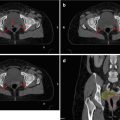
Fig 11.1
Axial MRI image demonstrating the proximal anal canal in a female
11.2 Pathology
More than 80 % of anal SCCs contain one or more subtypes of human papilloma virus (HPV – and usually HPV16 or HPV18). HPV-associated tumours retain wild-type P53, and hence patients with HPV-associated tumours appear to have a good response to concurrent chemoradiotherapy, although most of the evidence has been derived from small retrospective studies (Yhim et al. 2011).
SCCA originates from the transitional and squamous mucosa of the anal canal. Terms such as basaloid, transitional or spheroidal and cloacogenic have largely been replaced by the general term squamous cell carcinoma (SCC), because all have a similar natural history and patterns of spread. The biology and prognosis of keratinising and non-keratinising tumours of the anal canal also appear to be similar. Verrucous carcinomas are another variant and are sometimes described as giant condylomas or Buschke-Lowenstein tumours, which are often enormous exophytic tumours but may have a better prognosis than SCC.
11.2.1 Tumour Grade
Tumours of the anal canal are often defined as poorly differentiated SCC, whereas tumours at the anal margin are well differentiated, but histological grading has been subject to interobserver variability. There is also considerable heterogeneity particularly in larger tumours. Hence, although high-grade tumours are generally accepted to have a worse prognosis, this has not been confirmed in multivariate analysis (Shepherd et al. 1990; Hill et al. 2003).
11.3 Historical Background
Three phase III trials demonstrated that radiotherapy (RT) with concurrent 5FU and mitomycin (MMC) (UKCCCR 1996; Bartelink et al. 1997; Flam et al. 1996) achieves better outcomes in terms of local control and recurrence- or disease-free survival (RFS/DFS) compared to RT alone or RT combined with 5FU alone. In contrast, phase III trials by the Radiotherapy Therapy Oncology Group RTOG 98–11 (Ajani et al. 2008; Gunderson et al. 2012) and the Action Clinique Coordonnees en Cancerologie Digestive ACCORD-03 phase III trial (Peiffert et al. 2012) failed to show benefit for the addition of cisplatin-based neoadjuvant chemotherapy (NACT) prior to CRT in terms of colostomy-free survival (CFS). In the RTOG 9811 trial, the DFS and colostomy rate actually appears inferior with cisplatin (Gunderson et al. 2012). The ACCORD-03 trial also failed to show a benefit in CFS from an increase in the radiotherapy boost dose (Peiffert et al. 2012). Preliminary results of the United Kingdom National Anal Cancer Trial (ACT II) confirm the standard of 5FU/MMC CRT. Results show excellent complete response rates (90 %), with 3-year recurrence-free survival rates overall of 73 % (81 % in T1/T2 tumours, but 64 % for more advanced T3/T4 tumours) (James et al. 2013). The dose and treatment schedule used in the ACT II trial is now the current standard of care in the UK.
11.4 Conventional Radiotherapy Treatment Planning of Anal Cancer
Historically, anal cancer has been treated in all randomised phase III trials with doses of 1.8 Gy per day, using a shrinking-field technique over the course of treatment (UKCCR 1996; Bartelink et al. 1997; Flam et al. 1996; Ajani et al. 2008; Peiffert et al. 2012; James et al. 2013). There have been various previous trial planning techniques. Conventional 2-D large APPA pelvic radiation fields in anal cancer (with generous length and widths of field sizes such that a geometrical miss was extremely unlikely) used the pelvic bones as reference extrapolating the position of the pelvic nodes – based on historical data from studies imaging lymph nodes with lymphangiograms (Davey et al. 1996; Chao and Lin 2002) and early CT scans and from surgical series which defined the sites of pelvic lymph node pathological involvement at laparotomy (Hightower and Judd 1967; Stearns and Quan 1970; Beahrs 1979).
These techniques caused significant acute toxicity of the perineal skin and genitalia; genitourinary, gastrointestinal and haematological toxicity; and poor late function (Ajani et al. 2008; Myerson et al. 2009), often associated with radiotherapy breaks which increase the overall treatment time (OTT), and may compromise efficacy (Allal et al. 1997; Weber et al. 2001; Graf et al. 2003; Huang et al. 2007; Ajani et al. 2008). In April 2012, the National Comprehensive Cancer Network (NCCN) panel agreed that multifield techniques are now preferred over APPA techniques for radiation delivery in anal cancer (Benson et al. 2012). Hence, many institutions are now moving to use multifield techniques, with a range of techniques and different recommended doses.
11.5 Modern Techniques (Intensity-Modulated Radiation Therapy and Volumetric Modulated Arc Therapy)
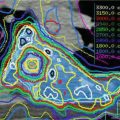
Delivery of radiotherapy in anal cancer is complex because of the heterogeneity in size, the irregular shape of the target volume and the proximity to dose-sensitive critical structures (small bowel, femoral heads, perineum and external genitalia). Intensity-modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT) allow sophisticated dose-painting treatment planning. Comparisons between 3D-CRT, IMRT and VMAT in SCCA demonstrate the same dose coverage in the target but 3D-CRT exposes the surrounding tissue and consequently the OAR to much higher doses (Chen et al. 2005; Stieler et al. 2009).
However, the narrow constraints and high precision of treatment raise concerns about potential geographical misses or compromise of target coverage due to systematic or random radiotherapy errors. Clear definitions of target volumes are therefore essential to ensure accurate and reproducible contouring, treatment planning, delivery and quality assurance. This in turn will require strong engagement with the wider multidisciplinary team including physicists and radiographers to optimise treatment outcome for individual patients.
The International Commission on Radiation Units and Measurements (ICRU) report 83 provides additional recommendations on the selection and delineation of the targets volumes and the organs at risk (ICRU 83 2010).
11.6 Image-Guided Radiotherapy (IGRT)
During a treatment course, individual day-to-day tumour position can be variable. On-line daily imaging can correct both systematic and random errors. Off-line imaging should be interpreted by the radiation oncologist for at least the first 3 fractions and then at weekly intervals to deal with systematic errors. The radiation oncologist can therefore use the on-board imaging system (OBI) or the cone beam CT (CBCT). Verification should use bone landmarks, because soft tissues inferiorly are often blurred.
11.6.1 Anatomy
Knowledge of the location and terminology of lymph node groups in the pelvis is essential for accurate staging in a standardised manner.
11.6.2 The Anal Canal
The anal canal is the most distal part of the large bowel beginning at the anorectal junction. It is approximately 4 cm in length, ending at the anal orifice where the true skin is found at the anal margin. Because the dentate line (which defines the level of the upper limit of the internal sphincter) is the most easily identified landmark in the mucosa of the anal canal, many have suggested that the anal canal is divided into infra-dentate and supra-dentate regions (Wendell-Smith 2000). The components of the anal canal of relevance to surgical disease and treatment are demonstrated on axial (Fig. 11.1), sagittal (Fig. 11.2) and coronal (Fig. 11.3) magnetic resonance imaging (MRI) of the anal canal.
Fig. 11.2
Coronal MRI image demonstrating the anal canal in a female
Fig. 11.3
Sagittal MRI image demonstrating the anal canal in a male
11.6.3 Anal Sphincter
The internal anal sphincter (IAS) is formed by a thickened segment of the circular muscle coat in the distal rectum. From the MRI obtained in the sagittal orientation (Fig. 11.2), the superior aspect of the anal canal can be determined and can usually be defined superiorly by a line joining the tip of the coccyx and the most inferior aspect of the pubis – reflecting the anorectal junction. The ischiorectal fossa, ischial tuberosities and sacrotuberous ligaments lie laterally (best appreciated on MRI obtained in the coronal orientation (Fig. 11.3), the contents of the urogenital triangle anteriorly (Fig. 11.1) and the anal orifice inferiorly (Figs. 11.2 and 11.3)).
11.6.4 Anal Margin
The anal margin is a region of pigmented skin with skin folds surrounding the anus. Although the lateral border of the anal margin has not been defined, anal margin cancer is usually considered as within a radius of approximately 5 cm from the anal orifice.
11.6.5 The Inguinal Nodes
The inguinal nodes are in the inguinal region (superficial inguinal nodes are often larger than nodes from other lymphatic areas) anterior to Scarpa’s femoral triangle and are bounded superiorly by the inguinal ligament, laterally by the medial border of sartorius and medially by the upper border of adductor longus.
From the superficial inguinal nodes, there is an extension to the deep inguinal nodes which are within the fatty tissue of the femoral canal and medial side of the femoral vein. If the superficial nodes are clinically negative, it may be reasonable to avoid treating the deep region.
11.6.6 Femoral Nodes
We have rarely if ever seen involvement of the femoral nodes in anal cancer and do not recommend routine contouring of the femoral nodes.
11.6.7 Presacral Nodes
Presacral nodes are sited around lateral and medial sacral arteries. These lie along the lateral borders of the sacrum and anterior to the sacral pelvic surface usually just medial to the foramen.
11.6.8 Pararectal Nodes
Pararectal nodes lie within the mesorectum usually posteriorly on both left and right sides – probably extending for no more than 4 cm cephalad to the anorectal tumour.
11.6.9 Common Iliac Lymph Nodes
Common iliac lymph nodes are grouped around the common iliac vessel (lateral, intermediate and medial groups).
11.6.10 Internal Iliac Nodes
Internal iliac nodes are sited lateral to the mesorectum and presacral space and are associated with the internal iliac vessels, arising superiorly from the bifurcation of the common iliac artery (at the level of S1) and ending at the level of obturator internus.
11.6.11 External Iliac Nodes
External iliac nodes are usually grouped around the external iliac vessels forming three distinct chains (the lateral, middle and medial groups of external iliac).
Examples of the definitions of the appropriate nodal groups can be found on the ATC website, http://atc.wustl.edu.
11.7 Normal Lymph Node Drainage
Lymphatic drainage depends on the position within the canal. The canal above the dentate line drains to internal pudendal nodes and to the internal iliac system. The canal below the dentate line drains to the medial group of superficial inguinal nodes with further extension to the deep inguinal nodes and some communication superiorly to external iliac nodes and inferiorly with femoral nodes. The upper half of the canal drains mainly by the superior rectal vein to the inferior mesenteric vein and thence potentially to the para-aortic nodes (Hill et al. 2003).
Involvement of regional lymph nodes represents the most common mode of spread from cancer of the anal canal and margin (Kuehn et al. 1968). The perirectal, inguinal, femoral and iliac lymph nodes are the most frequent sites for nodal metastases (Beahrs 1979; Stearns and Quan 1970; Greenall et al. 1985; Gérard et al. 2001). Patients developing inguinal nodal disease invariably do so in the ipsilateral groin (Gérard et al. 2001), unless the tumour is in the midline allowing bilateral nodal recurrence. Nodal involvement is rare if the primary tumour was ≤2 cm in maximum diameter but increased to 35 % when the tumour invaded into adjacent pelvic tissues (Boman et al. 1984). Nodal metastases are also more likely in poorly differentiated cancers (Boman et al. 1984).
11.8 Imaging in Anal Cancer
Available imaging modalities are computerised tomography (CT), magnetic resonance imaging (MRI), endo-anal ultrasound (EUS) and positron emission tomography (PET). Together they allow assessment of the local extent including involvement of other structures and spread to inguinal, pelvic and abdominal nodes and distant sites. Each modality has advantages and limitations, the most crucial being the difficulty in differentiating metastatic from uninvolved reactive nodes of equivalent size.
CT scans are conventionally used to image the pelvis and whole body, but some have recorded that CT failed to reveal an anal primary tumour in 10 of 40 patients, i.e. there were 25 % false negatives (Mistrangelo et al. 2012). MRI scans provide the most detailed anatomy of the primary tumour, the sphincter mechanism and the lymphatic network. MRI is now recommended for locoregional staging of anal cancer in European and NCCN guidelines and is routinely performed in the UK (NCCN 2015 – Benson et al. 2012; Glynne-Jones et al. 2010). A comparison of EUS and MRI (Otto et al. 2009) suggested that EUS may be superior to MRI in detecting small superficial tumours.
Anal cancer is FDG avid even in small tumours (1–2 cm), and PET has a high detection rate of the primary tumour of 90–100 % (Cotter et al. 2006; Nguyen et al. 2008; Winton et al. 2009). Hence positron emission tomography (PET)/CT is gaining ground as an initial staging modality since initial descriptions in 2005 and has been part of NCCN treatment guidelines since 2007.
11.8.1 Criteria for Identifying Involvement of Lymph Nodes
Suspicious perirectal and internal iliac nodes on imaging are rarely biopsied so there is significant risk of false positives. There is no international consensus regarding the normal limit for size in the diagnosis of pelvic and inguinal nodal metastases from pelvic tumours. Size criteria also are different for different histologies and different primary sites (Koh et al. 2006). Authors discussing inguinal node recurrences do not clearly define their CT and MRI criteria to determine uninvolved inguinal lymph nodes (Matthews et al. 2011; Ortholan et al. 2012), nor is this feature clear from any of the randomised trials.
Many use 10 mm as a conventional cut-off. Other criteria such as shape, signal intensity pattern, central necrosis and the degree of contrast enhancement in pelvic nodes are often useful but have not been validated.
11.9 Co-registration for Planning
CT is usually ideal for planning in the pelvis, because it provides anatomical detail with the electron density data essential for dosimetry. It is vital to use contrast with the correct windows and take advantage of multiple orthogonal views (axial, sagittal and coronal) to delineate target volumes (Steenbakkers et al. 2005). It is also advisable to involve your radiologist in person in the planning session. However, contouring the target volume with CT alone is difficult and may provide a major source of errors. A major advantage is that contouring vessels on the CT image can now be used as a surrogate for lymph node localisation and can offer a more precise and individualised elective nodal target delineation compared to that achieved previously.
Advances in the quality of MRI and PET/CT now allow us to determine areas of gross tumour volume more accurately and to delineate tumour and organ boundaries more confidently. The conventional planning CT scan can be co-registered with either diagnostic quality MRI imaging or PET.
11.9.1 MRI
There is little movement within the pelvis, and MRI allows the bone structures of the pelvis to be readily co-registered. Diffusion-weighted sequences are particularly useful to delineate the tumour extent, because it is a squamous cell carcinoma. But it is still vital to have the appropriate and high-resolution small field of view. MRI provides excellent anatomical definition of these structures and the components of the sphincter mechanism (see Figs. 11.1 and 11.2) and defines involvement of normal-sized lymph nodes seen on CT. If MRI is to be co-registered, it is important to use a hard couch top to avoid posterior distortion.
11.9.2 PET
An Italian group has found PET/CT useful in target volume delineation (Krengli et al. 2010). PET/CT can define both primary and nodal sites of metabolically active tumour (Bannas et al. 2011), although to our mind PET shows a larger extent than MRI. It is important to note that the positive predictive value of PET for lymph nodes is high, but the negative predictive value is less secure.
11.10 Consensus Atlas
The area of most potential variability and error is between individual radiation oncologists outlining of target and normal tissue volumes. There is a clear role for an agreed consensus/atlas (Nijkamp et al. 2012) with continuous education, training and cross-collaboration of the radiation oncologist with other specialties especially radiologists to reduce the degree of variability in tumour delineation and enhance the quality assurance within radiotherapy trials. The proposed atlas provides a delineation protocol for anal cancer.
The delineation of pelvic nodes radiologically is described in some relevant pelvic nodal atlases (Portaluri et al. 2005; Taylor et al. 2007; Lengele and Scalliet 2009; Japan Clinical Oncology Group 2010), but these are not sufficiently relevant to anal cancer. It is also curious that there are several different algorithms, which have been proposed for contouring the same pelvic nodes in prostate cancer, anorectal cancer and cervical cancer – and no consensus. The RTOG made suggestions specifically for the definitive treatment of anal cancer based on a consensus of nine experts in radiation oncology (Myerson et al. 2009) partly because of inaccurate contouring in some cases enrolled on RTOG 0529 but confined guidance to elective nodal volumes.
There is a tendency with each new atlas to design larger and larger volumes with more extensive fields and more complex methods, but there is no evidence yet that these developments improve outcome. Hence, there is no widely accepted consensus on proper selection and delineation of lymph node areas for definitive chemoradiation. In general algorithms defining CTV close to bone landmarks carry less variation than those which rely on soft tissue landmarks – particularly landmarks which vary such as the bladder. We have therefore tried to both simplify the structure to produce more compact CTVs and at the same time design individualised targets appropriate to the site of origin and clinical stage. Even then, these targets will vary according to the tumour size and stage, the sex and the individual shape of the patient.
11.11 Clinical Assessment of Primary Tumour
Clinical assessment of the tumour is essential. Information is required on the size and position of the tumour within the anus and whether it is infiltrating or exophytic. It is important to measure the distance the tumour extrudes beyond the anal margin and how far it extends cephalad (i.e. whether it extends above or below the dentate line and levators). Additionally females require a vaginal examination particularly in anterior tumours to assess if the vagina itself is directly involved or if the tumour is palpable by involving the rectovaginal septum. However should pain prevent per rectal (PR) examination, an EUA (examination under anaesthetic) should be considered. It is recommended that the treating radiation oncologist is present during the procedure to ensure that precise measurements are noted, facilitating target volume delineation and treatment planning. We consider a clinical proforma an absolute essential for accurate target delineation (clinical proforma – see Appendix 11.2).
11.12 Clinical Assessment of Inguinal Nodes
Clinical assessment of inguinal nodes is also required. Involved nodes tend to be found medially, just lateral to the pelvic tubercle, and are firm, almost analogous to a hard marble. Fixed nodes may be palpated more laterally beyond these areas in patients presenting with more extensive T3/T4 tumours.
11.13 Details of Imaging Proforma for Each Patient (Appendix 11.3)
An imaging proforma based on MRI should be completed by the MDT radiologist.
11.14 Planning
The use of a planning CT scan with target volumes delineated (primary and nodal) on each slice- and pixel-based inhomogeneity correction is considered standard practice. There are arguments for planning both in the supine and prone positions. We recommend patients should be simulated and planned in the supine position because it is more stable and reproducible without any custom immobilisation device. Although we accept that local practices may vary, some prefer that patients with very exophytic tumours extending well outside the anal canal are planned prone and bolus used. Hence, appropriate immobilisation and a treatment position with which the centre is familiar should ideally be used.
11.15 Patient Data Acquisition
The CT scan limits are the superior aspect of L3 superiorly to the mid-femur or 6 cm below a radio-opaque marker/ball bearing indicating the anal verge or the inferior extent of tumour, whichever is more inferior and can be wired. The recommended slice thickness is 3 mm. Immobilisation devices such as Vac-Lok are recommended. All patients must be scanned with a comfortably full bladder (>250 ml). For optimal set-up techniques, it is important to consider patient interventions which promote ideal imaging and the patient keeping still, i.e. advice on diet, bowel preparation, pain relief and even methods of relaxation.
11.15.1 Contrast
Intravenous contrast is mandatory unless contraindicated by virtue of allergy or renal impairment. Small bowel contrast is recommended if the small bowel is intended to be contoured as an OAR. Gastrografin 20 ml in water 45–60 min prior to the planning scan or dilute contrast agents in routine diagnostic use are useful. An intravaginal marker should be used in females.
11.15.2 Bolus
Application of bolus is more difficult if the patient is placed supine. If there are concerns, to ensure adequate dose at the anal margin, as an alternative to bolus, the patient’s buttocks can be taped together at the time of simulation and for treatment, although this position may not be easily reproducible. Bolus is not recommended to the skin overlying the groins unless tumour extends to skin surface, because the oblique incidence of the IMRT beams usually increase the superficial dose. Anyway we aim to spare the most superficial 5 mm of skin unless there are fungating nodes in the groin. However, it may be important to provide adequate photon fluence in air near the skin in these areas to account for set-up variations.
11.16 Definition of Target Volumes
Definition of target volumes and OARs has been standardised in ICRU reports 50 (ICRU 50 1993) and ICRU 62 (ICRU 62 1999).
Details of imaging proforma for each patient (Appendix 11.3)
Additional information will be available from CT, MRI and PET/CT.
11.16.1 The Primary Gross Tumour Volume
The primary gross tumour volume (GTVp), and the nodal GTV (GTVn), i.e. all involved nodal regions (on imaging or biopsy proven), should be defined and outlined on each CT slice, using all radiological imaging available, and ideally co-registered with the planning scan. The overall GTV is defined but described separately by all macroscopic tumour together with the entire circumference of the anal canal wall (GTVp) and the involved nodes’ GTVn. GTVp will extend from either the ball-bearing marker or the demarcated inferior aspect of the tumour extending below the anal margin – whichever is more inferior. Where the primary tumour cannot be identified on the CT images – often Tx (excisional biopsy with positive margins but no macroscopic disease), the anal sphincter complex, will be contoured (in addition to any observed perianal tumour extension) and will be designated as the CTVa.
Whether using a single-phase DP-IMRT or two phases (IMRT and conformal), it is recommended that all phases of treatment are planned at the same time, as the primary site and even involved lymph nodes may regress rapidly on commencement of CRT.
11.16.2 The Primary Tumour Clinical Target Volume (CTV)
The clinical target volume (CTV) represents extension around tumour and subclinical disease which cannot be seen or imaged. The CTV needs to encompass gross primary tumour CTVp, involved lymph nodes and lymph node stations potentially at risk of microscopic disease (CTVn), the mesorectum (CTVm) and the entire anal canal (CTVa). Defined landmarks should be easy to recognise.
A CTVp should be created by expanding the GTVp anisotropically by 10 mm radially to cover microscopic spread and by 15 mm superiorly and 15 mm inferiorly. This volume is created according to a computer-generated algorithm and therefore does not follow anatomical landmarks. However, anatomical boundaries should be respected, so CTVp in air, bone or any tissues, normally considered natural barriers to tumour infiltration and hence not at risk for microscopic spread, should be manually edited to avoid overlap into these nontarget areas.
11.16.3 The Primary Tumour Planning Target Volume (PTV)
A further expansion to allow for set-up and day-to-day internal organ movement should be created. 10-mm expansion is recommended on CTVps to generate these PTVs. Very little data exists for the use of IGRT and adaptive treatment plans for anal cancer. It may be necessary to insert fiducial markers into or close to the primary tumour and the anal margin to track the movement of these to provide confidence regarding tumour position. Alternatively cone beam CT scanning may be used with off-line correction. Due to the relatively poor visualisation with cone beam imaging, visualisation of the primary tumour may be difficult, and a surrogate of potential tumour movement might be required, for example, the degree of rectal gas distortion. Daily imaging and a knowledge of the department’s systematic and random errors may allow the clinician to reduce the CTV to PTV margin to 5–7 mm particularly for patients treated in the supine position. Hence, each department should audit its margin of errors to ensure the PTV margins allocated are reasonable.
11.16.4 Elective Volumes
11.16.4.1 Anal Canal CTV (CTVa)
We believe that the whole anal cancer should be considered at risk of microscopic disease and, if not covered in the initial GTV expansion, should be delineated separately and then expanded to form part of the CTV, i.e. CTVa alongside the primary tumour CTVp to create the primary tumour PTVp + a. This is rarely the case as expansion of 15 mm caudal and cephalad means the anal canal will invariably be included in the CTVp, unless the tumour involves the rectum above the dentate line. The superior extent of the anal canal can be determined on MRI scans and is usually defined superiorly by a line joining the tip of the coccyx and the most inferior aspect of the pubis. However, we do not agree with the Australasian atlas (Ng et al. 2012) that the entire ischiorectal fossa should be contoured as CTVa.
11.16.4.2 Mesorectum (CTVm)
The perirectal mesorectal region should be contoured to include perirectal nodes, but the lower part of the mesorectum is poorly visualised on CT and is even less clear more superiorly, particularly anteriorly, because other structures are not available to define its boundaries. Hence there may be a need to be more generous anteriorly. The archives suggest that in anal cancer Papillon did not formally treat the lymph nodes – although he used arc therapy. He is said to have commented that recurrences were always within the reach of his finger (i.e. 6–9 cm) and probably reflect recurrent mesorectal lymph nodes. We do not therefore recommend treatment of the upper portion or the entire mesorectum unless tumour extends to the peritoneal reflection and enlarged presacral nodes are imaged. The lower portion of the mesorectum to a maximum distance of 5 cm cephalad to the tumour should be sufficient for CTVm unless tumour extends from the anal canal above the dentate line. We suggest that CTVm = mesorectum with no further expansion + 10 mm for PTV will then suffice.
11.17 Elective Nodal Volumes (CTVn)
Much of the basis of pelvic atlases and anatomical details have been defined in patients with cervical cancers, where it was apparent that conventional techniques for cervix irradiation based on bone references often failed to encompass the planning target volume (Zunino et al. 1999).
Inclusion of the common iliac nodes, and full coverage of the entire internal iliac nodal system, by defining an upper CTV border at, or near, the sacral promontory (Das et al. 2007; Wright et al. 2010) remains an area of discussion. In the RTOG and European CTV recommendations, the elective nodal regions include common iliac nodes up to the 5th lumbar vertebra to a dose of 45 Gy. Yet, common iliac nodal involvement appears rare (1 %), and few recurrences are observed in this site. Standard inclusion within the radiotherapy field may therefore not be justified. In the Norwegian National Population Cohort (Bentzen et al. 2012), the standard superior border was at the level of the lower border of the SI joints. Only if the primary cancer extended into rectal mucosa or the nodes were considered involved did the field extend to the sacral promontory. Thus despite the fact that approximately 50 % of patients had a field extending to the lower end of the SI joint, no recurrences were observed above this treatment field (Bentzen et al. 2012).
In ACT II the superior aspect of the initial APPA field was defined as 2 cm above the inferior aspect of the sacroiliac joints, i.e. usually at the S1/S2 interface, and with the beam divergence, the estimated dose to the common iliac nodes was small (Aggarwal et al. 2012). Very few isolated recurrences are observed above this field in the ACT II dataset (Sebag-Montefiore et al. 2012).
We therefore recommend that only the more advanced (T3/T4) cancers with presacral nodes may need higher superior border extending the nodal/elective CTV to the origin of external and internal iliac nodes.
Normal-sized but potentially involved nodes cannot be reliably seen on CT or routine pelvic MRI scans. Three-dimensional lymph node mapping with the aid of lymphangiograms has been used to generate a nodal CTV guideline for gynaecologic malignancies (Chao and Lin 2002). Meticulous pioneering work by Taylor et al. (2005 and 2007) proposed the targeting of pelvic lymph nodes determined upon their predicted relationship to the pelvic vasculature which can be easily identified on CT scan especially following the administration of intravenous contrast.
The use of a margin of 7 mm was shown to cover 91, 98, 94 and 98.6 % of the common iliac, medial external iliac, anterior external iliac, and internal iliac lymph nodes, respectively. Although this study was performed in gynaecological cancer, it has gained acceptance as the basis for lymph node outlining in many pelvic cancers including high-risk prostate, bladder and penile cancer. The outlining of the vessels and subsequent expansion according to Taylor was used by the Australasian Gastrointestinal Tumour Group (AGITG) to form the basis of their atlas for IMRT planning of anal cancer (Ng et al. 2012). We have therefore recommended a 7-mm margin for elective nodal CTV around vessels.
11.17.1 External Iliac Nodes
The external iliac vessels extend anteriorly along the pelvic sidewall as they descend through the pelvis. In terms of definition, the external iliac nodes refer to those above the inguinal ligament distinguishing them from the inguinal nodes which lie below. The lateral external nodes are less well covered using the 7-mm margin. Hence a wider 10-mm margin following the iliopsoas margin should be considered. Consideration should be given to contouring the superficial iliac circumflex vein in clinically node-positive patients.
11.17.2 Internal Iliac Nodes
The internal iliac vessels sometimes have subdivisions which should be outlined and then expanded by 7 mm. Care should be taken to extend the target volume to the pelvic sidewall.
11.17.3 Obturator Node
The obturator node is not well covered using a simple expansion from the pelvic blood vessels. To cover this nodal group, a strip of 15–18 mm along the pelvic sidewall connecting the external iliac nodes to the internal iliac nodes is recommended.
11.17.4 Inguinal Lymph Nodes
Agreed boundaries of the inguinal region and the position of uninvolved inguinal lymph nodes are difficult to determine on CT imaging alone. We agree with the RTOG suggestion that the inguinal region should be contoured as a compartment (Myerson et al. 2009), rather than just using vessels. The inguinal node positions were not defined within the Taylor proforma (Taylor et al. 2007). The original ACT II protocol called for a 3-cm margin to field inferior to the anal verge treating the inguinal and femoral nodes inferiorly to this distance. This would seem to extend unnecessarily far inferiorly.
The inguinal nodes lie below the inguinal ligament (not easily visible on CT scans). We consider the inguinal compartment as extending from the superior aspect of the femoral head to 1–2 cm below the junction of the saphenous vein and femoral vein. The superficial inguinal lymph nodes form a T-shape: one row (the horizontal group) is running parallel to and below the inguinal ligament, while the other superficial row (the vertical group) is arranged vertically along the femoral/great saphenous vein. We have rarely if ever seen clinical involvement of the femoral nodes in anal cancer, unless the inguinal nodes are already grossly involved, and do not therefore recommend routine contouring of the femoral nodes.
Sartorius may be a difficult landmark. Anteriorly, the skin is not part of the volume, and the first 5 mm can be spared except in case of skin invasion from involved nodes. We prefer to use a faint line anteriorly defining the fascia and the spermatic cord more medially. Posteriorly is the deep femoral vein. The edge of the iliopsoas muscle defines the lateral border, and the edge of the adductor longus muscle, the medial border. Again there is considerable variability on the medial aspect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree