Fig. 2.1
Schematic representation of the blood supply to the lips
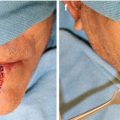
Fig. 2.2
Schematic representation of the cross section of the lower lip demonstrating the relationship of the labial artery to the surface anatomy and musculature
Most commonly, the facial artery also gives rise to a HLA and VLA. The complementary nature of these vessels means a patient with a small HLA will have a larger VLA and vice versa. The VLA ascends in the labiomental region deep to the depressor labii inferioris and occasionally will originate from the submental artery. As it ascends, the VLA splits into branches traveling superficial and deep to the orbicularis oris often anastomosing with the superficial and deep descending branches of the ILA. The HLA originates from the facial artery proximal to the ILA and runs in the labiomental portion of the lip. After branching from the facial artery, it can course horizontally to anastomose with the contralateral HLA, decrease in size until terminating near the midline, or turn to run in a vertical direction [9, 11].
The upper lip blood supply is derived from the superior labial artery (SLA). It originates 10–12 mm laterally from the commissure and is superior to the commissure in 78 % of cases with the remaining 22 % originating at the commissure [11]. The distance to the commissure is important in the consideration of the amount of tissue to be preserved in rotation of axial pattern flaps in this area. The mean diameter of the SLA after branching is 1.8 mm and is a single vessel in all cases [11]. Similar to the lower lip ILA, the SLA travels at the level of the vermillion-cutaneous junction between orbicularis oris and mucosa and forms an anastomosis at the midline with the contralateral SLA. In its course, the SLA gives off superficial and deep ascending branches in a fashion similar to the lower lip. These branches send small vessels to the vermillion before traveling superiorly to anastomose with the vascular plexus at the base of the nose, columella, and nasal tip [7, 10, 11].
The venous drainage of the lips is less well defined and is difficult to identify. Vena comitantes are commonly considered as the main venous drainage system of the lips. Superior and inferior labial veins have also been described, both of which drain into the ipsilateral facial vein. As can be seen, the vascular supply of the lips is complex however the major supply of both the upper and lower lip is fairly consistent in location with numerous anastomoses providing collateral flow.
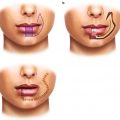
2.4 Lymphatic Anatomy
The lymphatic anatomy of the upper and lower lip should be considered separately due to varied drainage patterns arising from the embryologic development of the lips. The upper lip is less likely to drain to contralateral nodal basins due to the fusion of a central medial nasal process with the paired lateral nasal processes. This midline process separating the paired lateral processes makes contralateral neck disease a rare finding. In contrast, the lower lip is formed by fusion of two mandibular processes and contains numerous interconnecting lymphatics across the midline, increasing the chance of bilateral or contralateral drainage patterns [12] (Fig. 2.3).