- 4.1 Introduction
- 4.2 Immediate (type I) hypersensitivity
- 4.3 Atopy
- 4.4 Anaphylaxis
- 4.4.1 Anaphylaxis
- 4.4.2 Anaphylactoid reactions
- 4.4.1 Anaphylaxis
- 4.5 Allergic conjunctivitis
- 4.5.1 Seasonal (hay fever) and perennial (vernal) conjunctivitis
- 4.6 Respiratory allergy
- 4.6.1 Allergic rhinitis
- 4.6.2 Asthma
- 4.6.1 Allergic rhinitis
- 4.7 Food allergy and intolerance
- 4.7.1 Food allergy and intolerance
- 4.7.2 Diagnosis of food allergy and intolerance
- 4.7.1 Food allergy and intolerance
- 4.8 Skin diseases
- 4.8.1 Urticaria and angioedema
- 4.8.2 Atopic eczema
- 4.8.3 Contact dermatitis
- 4.8.1 Urticaria and angioedema
 Visit the companion website at www.immunologyclinic.com to download cases with additional figures on these topics.
Visit the companion website at www.immunologyclinic.com to download cases with additional figures on these topics.
4.1 Introduction
‘Allergy’ is a much-misunderstood term that is used wrongly in general parlance. Unfortunately, the term is often used loosely to describe any intolerance of environmental factors irrespective of any objective evidence of immunological reactivity to an identified antigen. In this chapter, we distinguish those conditions in which immunological reactivity to key antigens is well defined from the rest, since such patients often present to an allergy clinic because of a popular public perception that they are ‘allergic’ in origin. In order to avoid any confusion the relationship of these terms is shown in Box 4.1.
Truly allergic diseases are common: about 20% of the population experience some form of allergy and this imposes a substantial physical and economic burden on the individual and society. Some patients have an occasional mild allergic reaction, some suffer life-long debilitating disease, while, more rarely, some react with severe or fatal anaphylactic shock. The prevalence of allergic diseases is increasing. Although not all diagnoses of ‘asthma’ may be truly immunological (wheeze induced by common childhood viral infections, bronchiolitis in infants), in the USA, UK and many European countries the prevalence of asthma diagnosed in children has risen at a rate of about 5% per year. Multiple factors contribute to the overall risk of developing allergy (Box 4.2), but the decline in family size and a reduced microbial burden during childhood in many countries – the hygiene hypothesis – may partly account for the rising prevalence.
- Atopy
- Age – commoner in children than adults
- Gender – commoner in boys than girls
- Family size – less common in large families
- Reduced microbial burden in developed countries (hygiene hypothesis)
- Smoking – active or passive
- High levels of antigen exposure
- Dietary factors – poor intrauterine nutrition
Allergic reactions to antigens that enter the systemic circulation, through an insect sting or intravenous administration of an antibiotic, can produce life-threatening anaphylactic reactions. More commonly, antigens are inhaled or ingested, trigger more local reactions in the upper or lower respiratory tracts (rhinitis or asthma) or in the mouth or upper gastrointestinal tract. However, some ingested (peanut) or inhaled (latex particles) antigens can cause anaphylaxis, a severe systemic reaction.
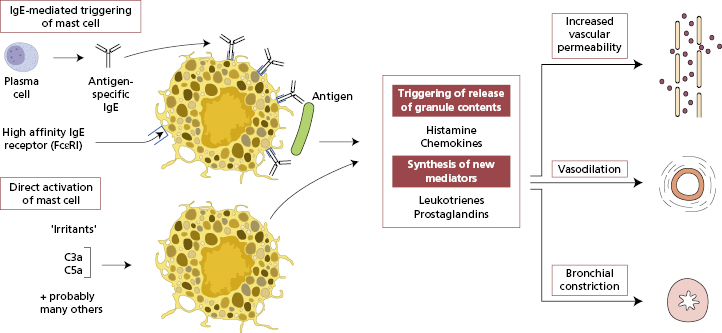
4.2 Immediate (type I) hypersensitivity
Recognition of antigen by antibodies and cellular receptors can cause incidental tissue damage as well as the intended destruction of the antigen. Such reactions are called hypersensitivity reactions (section 1.6) and the term allergy is synonymous with immediate (type I) hypersensitivity, since IgE-mediated reactions are occur within a few minutes of the second antigen exposure. Antigen-specific IgE plays a key role being synthesized on first exposure and causing allergy only on subsequent exposures. IgE is only a trace component of normal serum as it is bound, via its Fc regions, to the high-affinity FcΣRI receptor on mast cells (Fig. 4.1). Antigen reacts with surface-bound IgE causing cross-linking of receptors, an influx of calcium ions into the cell and explosive degranulation with release of preformed mediators (Fig. 4.1): these mediators include histamine, heparin, lysosomal enzymes and proteases, and several chemoattractant cytokines (chemokines) such as interleukin-(IL)-8 and RANTES (Table 1.6). Other mediators are newly generated and derived from the metabolism of arachidonic acid via two enzyme pathways: one leads to production of prostaglandins and thromboxane, the other to formation of leukotrienes. Histamine is a dominant mediator in the upper airways and leukotrienes in the lower airways disease.
Type I hypersensitivity reactions are rapid; for example, if the antigen is injected into the skin (a skinprick test), immediate hypersensitivity can be seen within 5–10 min as a ‘weal-and-flare’ response, provided the individual has been exposed previously. IgE-mediated reactions are more commonly directed against antigens which enter at epithelial surfaces – inhaled or ingested antigens – so most allergic reactions occur via mast cells in the upper and lower airways or the gastrointestinal tract. Within the upper airways, this is associated with nasal itch, sneeze and rhinorrhoea, which are neurally mediated, as well as nasal obstruction, which is vascular in origin. In the lower airways, mediator release is associated with bronchoconstriction and mucus hypersecretion, giving rise to symptoms of wheeze, breathlessness, chest tightness and cough. Where allergen exposure is persistent, there is also tissue accumulation of neutrophils and eosinophils. Release of mediators from eosinophils and from activated epithelial cells contributes to symptoms (see section 4.6.2). Reactions to insect venom or drugs cause immediate and systemic symptoms via this mechanism too, presumably with small antigens being transported to sensitized mast cells in vital sites such as the larynx.
Exposure of allergic patients to antigen challenge may trigger both ‘immediate’ and ‘late’ phases of bronchoconstriction. This late-phase response (LPR) starts 4–6 h after exposure and can last 24 h. The LPR is characterized by accumulation of activated inflammatory cells, including eosinophils and T lymphocytes. Two mechanisms are involved: in one, the LPR is primarily an IgE- and mast cell-dependent reaction, with newly synthesized mediators attracting the cellular infiltration; in the other, it is mainly mediated by IL-4 released by CD4+ T lymphocytes. These mechanisms are not mutually exclusive.
Not all rapid clinical features resulting from mast cell degranulation necessarily involve IgE-mediated sensitivity. Direct activation of mast cells, known as anaphylactoid reactions, result in release of histamine or other mediators having similar effects (see Fig.4.1). Tartrazine and preservatives that cause asthma or urticaria in sensitive patients (though rarely true anaphylaxis) probably do so by directly triggering basophils or mast cells. Substances that directly activate complement with the production of C3a and C5a also cause immediate reactions, since C3a and C5a are anaphylatoxins that release histamine from mast cells.
4.3 Atopy
Allergic diseases tend to run in families. Atopy defines a state of disordered immunity in which Th2 lymphocytes drive an inherited tendency for hyperproduction of IgE antibodies to common environmental allergens. About 80% of atopic individuals have a family history of ‘allergy’, compared with only 20% of the normal population. However, this trait is not absolute as there is only 50% concordance in monozygotic twins, so there are strong environment influences. Atopy is a clinical definition involving one or more of the common IgE-mediated diseases, namely atopic eczema, allergic rhinitis, allergic conjunctivitis and extrinsic asthma.
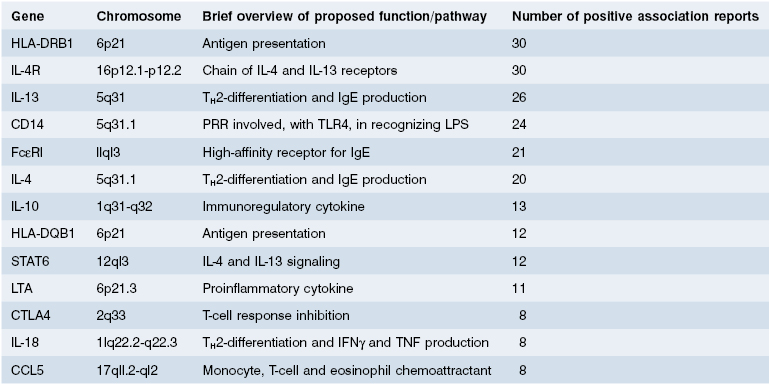
The susceptibility to these atopic disorders is under genetic control, but the evidence suggests that there are many genes with moderate effects (Table 4.1 (a)) rather than one or two major genes. Despite several genome-wide association studies identifying potential new genes, there is as yet no consensus let alone confirmatory functional data. That said, it is clear that total serum IgE levels, production of antigen-specific IgE and bronchial hyper-reactivity are all under some degree of genetic control, accounting for family clustering. Genes on chromosome 5 (the IL-4 gene cluster) are implicated in the regulation of IgE production and genes on chromosome 11q to the atopic phenotype. Inheritance of the HLA-DR3 haplotype is linked to the development of allergy to rye grass, implicating the role of MHC in presenting the particular epitope.
Table 4.1 (a) Some of the candidate genes implicated in development of atopy, asthma and atopic dermatitis
| Chromosome | Candidate gene |
|---|---|
| 5q | TH2 cytokine cluster (IL-3, IL-4, IL-5, IL-13 and GM-CSF) |
| 11q | High-affinity IgE receptor β-subunit |
| 16q | IL-4 receptor α-subunit |
| 17q | RANTES |
| 3q | CD80/CD86 |
| 20p | ADAM 33 metalloproteinase |
Listed in order of likely significance but this will almost certainly change – compare with Table 4.1(b)
Although genetic susceptibility to allergic disease is clearly important, environmental risk factors must play a significant role (see Box 4.2). The epidemiological observation that allergic sensitization is less common in children with older siblings and in those with early exposure to animals or brought up on farms has given rise to the ‘hygiene hypothesis’, which argues that different patterns of microbial exposure may render the immune system of children brought up in urban areas more prone to produce allergic responses. This appears to be due to a polarization of T cells towards a Th2, rather than a Th1, cytokine profile, so posing a greater risk of allergic disease. However, advances in understanding of T cell biology have revealed important roles for other T-cell populations, indicating the Th1/Th2 paradigm oversimplifies the complex mechanisms involved and that T-regulatory cells have been identified as critical players in maintaining tolerance to environmental antigens and Th17 in persistence of inflammation involved in asthma.
4.4 Anaphylaxis
4.4.1 Anaphylaxis
Systemic anaphylaxis is the most dramatic example of an immediate hypersensitivity reaction. Clinically, the term refers to the sudden, generalized cardiovascular collapse or bronchospasm (Table 4.2) that occurs when a patient reacts to a substance to which he or she is exquisitely sensitive (Box 4.2). Generalized degranulation of IgE-sensitized mast cells or basophils follows antigen exposure and previous sensitization is therefore required. While anaphylaxis is uncommon, it is extremely dangerous, as it is so unexpected, and can be fatal.
Table 4.2 Clinical features of anaphylaxis
| Organ | Feature |
|---|---|
| Cardiovascular system | Vascular collapse |
| Respiratory system | Bronchospasm |
| Laryngeal oedema | |
| Skin | Erythema |
| Angioedema | |
| Urticaria | |
| Gastrointestinal system | Vomiting |
| Diarrhoea |
When antigen is introduced systemically, as in a wasp sting or intravenous antibiotic, cardiovascular collapse is the predominant clinical feature. When antigen is absorbed through the skin or mucosa, as in latex rubber anaphylaxis, the reaction develops slightly more slowly (see Case 4.2). Allergy to latex rubber is increasingly common: several high-risk groups are recognized (Table 4.3) and latex allergy may cross-react with certain foods (Table 4.3). Foods that are absorbed via the oral mucosa seem especially likely to trigger angioedema of the lips, tongue and larynx. In some cases, hypotension and collapse may occur during or after exercise if certain foods are eaten immediately before the exertion – food-related, exercise-induced anaphylaxis.
Table 4.3 Key features of latex rubber allergy
High-risk groups
Operating theatre staff Females Atopics
|
High-risk latex products
|
Cross-reactivity with food allergies
|
Anaphylaxis can also occur in those allergic to a particular drug, such as penicillin. Penicillin allergy is commonly self-reported, but true anaphylactic reactions are much rarer, with a rate of 25 per 100 000 treated patients. The risk of a severe reaction is greater following parenteral than oral penicillin, and over six times more likely in a patient with previous reactions to penicillin. However, most serious reactions occur in patients with no previous history of penicillin allergy. Skin-prick testing using major and minor penicilloyl determinants is of limited value, since up to 90% of skin-test-positive patients subsequently tolerate penicillin. On the other hand, a negative skin-prick test usually indicates patients who are not at risk or in whom reactions will be mild.
The only laboratory test that is useful at the time of an apparent anaphylactic reaction is blood mast cell tryptase. This is an indicator of mast cell degranulation, but an elevated level identifies neither the mechanism of mast cell activation nor its cause. Antigen-specific IgE (RAST) tests are helpful to confirm the nature of the insect venom prior to desensitization but skin testing is more useful for latex rubber.
As in Cases 4.1 and 4.2, intramuscular epinephrine (adrenaline) is the most important drug in treating anaphylaxis and is nearly always effective. It should be followed by parenteral administration of hydrocortisone and chlorpheniramine. Epinephrine (adrenaline) by inhalation is much less effective. A note of caution: a detailed history is vital in distinguishing anaphylaxis from idiopathic angioedema and urticaria (section 4.8.1), with which it is often confused. While injection of epinephrine (adrenaline) can be lifesaving in anaphylaxis, it can be harmful, even fatal, in elderly arteriosclerotic patients with urticaria and angioedema.
 Case 4.1 Wasp venom anaphylaxis
Case 4.1 Wasp venom anaphylaxisA 69-year-old woman was fit and well until one August when she was stung on the back of her right hand by a wasp. She had previously been stung on several occasions, the last time 2 weeks earlier. Within 5 min, she felt faint, followed shortly by a pounding sensation in her head and tightness of her chest. She collapsed and lost consciousness and, according to her husband, became grey and made gasping sounds. After 2–3 min, she regained awareness but lost consciousness immediately when her husband and a friend tried misguidedly to help her to her feet. Fortunately, a doctor neighbour arrived in time to prevent her being propped up in a chair: he laid her flat, administered intramuscular epinephrine (adrenaline) and intravenous antihistamines and ordered a paramedic ambulance. She had recovered fully by the next day.
She had clinical wasp venom anaphylaxis. Her total serum IgE was 147 IU/ml (NR <120 IU/ml). Her antigen-specific IgE antibody level to wasp venom was 21 U/ml [radioallergosorbent test (RAST) class 4], but that to bee venom was 0.3 U/ml (RAST class 0). The patient was a candidate for specific allergen injection immunotherapy (hyposensitization). The slight but definite risk of desensitization was explained and balanced against the major risk of anaphylaxis should she be stung again. The first injection consisted of 0.1 ml of 0.0001 µg/ml of wasp venom vaccine given subcutaneously. No reaction occurred. Over the next 12 weeks, gradually increasing doses were given without adverse effects. Over this period, she tolerated injections of 100 µg venom. She then continued on a maintenance regimen of 100 µg of venom per month for 3 years.
At the age of 76 years, she was stung by a wasp that had come into her bathroom. She remained calm, lay down and experienced no significant systemic reaction.
 Case 4.2 Latex-induced anaphylaxis
Case 4.2 Latex-induced anaphylaxisA 38-year-old woman was referred for investigation following an anaphylactic reaction whilst visiting a relative in hospital. She gave a 5-year history of recurrent conjunctival oedema and rhinitis when blowing up balloons for her children’s birthday parties. In the year prior to admission, three successive visits to her dentist triggered marked angioedema of her face on the side opposite to that requiring dental treatment. The swellings took 48 h to subside.
On the day of admission, she visited a critically ill relative in hospital. The patient was being reverse barrier nursed and visitors were required to wear gown and gloves. About 20 min after putting on the gloves her face and eyes became swollen, she felt wheezy and developed a pounding heart beat and light-headedness. Her tongue started to swell and she was taken to the Emergency Department where she was given intramuscular epinephrine (adrenaline) and intravenous hydrocortisone (inappropriately as it transpired). She recovered rapidly but was kept under observation overnight.
She had no history of atopy or other allergies. Ten years earlier she had undergone a series of operations for ureteric reflux and in the preceding 2 years had received colposcopic laser treatment for cervical intra-epithelial neoplasia (CIN-III).
Skin-prick testing to a crude latex extract produced a very strong reaction and her antigen-specific IgE antibody level to latex was significantly elevated at 57 U/ml (RAST class 5).
The diagnosis was that of latex-induced anaphylaxis. She was advised to avoid contact with all materials containing latex, and warned that she could react to certain foods (see Table 4.3). It was suggested that she wears a medical alert bracelet, in case she required future emergency surgery, and carry a self-injectable form of epinephrine. The diagnosis has important implications for any further dental, surgical or anaesthetic procedures. Hospitals now have written procedures for latex-free surgery for emergency and planned operations.
Long-term management requires detailed advice on avoidance to prevent further attacks. Preloaded epinephrine (adrenaline) syringes are readily available and effective, but patients must receive training on when and how to use them. Wearing a medical alert bracelet alerts paramedic staff and doctors to the possible cause of collapse. Hyposensitization, or specific allergen immunotherapy, is over 90% effective in patients with bee or wasp venom anaphylaxis provided recommended guidelines are followed (Box 4.4). Venom immunotherapy leads to a marked change in cytokine secretion, with a switch from the proallergic Th2 cytokine profile to a Th1 or inducing T-regulatory cells (see Chapter 7).
- Only high-quality standardized allergen extracts may be used
- Administered in hospitals or specialized clinics only
- Medical staff should have appropriate training and experience in immunotherapy
- Epinephrine (adrenaline) should always be immediately available
- Ensure ready access to resuscitative facilities with attendant staff trained in resuscitative techniques
- Patients should be kept under close supervision for 60 min after each injection
4.4.2 Anaphylactoid reactions
Anaphylaxis should be distinguished from anaphylactoid (i.e. anaphylaxis-like) reactions. These are not mediated by IgE antibodies. Similar pharmacological mediators (such as histamine) are responsible for the clinical features but the stimulus for their release differs. Substances inducing anaphylactoid reactions do so by a direct action on mast cells or by alternate pathway complement activation (see Fig. 4.1). Since this is not immunologically specific, the person does not need to have been previously sensitized to the substance. Collapse following intravenous induction agents for anaesthesia may fall into this category, and expert guidance is required for all patients suffering acute shock during anaesthetic induction to exclude genuine IgE-mediated anaphylaxis. Non-steroidal anti-inflammatory drugs (NSAIDs) divert arachidonic acid metabolism towards production of leukotrienes, which are potent inducers of anaphylactoid reactions via their interactions with specific receptors on target tissues.
The emergency treatment of an anaphylactoid reaction is the same as that of anaphylaxis, but the distinction is important in ensuring the appropriateness and interpretation of investigations and in long-term management of the clinical problem (Case 4.3). In anaphylactoid reactions, skin-prick tests and measurements of antigen-specific IgE are of no value: the only test available is in vivo challenge. Management requires avoidance of the offending agent, since specific allergen immunotherapy is of no benefit in non-IgE-mediated reactions.
 Case 4.3 Drug-induced reaction
Case 4.3 Drug-induced reactionA 77-year-old woman was referred from the Accident and Emergency Department, having been admitted overnight because of sudden onset of massive angioedema of her tongue associated with laryngeal stridor. She was treated with intravenous hydrocortisone only. This was her fifth such episode: an anaphylactoid attack 2 months earlier was severe enough for her to be intubated and ventilated on the Intensive Care Unit.
She had no history of previous allergy and no family history of atopy. A drug history revealed that, in addition to oral prednisolone prescribed in the Accident and Emergency Department, she was taking oral furosemide and captopril. Captopril is an angiotensin-converting enzyme (ACE) inhibitor and this group of drugs is known to cause severe episodes of angioedema. Captopril was discontinued and her mild hypertension was managed with alternative medication. The attacks have not recurred.
4.5 Allergic conjunctivitis
4.5.1 Seasonal (hay fever) and perennial (vernal) conjunctivitis
Seasonal conjunctivitis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree