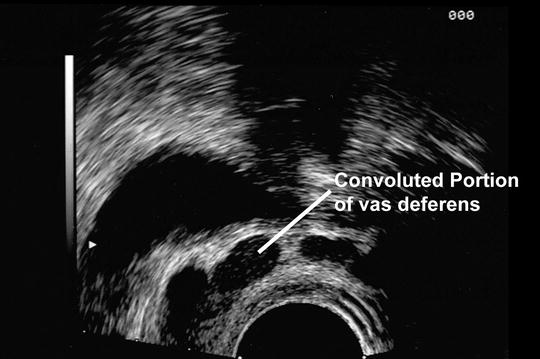
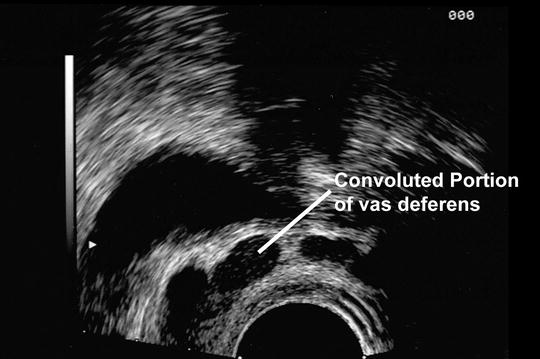
Fig. 6
Ultrasound image using 7.5 MHz probe
The SVs cannot be palpated on digital rectal exam, unless involved by a pathologic process, e.g. invasion of prostate cancer. Seminal vesicle invasion is universally accepted as an adverse prognostic factor. Since SV can be invaded by prostate cancer, standard radical prostatectomy includes “en bloc” resection of the prostate and the SVs. Some recent publications advocated SV-sparing radical prostatectomy for low risk localised prostate cancer, to avoid injury to the pelvic autonomous nerves and improve post-operative recovery of potency and continence [8, 9]. The anatomical evidence for this approach however is unclear: we demonstrated that the nerves surrounding the SVs are mainly sympathetic nerves responsible for ejaculation, rather than parasympathetic cavernous nervous. In our view, seminal vesicle-sparing surgery remains experimental with the potential risk of incomplete oncological resection.
Anatomy of the Pelvic Floor
The male pelvic floor is a complex structure consisting of muscles, fasciae and ligaments that support the visceral organs. It is traversed by the urethra and the rectum and has connections to the bony pelvis, the pelvic organs and the extensive fibro-elastic network in the fat-containing anatomical spaces. Distinct anatomical units of the pelvic floor functionally cooperate to maintain continence and to facilitate micturition and defecation [6, 10].
This chapter specifically focuses on the role of the pelvic floor in urinary (patho)physiology, for its role in faecal continence mechanisms readers are referred to the literature [10].
Levator Ani Muscle
The levator ani is the largest muscle of the pelvic floor, consisting of different parts (the pubovisceralis, iliococcygeus and pubococcygeus muscles) that originate at the pubic bone, the tendinous arc of the levator ani muscle and the spine of the ischium and sweep down in a series of loops.
The levator urethrae or levator prostatae muscle constitutes the anteromedial aspect of the pubovisceralis muscle (Fig. 5). It originates at the posterior side of the pubic bone and forms a loop around the prostatourethral junction to insert into the perineal body, between the urethra and the anal sphincter. The puborectalis muscle constitutes the main part of the pubovisceralis muscle. It sweeps around the anorectal junction, where it constitutes part of the anal sphincter (for an excellent review see [10]). Contraction of the pubovisceralis muscle lifts and compresses the urethra to stop urine outflow from the bladder. These muscle fibres play an important role in active maintenance of urinary continence. As such it is important to recognise and preserve these muscles during apical prostate dissection [6, 11].
The iliococcygeus and pubococcygeus muscles arise from the pelvic wall and insert into the last two segments of the coccyx and the anococcygeal raphe [10].
Urinary Sphincter
For an excellent review of the anatomical history and current concepts about the urethral sphincter complex, we strongly recommend the review by Dr. M. Koraitim [12].
The male urethral sphincter complex consists of two functional components: an involuntary inner urethral sphincter (IUS) composed of urethral smooth muscle fibres and a voluntary external urethral sphincter (EUS) composed of striated muscle. This sphincter complex surrounds the urethra from the vesical orifice to the distal end of the membranous urethra. Importantly, the urinary sphincter is solely composed of urethral smooth muscle. Bladder smooth muscle fibres do not contribute to the urinary sphincter mechanism.
Inner Urethral Sphincter
The internal urethral sphincter (IUS) also called the lissosphincter, is composed of smooth muscle and elastic connective tissue that completely surround the urethra from the bladder neck to the membranous urethra. The lissosphincter consists of an inner layer of longitudinally oriented fibres surrounded by a wider layer of circular smooth muscle, that is most prominent at the level of the vesical orifice and gets thinner around the proximal urethra (Fig. 7) [11–13].
Fig. 7
Urinary sphincter complex
Functionally, the IUS is responsible for involuntary continence at rest, the so-called passive continence. Involuntary contraction of the circular fibres results in closure of the bladder neck and concentric narrowing of the proximal urethra to provide passive continence. Continence studies after surgery (TURP, prostatectomy [14], urethraplasty [15, 16]) have clearly demonstrated that the full length of the IUS is not mandatory to maintain continence, but there is a crucial minimal length below which incontinence is inevitable. Therefore, careful dissection of the prostatourethral junction and prostatic apex, with maximal preservation of urethral length during radical prostatectomy can contribute to post-operative recovery of urinary continence.
External Urethral Sphincter
The external urethral sphincter (EUS), also called rhabdosphincter consists of striated muscle fibres that largely cover the external side of the IUS. In contrast to the IUS however, the EUS does not completely encircle the urethra, but has an opening on the dorsal side (Fig. 7). In males the EUS has no anatomical connections to the levator urethrae muscle and thus forms a distinct anatomical and functional structure [12, 13].
The rhabdosphincter is most prominent around the membranous urethra and gradually decreases in thickness towards the bladder. The increase in prostate size after puberty causes the muscle fibres to partially atrophy and become more dispersed, with intervening smooth muscle fibres. As such, the superior part of the EUS forms a thin cap on the anterolateral side of the prostate, whereas the inferior part forms a horseshoe-shaped muscle around the membranous urethra. At the infraprostatic level, the thickness of the striated muscle is greater on the anterior and anterolateral aspect of the sphincter and gradually gets thinner at the posterolateral side. Posteriorly, the circumference of the rhabdosphincter is interrupted by the fibrous median raphe [12, 13].
The rhabdosphincter provides active continence. Contraction of the horseshoe-shaped muscle compresses and angulates the anterior wall of the urethra against the rigid posterior plate formed by the median raphe, Denonvillier’s fascia and the rectourethralis muscle [12].
The EUS muscle is composed of both slow (type I) and fast twitch (type II) muscle fibres; with the fast twitch fibres predominating in the infraprostatic part. This allows the EUS to contract quickly and forcefully when the intra-abdominal pressure rises. This contraction can however only be maintained for a short period of time (seconds). In contrast, the lissosphincter that provides involuntary, passive continence cannot contract as strongly but is able to maintain its contraction much longer [12, 17, 18].
The prostatic part of the rhabdosphincter does not play a role in maintaining continence but may play a role in semen propulsion by compression of the prostatic urethra [12].
Fasciae of the Male Pelvis
The pelvic fasciae consist of two components: the endopelvic fascia, which primarily covers the pelvic muscles and the visceral fascia, which covers the pelvic organs and the supplying vessels and nerves [4, 6]. Whereas the endopelvic fascia consists of a condensed layer of collagen fibres, the visceral fasciae consist of connective and fatty tissue that form different layers, which are sometimes difficult to recognise anatomically, with many confusing and conflicting descriptions. Nevertheless, understanding of the fascial investments of the prostate, rectum and levator ani is fundamental for the urologist to perform nerve sparing radical prostatectomy. Various authors have used different terminology to describe the fasciae of the pelvis. In this chapter, we will follow the terminology proposed by Walz et al. in their excellent review of prostate anatomy [6].
The Endopelvic Fascia
The endopelvic fascia is the fascia that covers the pelvic floor. It can be divided in the parietal endopelvic fascia, covering the levator ani muscle, and the visceral endopelvic fascia, covering the anterior side of the bladder, prostate and rectum. This fascial layer is fused with the anterior fibromuscular stroma of the prostate [6, 19]. The visceral and parietal endopelvic fascia coalesce lateral to the bladder and prostate, forming a whitish line, the fascial tendinous arch of the pelvis (FTAP) (Fig. 2). This fascial condensation stretches from the PPL/PVL to the ischial spine. During radical prostatectomy the FTAP needs to be incised to mobilise the prostate. Applying counter traction to the prostate facilitates identification of the fascial reflection between the parietal and visceral endopelvic fascia. This cul-de-sac is easiest to recognise and incise at the base of the prostate, where the space between the levator ani muscle and prostate is larger and the endopelvic fascia is thinner [4, 6, 19].
The Periprostatic Fascia
The term periprostatic fascia (PPF) is used to describe the fascial layers that cover the anterior and lateral surface of the prostate [6]. The PPF does not consist of a single layer of collagenous tissue, but is composed of different layers of connective and dispersed adipose tissue [20]. Importantly, preservation techniques for anatomical dissection often dissolve the adipose tissue, making it hard to recognise these different layers in the dissection room.
The term anterior periprostatic fascia is used for the visceral endopelvic fascia that covers the detrusor apron and dorsal vascular complex on the anterior surface of the prostate (Fig. 2) [6].
The lateral periprostatic fascia enfolds the anterolateral surface of the prostate. It is multilayered and consists of an outer Levator Ani Fascia (LAF) and an inner, usually multilayered Prostatic Fascia (PF) [6]. The layers of the periprostatic fascia form a fascial sheet around the neurovascular bundle on the dorsolateral side of the prostate that is important for the surgeon performing a radical prostatectomy [6, 21, 22]. The PF directly covers the prostatic capsule and fuses with the PPL/PVL and the DVC on the anterior aspect of the prostate. As such the PF runs medial to the NVB. The outer LAF covers the levator ani muscle and runs laterally to the NVB on the dorsolateral aspect of the prostate (Fig. 2). Posteriorly, this fascia continues as the Pararectal Fascia as it separates the levator ani from the rectal wall.
In about half of the patients, the PF and LAF are fused at the anterolateral aspect of the prostate and diverge only at its dorsolateral side, to form a triangular sheet around the NVB, with the medial layer being PF, the lateral layer LAF and the posterior layer Denonvillier’s fascia. In the other half, the PF and LAF are not fused, but separated by a thin layer of areolar tissue. In these patients, the fibres of the NVB are dispersed over the lateral surface of the prostate rather than forming a distinct bundle [20].
The Fascia of Denonvilliers
Denovilliers’s fascia is an important anatomical landmark for urological and colorectal surgeons. This fascia runs almost vertically between the peritoneal reflection of the rectovesical pouch and the pelvic floor, covering the posterior aspect of the prostate (posterior prostatic fascia) and the seminal vesicles (seminal vesicle fascia) (Fig. 2). Histologically it is composed of dense collagen, smooth muscle fibres, and coarse elastic fibres and varies from a fragile thin layer to a dense, single layered membrane [6, 23].
Denovilliers’ fascia separates the prostate from the extraperitoneal rectal wall that is covered by the fatty anterior mesorectum and fascia propria. It is often fused with the prostatic capsule in the midline and is continuous with the central perineal tendon at the prostato-urethral junction. More laterally DF has no significance adherence to the prostatic capsule. It merges laterally with the LAF, herby forming the base of the triangular sheet around the NVB, separating it from the mesorectum. Complete resection of Denonvillier’s fascia can be important in to avoidance of positive surgical margins.
The rectal fascia propria is a thin fascial layer (serosa) that is often incorrectly nominated the posterior layer of Denonvilliers fascia. During total mesorectal excision, the plain of dissection should be between Denonvillier’s fascia and the fascia propria, to obtain an oncological safe resection while avoiding damage to the neurovascular bundle [23–25].
Detrusor Apron and Pubovesical/Puboprostatic Ligaments
For an excellent review of the anatomy and histology of the detrusor apron, see Myers et al. [26]. Several authors have shown that the bladder smooth muscle does not stop at the vesico-prostatic junction but that superficial, longitudinal smooth muscle fibres of the anterior bladder wall fan out distally covering the anterolateral aspect of the prostate, as the so-called detrusor apron (DA) (Fig. 2). These fibres converge in their path towards the apex as two lateral condensations that attach to the posterior surface of the pubic bone as the pubovesical ligaments (PVL). In small prostates, the detrusor apron forms a thick layer on the anterior surface of the prostate and the relation between the anterior bladder wall and PVL is easily appreciated. As the prostate grows however, the DA gradually gets stretched and the distance between the bladder neck and the pubic attachments of the DA increases. In benign prostatic hyperplasia, the fibrous attachments to the pubic bone seem to be connected to the ventral prostate, without continuity to the bladder and were therefore called puboprostatic ligaments (PPL) [4, 19, 26–28].
The PVL/PPL that support the prostate, urethra and anterior bladder neck are thought to be relevant in anterior stabilisation of the sphincter complex. Several approaches have been described to preserve the PVL/PPL during retropubic or laparoscopic radical prostatectomy in an attempt to improve early recovery of urinary continence [29, 30]. Similarly, a so-called anterior suspension suture is used to restore the anterior stabilisation of the urethra to the posterior pelvic bone ([31, 32] Hurtes, #86). Although there is little evidence, an increasing number of papers try to support a role for the PVL/PPL complex in preservation/restoration of urinary continence after radical prostatectomy.
Vesicoprostatic Muscle
Similar to the anterior detrusor apron, the outer longitudinal fibres of the detrusor muscle continue distal to the posterior vesicoprostatic junction, to form the vesicoprostatic muscle. These fibres fan out between the posterior bladder neck and the insertion of the seminal vesicles and the vasa deferentia. Histologically the vesicoprostatic muscle consists of two layers: on anterior layer of longitudinally oriented muscle fibres that are continuous with the outer layer of the detrusor muscle and a posterior layer that consists of fibroadipose tissue that is continuous with the bladder adventitia [33]. During the so-called Rocco-stitch to repair the posterior suspension mechanism of the rhabdosphincter, the remnant of the transected vesicoprostatic muscle is sutured to the posterior median raphe [34].
Periprostatic Neurovascular Anatomy
Blood Supply to the Prostate and SV
Prostate
The introduction of selective arterial embolisation as an alternative treatment for BPH introduced a renewed interest in the arterial anatomy of the prostate. Although this treatment is still experimental, it has lead to a number of new studies that have improved our insights into the vascular anatomy of the prostate. In addition to dissections on human cadaveric specimens, the newer studies use vascular imaging techniques as arteriography and CT angiography to study the prostatic arteries [35–37].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree