The American College of Surgeons Oncology Group (ACOSOG) conducts cancer trials that are relevant to surgeons who treat patients with breast, thoracic, and gastrointestinal cancers. ACOSOG is funded by the National Cancer Institute and is charged with conducting prospective clinical trials that address important questions in academic and community practice settings. Examples include role of axillary dissection for microscopic nodal disease, neoadjuvant therapy for organ-conserving surgery, laparoscopic rectal cancer resection, mediastinal nodal staging, and sublobar resection for early-stage non–small cell lung cancer. Such trials are relevant to most practicing surgeons.
The American College of Surgeons Oncology Group (ACOSOG) conducts cancer trials that are relevant to surgeons who treat patients with breast, thoracic, and gastrointestinal cancers. ACOSOG is funded by the National Cancer Institute and is charged with conducting prospective clinical trials that address important questions in both academic and community practice settings. Examples include role of axillary dissection for microscopic nodal disease, neoadjuvant therapy for organ-conserving surgery, laparoscopic rectal cancer resection, mediastinal nodal staging, and sublobar resection for early-stage non–small cell lung cancer (NSCLC). Such trials are relevant to most practicing surgeons.
ACOSOG was established in 1999 as a national surgeon-based clinical trial cooperative group. Early on, the scientific leadership that developed the trials consisted of surgeons but has evolved to include medical oncologists, radiation oncologists, radiologists, and pathologists. Because cancer treatment is multidisciplinary, current ACOSOG trials have multiple treatment combinations while retaining a surgical focus.
There are several reasons for academic and community surgeons to participate in national clinical trials. First, resectable cancers are commonly seen in community practices and completion of a trial is best accomplished with both academic and community surgeon involvement. There are other reasons for community surgeons to participate in clinical trials. Surgeons are tasked with improving the outcomes of surgical patients. New instruments, procedures, and therapeutic agents are a constant feature of our innovative medical culture, and community surgeons involved in trials are most likely to keep current with new technology. Furthermore, prospective trials are essential to determine safety and outcome of a new procedure or treatment. Lastly, participation in a clinical trial not only improves medical knowledge but also can enhance a surgeon’s leadership in the community. This can result in recognition as a leader in the medical community and as an advocate for science. ACOSOG recognizes the importance of community surgeons and has started to fill its scientific leadership positions with these surgeons.
A review of ACOSOG trials reveals that these studies have had an impact on surgical practice patterns and patient outcomes. The portfolio of trials is organized according to organ site and assigned to committees, including breast, gastrointestinal, and thoracic committees. Committee members include practicing surgeons, medical oncologists, radiation oncologists, statisticians, nurses/clinical research associates, and patient advocates. The committees are tasked with developing, assessing feasibility of, prioritizing, overseeing the conduct of, and promoting accrual to ACOSOG trials.
The ACOSOG breast committee has focused on important procedural and multidisciplinary cancer trials. The introduction of lymphatic mapping and sentinel lymph node (SLN) biopsy by Giuliano and associates was a major advance in breast cancer surgery and has led to other important practice-changing trials. The most notable example is ACOSOG Z0011, the phase III randomized trial of axillary lymph node dissection versus SLN dissection alone for microscopic detected lymph node metastases. For more than a century, Halsted axillary dissection has been a standard surgical procedure for breast cancer. The advent of lymphatic mapping and sentinel node biopsy changed surgical management of the axilla for breast cancer and melanoma. ACOSOG Z0011 showed no difference in local-regional control and overall survival between the two axillary procedures at 5-year follow-up. This practice-changing trial provided data disputing the need for axillary dissection in patients who have less than or equal to 2 SLNs containing microscopic metastatic disease undergoing breast-conserving surgery (BCS) with radiation.
The breast committee conducted the Z0010 trial to assess the prognostic significance of micrometastases in the SLNs and bone marrow identified by immunohistochemistry (IHC) among patients presenting with clinical stage I and II disease. The focused examination of SLNs encouraged the application of IHC technology for detection of micrometastases when routine hematoxylin-eosin staining was negative for metastatic disease. The clinical significance of IHC-detected micrometastases and the implications for postoperative adjuvant therapy have not been clear. The Z0010 trial showed no difference in local and systemic recurrence rates in patients with SLN micrometastases compared with IHC-negative SLN subjects. Trial data negate the value of routine IHC examination of SLNs in early-stage breast cancer. These two large trials required broad participation for their success. Cancer surgery is primarily done in the private-practice setting, and enrollment to trials, such as these, require the involvement of all surgeons.
SLN trials are continuing. The legacy SLN trials (Z0010 and Z0011) involved early-stage disease. There has been substantial controversy, however, about the role of SLN biopsy in locally advanced breast cancer (LABC). Patients with LABC are often treated with neoadjuvant therapy with downstaging of the primary tumor and involved axillary lymph nodes. ACOSOG Z1071 (Study Chair Dr Judy Boughey) is a 660-patient phase II study of lymphatic mapping for patients who receive neoadjuvant chemotherapy for LABC with positive axillary lymph nodes confirmed by needle biopsy. The primary objective is to determine the accuracy of lymphatic mapping and SLN biopsy after neoadjuvant chemotherapy in predicting residual nodal disease. Patients receive neoadjuvant chemotherapy and then undergo SLN biopsy and axillary lymph node dissection. This trial is rapidly accruing 40 patients a month and enrollment will be complete by November 2011. In keeping with the theme of minimizing surgical therapy, ACOSOG has undertaken a trial to look at another alternative primary tumor therapy. The Z1072 trial (Study Chair Dr Rache Simmons) involves cryoablation of less than 2-cm primary breast cancers, followed by MRI to assess for residual disease. Lumpectomy is then performed to histologically assess for residual viable tumor. If the postablation MRI proves to successfully document complete tumor ablation in this highly selected patient population, then larger randomized trials will be undertaken to validate ablation without surgical resection.
The breast committee is also conducting neoadjuvant systemic therapeutic trials for LABC to improve BCS rates. Z1031 (Study Chair Dr Matthew Ellis) is actively enrolling postmenopausal patients with clinical stage II or III palpable estrogen receptor (ER)-positive breast cancers. Instead of chemotherapy, patients receive neoadjuvant aromatase inhibitor (AI) for 16 weeks. The results of cohort A, 377 patients, were first reported at the American Society of Clinical Oncology 2010 annual meeting (ASCO 2010). The clinical response to AI therapy was 60%. Those patients judged by their surgeons to be candidates for BCS before neoadjuvant AI therapy had an 85% BCS rate. There were 150 patients judged to require mastectomy and, after neoadjuvant AI therapy, 51% were converted to BCS. These are promising results, but the investigators are not satisfied with a 51% BCS rate. The study revealed that there is a subset of patients with highly ER-positive tumors who did not respond to AI therapy. This indicates that there is another mechanism or proliferative growth pathway overcoming the antiendocrine therapy. In cohort B of Z1031, a marker of proliferation, Ki67, is being analyzed in specimens from pretreatment biopsy and from a second biopsy at 2 weeks to select patents most likely to respond to AI for continuation of therapy. Those with an elevated Ki67 (>20%) after 2 weeks of AI therapy are switched to chemotherapy with the goal of assessing pathologic response in this selected patient population. Correlative science studies are ongoing to identify other predicators of AI resistance to improve the BCS rate.
Critical to the success of Z1031 is the ability of surgeons to acquire a research core needle biopsy of the palpable primary tumor before AI therapy is started and during the course of therapy. The specimen is frozen and sent to the ACOSOG tumor bank for RNA and DNA analysis. There is an emerging technology of whole genome sequencing of the tumor DNA looking for mutations of proliferative pathway genes. Specific mutations in KIT, BRAF, and EGFR genes result in susceptibility to specific oral kinase inhibitors and are good examples of how DNA sequencing can detect gene mutations and direct targeted therapy. Remarkable laboratory investigation is only possible with the acquisition of well-preserved specimens of primary tumor. Every day, surgeons are resecting primary tumors and have the ability to acquire fresh tumor tissue for DNA analysis.
Z1041 (Study Chair Dr Aman Buzdar) addresses the use of targeted trastuzumab-anthracycline therapy for LABC that is HER2neu positive. In a pilot study of this regimen, pathologic complete response (pCR) rates were as high as 65%. In this randomized trial, the initial regimen is compared with a similar regimen in which trastuzumab is not given concurrently with 5-fluorouracil, epirubicin, and cyclophosphamide (FEC) to compare efficacy for pCR and variance in toxicity. The rate of BCS will be assessed and correlative studies will assess for markers to chemosensitivity.
The gastrointestinal committee trial portfolio includes studies addressing surgical issues, adjuvant therapy, and neoadjuvant approaches for minimizing surgical intervention. Z9001 (Study Chair Dr Ron DeMatteo) is a phase III, double-blind, randomized adjuvant trial of placebo versus imatinib for resected gastrointestinal stromal tumors (GISTs). This trial opened in 2001 and completed accrual of 713 evaluable patients in 2007. There were considerable concerns about the feasibility of completing this trial when only 5000 new GIST cases per year are diagnosed in the United States. In 2001, the National Cancer Data Base was queried to identify hospitals with a high volume of GIST patients; it was discovered that there were no high-volume sites. GIST is treated by community surgeons. The trial enrolled 717 GIST subjects from 234 sites. Although GIST is an uncommon cancer, surgical resection and investigational targeted therapy can be done in a community setting. Without a large number of participating sites, this first adjuvant trial of a novel targeted agent would not have been possible. The Z9001 GIST adjuvant trial shows that when a trial asks a scientifically important question, there is broad participation. This trial also emphasized that a clinical trial must have impact on clinical practices and therein lays the importance of the science to practicing surgeons.
The gastrointestinal committee has conducted neoadjuvant trials that facilitate minimally invasive surgical procedures. Z6041 (Study Chair Dr Julio Garcia-Aguilar) is a completed phase II trial of neoadjuvant chemoradiation therapy followed by local excision of TIN0M0 rectal carcinomas less than 4 cm. The early results of the trials were reported at ASCO 2010. One objective of this study is to assess the pCR rate in resected specimens. There were 79 evaluable patients with a 43% pCR. An R0 resection with local excision was achieved in 98% of patients. A significant limitation of the oxaliplatin-capecitabine radiation therapy, however, was its toxicity. Thus, a successor trial is in development with the objective of reducing the toxicity of the neoadjuvant regimen while maintaining a high pCR rate.
Mutational analysis of the primary tumor biopsy specimens from Z6041 is currently being done. There is considerable interest in KRAS mutation and radiotherapy resistance. The objective of these analyses is to develop a predictive model for pCR using mutation analysis of KRAS, other proliferative pathway genes, or DNA repair genes. Such investigations may give clues to select targeted agents that maximize tumor downstaging to achieve an R0 local excision for early rectal cancer.
The gastrointestinal committee is committed to prospectively assessing novel surgical procedures. Z6051 (Study Chair Dr James Fleshman) is a phase III trial comparing laparoscopic-assisted resection with open resection for rectal cancer. A major quality indicator for rectal cancer resection is total mesorectal excision (TME). TME requires an intact mesorectum and covering peritoneal envelope to the level of rectal transection with no coning in of the mesorectum above the point of transection. This trial will determine if laparoscopic-assisted resection is not inferior to open rectal resection based on (1) circumferential margin, (2) distal margin, and (3) completeness of TME. This trial is open and has enrolled 206 patients with a monthly accrual rate of 9 patients a month. The accrual goal is 480 patients with an estimated completion date of May 2013.
The thoracic committee has been actively involved with trials that focus on accurate early lung cancer staging, resection techniques for stage 1 disease, and locally advanced esophageal adenocarcinoma. Z30 (Study Chair Dr Mark Allen) is a phase III trial comparing mediastinal lymph node dissection with mediastinal lymph node sampling for T1N0N1 NSCLC. This trial enrolled 1111 patients in fewer than 5 years. In 2006, Allen and colleagues published the perioperative outcomes for the two mediastinal nodal staging procedures. There were no differences in hospital length of stay, chest tube days, and complications. Darling and colleagues recently reported that at 6.3-year follow-up there was no difference in survival between the two mediastinal nodal staging procedures.
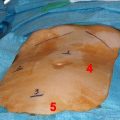
An important clinical question in thoracic surgical oncology is risk of local recurrence after a sublobar resection for T1 NSCLC in those patients who are not candidates for lobectomy because of the higher risk of complications. Local recurrence could be as high as 20%. Z4032 (Study Chair Dr Hiran Fernando) is a phase III trial comparing sublobar resection with sublobar resection plus brachytherapy. The hypothesis states that radiation seeds placed over the staple line of the sublobar resection reduce local recurrence. The primary objective is to determine local recurrence rates between the two treatment arms. The trial completed accrual of 227 patients in early 2010 and follow-up continues for recurrence. Fernando and colleagues recently reported that brachytherapy did not adversely affect postoperative pulmonary function or dyspnea scores.
The scientific questions of ACOSOG trials are encountered in everyday practice. These questions are relevant to practicing surgeons. Community surgeons contribute to 40% of ACOSOG enrollment. Although the legacy trials focused on surgical procedures, the current trials are more multidisciplinary, demonstrating the maturity of ACOSOG and its network of oncologists in all specialties. Because ACOSOG trials focus on early disease and surgical management questions, these trials should appeal to all surgeons. These trials have demonstrated surgeons’ ability to acquire fresh tissue at the time of surgery for central specimen bank storage. Surgeons in both community and academic settings have been highly successful in fresh tissue acquisition, which is critical to ACOSOG research aims. Surgeons have taken on the complex task of obtaining informed consent for tissue acquisition for laboratory investigations, such as DNA sequencing, and, because they evaluate patients with resectable disease, they are able to answer questions and reassure patients that their privacy will be protected in these investigations.
ACOSOG has worked diligently to provide a broad portfolio of trials that is relevant to practicing surgeons who treat breast, gastrointestinal, and thoracic malignancies. The ACOSOG Web site provides information about membership, meetings, and protocols. This is research for practicing surgeons who are committed to improving the treatment of their cancer patients. These trials require surgeon leadership to successfully accrue patients who have early-stage disease. Surgeons must decide to offer their patients participation in prospective clinical trials to advance surgical knowledge.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree