Allogeneic stem cell transplant remains the only curative option for β-thalassemia major. In patients with good risk features it is reasonable to anticipate a greater than 90% chance of a successful transplant outcome. The conventional risk stratification system has limitations and alternative systems are being explored to better identify subsets that require innovative approaches. Several novel regimens have been evaluated to reduce treatment-related morbidity and mortality. There remain challenges in improving the clinical outcome of high-risk patients. There are limited data on the role of splenectomy before transplantation or optimal posttransplant chelation and care of these patients.
Key points
- •
Allogeneic stem cell transplant remains the only curative option for patients with thalassemia major.
- •
Current risk stratification strategies have limitations and fail to recognize a very high risk subset of patients in whom a conventional conditioning regimen is associated with an unacceptable risk of treatment related mortality, especially in countries where pre-transplant medical therapy is sub-optimal.
- •
A number of novel conditioning regimen have been evaluated in an effort to improve the transplant outcomes in high risk patients. In the absence of controlled clinical trials to compare these it is difficult to make strong recommendation for one or the other of these approaches. A treosulfan based conditioning regimen has shown promise in high risk cases.
- •
Bone marrow is the preferable source of stem cells. While there is data to suggest a potential role for peripheral blood stem cells in reducing the risk of graft rejection in high risk cases this cannot be considered a recommendation based on the available data.
- •
Results from matched unrelated donor stem cell transplant have improved with the use of high resolution leukocyte antigen (HLA) typing and can be considered in low risk patients with a fully matched donor. There is a potential role for related cord blood transplants and if done should be in a center which has facilities with considerable experience in this procedure. It should preferably be done only in low risk cases. Unrelated cord blood transplants and haploidentical transplants should preferably be done only in the setting of a clinical trial.
Introduction
Allogeneic stem cell transplantation (SCT) remains the only curative option for patients with β-thalassemia major. The correction of this disorder by an allogeneic stem cell transplant was first described by Thomas and colleagues. A conditioning regimen of busulfan and cyclophosphamide was subsequently established for SCT in this condition. This myeloablative therapy forms the basis for the current conditioning regimens in this condition. Reduced-intensity conditioning regimens have been attempted, with some success, although the increased risk of rejection with this approach has limited its widespread acceptance. To date more than 3000 transplants have been reported worldwide for this condition. The current risk stratification of patients with β-thalassemia major undergoing a myeloablative allogeneic SCT classifies them into 3 risk groups (Pesaro classes I, II, and III), based on liver size (>2 cm), presence of liver fibrosis, and inadequate iron chelation. Recent advances have attempted to improve on the risk stratification to better identify subsets that are likely to do poorly and need alternative/improved strategies to reduce rejection and treatment-related mortality (TRM) among patients in class III. There has been some progress in developing new protocols; preliminary studies have shown the ability of such regimens to reduce TRM and rejection. Of special interest is the role of intravenous busulfan and treosulfan in conditioning regimens and efforts to reduce the risk of sinusoidal obstruction syndrome (SOS). The development of new conditioning regimens has, in general, been empiric with the evaluation of a variety of drugs and doses and schedules with no controlled studies to validate the claims of superiority of one rather than another. Of recent interest is the role of matched unrelated donor (MUD) stem cell transplants, cord blood stem cell transplants, and haploidentical stem cell transplants. Their potential lies in expanding the number of recipients for this curative strategy. Although there have been significant challenges and concerns with these alternate donor sources there have also been steady improvements in clinical outcome with these approaches that has put them on the threshold of being considering as standard of care. The role of splenectomy before allogeneic SCT is unclear, although there are theoretic benefits. There are limited data on optimal posttransplant chelation therapy, immune reconstitution, and long-term care after transplantation. In the absence of controlled clinical trials to address issues such as optimal conditioning regimen, graft source, use of alternate donors, and graft-versus-host disease (GVHD) prophylaxis clinicians have to rely on expert and consensus opinions, which have significant limitations. This article addresses some of these issues and the advances in each of these areas.
Introduction
Allogeneic stem cell transplantation (SCT) remains the only curative option for patients with β-thalassemia major. The correction of this disorder by an allogeneic stem cell transplant was first described by Thomas and colleagues. A conditioning regimen of busulfan and cyclophosphamide was subsequently established for SCT in this condition. This myeloablative therapy forms the basis for the current conditioning regimens in this condition. Reduced-intensity conditioning regimens have been attempted, with some success, although the increased risk of rejection with this approach has limited its widespread acceptance. To date more than 3000 transplants have been reported worldwide for this condition. The current risk stratification of patients with β-thalassemia major undergoing a myeloablative allogeneic SCT classifies them into 3 risk groups (Pesaro classes I, II, and III), based on liver size (>2 cm), presence of liver fibrosis, and inadequate iron chelation. Recent advances have attempted to improve on the risk stratification to better identify subsets that are likely to do poorly and need alternative/improved strategies to reduce rejection and treatment-related mortality (TRM) among patients in class III. There has been some progress in developing new protocols; preliminary studies have shown the ability of such regimens to reduce TRM and rejection. Of special interest is the role of intravenous busulfan and treosulfan in conditioning regimens and efforts to reduce the risk of sinusoidal obstruction syndrome (SOS). The development of new conditioning regimens has, in general, been empiric with the evaluation of a variety of drugs and doses and schedules with no controlled studies to validate the claims of superiority of one rather than another. Of recent interest is the role of matched unrelated donor (MUD) stem cell transplants, cord blood stem cell transplants, and haploidentical stem cell transplants. Their potential lies in expanding the number of recipients for this curative strategy. Although there have been significant challenges and concerns with these alternate donor sources there have also been steady improvements in clinical outcome with these approaches that has put them on the threshold of being considering as standard of care. The role of splenectomy before allogeneic SCT is unclear, although there are theoretic benefits. There are limited data on optimal posttransplant chelation therapy, immune reconstitution, and long-term care after transplantation. In the absence of controlled clinical trials to address issues such as optimal conditioning regimen, graft source, use of alternate donors, and graft-versus-host disease (GVHD) prophylaxis clinicians have to rely on expert and consensus opinions, which have significant limitations. This article addresses some of these issues and the advances in each of these areas.
Pretransplant risk stratification and age at transplantation
The conventional risk stratification of patients with β-thalassemia major undergoing a myeloablative allogeneic SCT classifies them into 3 risk groups (Pesaro classes I, II, and III) based on liver size (>2 cm), presence of liver fibrosis, and inadequate iron chelation (adequate chelation was defined as initiation of chelation by 18 months from date of first transfusion and chelation with deferoxamine administered subcutaneously over 8–10 hours/d for at least 5 days a week). Patients with none of these risk factors are classified as class I, those with 1 or 2 of these risk factors are class II, whereas those patients who have all 3 adverse risk factors are classified as class III. Patients in class I and II are considered to be low risk and have excellent long-term outcomes following an allogeneic SCT. In contrast, class III patients are considered high risk and have inferior outcomes following SCT. The authors further showed the ability of this classification to discriminate the thalassemia-free survival (TFS) and overall survival (OS) between these groups. In that initial report, age up to 15 years did not affect TFS.
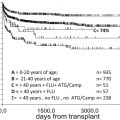
This risk stratification has not been validated in different populations, especially in a group of patients with inadequate medical care before an allogeneic SCT (as commonly seen in developing countries where such transplants are increasingly done). When applied to such a population with inadequate medical therapy before transplantation there was skewing in the distribution of patients, with most being class III, and there was also significant heterogeneity in clinical outcomes among this class III subset that could not be recognized by the existing risk stratification strategy. We had previously reported on the limitations of this classification in our population and, based on statistical analysis, had further subdivided class III patients into a high-risk subset (class III HR) based on age greater than or equal to 7 years and liver size greater than or equal to 5 cm ( Fig. 1 ). We had proposed that this high-risk subset would need innovative strategies for improving outcomes following an allogeneic SCT, in view of their dismal outcomes with the conventional busulfan plus cyclophosphamide conditioning regimens. A subsequent registry-based analysis Center for International Blood and Marrow Transplant Research (CIBMTR) showed a similar adverse effect of age greater than or equal to 7 years and hepatomegaly on clinical outcomes after transplantation. In contrast with this, the European Society for Blood and Bone Marrow Transplantation (EBMT) registry analysis showed that the adverse effect of age occurred at a threshold of 14 years. This difference in the threshold age predicting poor clinical outcome is probably directly related to adequacy of medical care before transplantation in Europe in contrast with our series and the CIBMTR series in which a significant proportion of cases (>60%) were from developing countries. Based on the available data, it is reasonable to retain the Pesaro risk stratification strategy, recognizing its limitations and its inability to identify a very-high-risk subset.
Patients should ideally receive an allogeneic SCT within the first 2 to 3 years of life before significant iron-related organ damage has set in. There are very limited data for allogeneic SCT in adults (>18 years), although the TRM has consistently been reported to be more than 25% and is probably best avoided.
Conditioning regimens
The Pesaro group initially reported the adverse outcome in class III patients conditioned with a similar regimen as used for class I and II, with a TFS of 53% among class III patients versus 85% for the rest. They also noted a nonrejection mortality of 39% in this group. To improve on the outcome and reduce non–transplant-related mortality they reduced the dose of cyclophosphamide to 160 mg/kg from 200 mg/kg. This small change reduced TRM but resulted in an increase in rejection rate from 7% to 30%. The same group in March 1997 developed a conditioning regimen that started on day -45 with azathioprine and hydroxyurea, fludarabine from day -17 to -13, and busulfan 14 mg/kg with cyclophosphamide 160 mg/kg. With this new regimen, this group reported an 85% event-free survival (EFS) and a rejection rate of 8%.
Class III and, more specifically, the class III HR subset have a high risk of graft rejection and regimen-related toxicity (RRT), especially SOS leading to multiorgan failure and death. These complications are related to the high degree of alloimmunization and iron overload–related end-organ damage in this cohort. The poor clinical outcome in this subset of older patients with very poor pretransplant medical therapy, as reported previously, is not reflected in the Western literature because of the use of adequate blood transfusion and chelation support before transplantation. However, when such a population is transplanted, even in a developed country with expertise in such transplants, the rejection rate is as high as 34%.
The introduction of intravenous busulfan into conditioning regimens had the promise of more uniform pharmacokinetics and reduced toxicity (reviewed by Ciurea and Andersson ). A recent study of 57 patients with thalassemia major conditioned with intravenous busulfan along with oral defibrotide for SOS prophylaxis had a low incidence of SOS, with only 1 of 63 patients fulfilling the criteria for SOS. However, there are too few data on clinical outcomes comparing oral versus intravenous busulfan to state conclusively that the latter is superior with regard to TFS and OS.
Treosulfan (dihydroxybusulfan), has recently attracted a lot of attention as an agent to replace busulfan in view of its favorable toxicity profile. It is structurally similar to busulfan. Unlike busulfan it is water soluble and easy to reconstitute and administer intravenously. It also has a linear pharmacokinetic profile with good systemic exposure and very low intraindividual and interindividual pharmacokinetic variability. In phase I studies even at cumulative doses of 56 gm/m 2 (a dose not usually reached when used as an agent in conditioning regimens) there was no dose-limiting hepatic, renal, neurologic, or cardiac toxicity. Hepatic SOS is a common problem with conventional busulfan-based myeloablative regimens with an incidence ranging from 5% to 40%. Use of a busulfan-based conditioning regimen was associated with an increased incidence of SOS on a multivariate analysis in a prospective study. The link between pretransplant iron overload and SOS is similarly well recognized. Although targeted busulfan levels and prophylaxis with defibrotide have significantly reduced this complication in patients with thalassemia major, it is still a significant complication among class III HR patients. In the absence of such interventions, the cumulative incidence of SOS in the very-high-risk subset (class III HR) of patients has been reported to be as high as 78% and, in 24% of such cases, it led to multiorgan failure and death. Treosulfan was hence especially attractive in the context of an allogeneic SCT for high-risk β-thalassemia major because of its reported low hepatic toxicity profile and consistent pharmacokinetic profile, which are both significant problems with conventional busulfan in this population. However, it is also important to recognize that the pharmacokinetic profile of treosulfan-based regimens, both in patients with thalassemia major and when it is combined with other high-dose chemotherapeutic agents as part of the conditioning regimen, have not been studied extensively.
The first report on the use of treosulfan being used as part of the conditioning regimen for thalassemia was by Bernado and colleagues in a small series of 20 patients, of whom 45% were class III and 18 received matched unrelated stem cell transplants. Only 2 patients in this series developed transient liver enzyme increase. In addition, the conditioning consisted of thiotepa and fludarabine, was well tolerated, and 17 cases had complete chimerism. The same group recently reported on their expanded experience with this reduced toxicity myeloablative regimen. In this expanded series of 60 cases with thalassemia major the median age was 7 years, although only 7% of the 48 children were class III and the remaining 12 patients were adults. Forty (67%) of the patients received an unrelated donor transplant and in 47 (79%) the stem cell source was bone marrow. The regimen as previously reported was well tolerated with low (<10%) graft failure and a TFS of 84%.
A small series reported a comparable outcome between a similar treosulfan-based (n = 28) and a historical busulfan-based regimen (n = 12). However, the median age in the busulfan group was 7 years versus 9.6 years in the treosulfan group, and the treosulfan group had 75% class III patients of whom 52.4% were class III HR as defined previously. In the busulfan arm 58% were class III and the number that fulfilled the criteria of class III HR is not available. The age and risk group of the patients in the treosulfan arm who died because of RRT (n = 4) and those who had a graft rejection (n = 2) are not available. As reported previously, the outcome of class III HR can be significantly different from class III as a whole. Interpreting these data and comparing the 2 groups without this information must be done with caution, especially because of the small numbers in both groups. The inferior outcome in the treosulfan arm is likely to be related to the biology of class III HR rather than the conditioning regimen.
Our group recently reported our experience showing a clear advantage of a treosulfan-based regimen on the clinical outcome of class III as a whole and the subset of class III HR was recently reported. A significant reduction in nonrelapse mortality and RRT, especially SOS, was shown in the class III HR compared with a historical control arm that had used a conventional busulfan-based conditioning regimen.
However, in this very-high-risk group there was a significantly increased risk of mixed chimerism, which could be overcome with the use of a peripheral blood stem cell graft (PBSC). The use of this regimen with a PBSC graft translated to a significantly superior OS and EFS in the class III HR subset without a significant increased risk of GVHD.
More recently, Anurathapan and colleagues reported a novel approach of administration of 1 or 2 courses of immune-suppressive therapy with a combination of fludarabine and dexamethasone 1 to 2 months before the start of conditioning and followed this up with a reduced toxicity myeloablative conditioning regimen consisting of fludarabine, intravenous busulfan, and antithymocyte globulin with promising results in a small series of 18 patients with class III HR thalassemia major. Table 1 summarizes the data on attempts to improve the clinical outcome.
| Study, Year | N | Median Age (y)/(Range) | Proportion in Class III (%) | Proportion in Class III HR a (%) | Major Defining Feature of Change in Protocol | TRM (%) | Graft Rejection (%) | EFS (%) | OS (%) |
|---|---|---|---|---|---|---|---|---|---|
| Lucarelli et al, 1996 b | 115 | 11 (3–16) | 100 | NA | Reduction in cumulative cyclophosphamide from 200 mg/kg to 160 mg/kg | 24 | 35 | 49 | 74 |
| Sodani et al, 2004 | 33 | 11 (5–16) | 100 | NA | Reduction in cyclophosphamide dose to ≤160 mg/kg. Addition of azathioprine and fludarabine and intensification of immunosuppression. Suppression of erythropoiesis by hypertransfusion, chelation, and hydroxyurea starting from day -45 | 6 | 6 | 85 | 93 |
| Gaziev et al, 2010 | 71 | 9 (1.6–27) | 57.3 | NA | Intravenous busulfan, dose adjustments with therapeutic drug monitoring | 7 | 5 | 87 | 91 |
| Chiesa et al, 2010 | 53 | 8 (1–17) | 47 | NA | Intravenous busulfan, dose adjustments with therapeutic drug monitoring | 4 | 15 | 79 | 96 |
| Chiesa et al, 2010 c | 25 | NA | 100 | NA | Intravenous busulfan, dose adjustments with therapeutic drug monitoring | 4 | 34 | 66 | 96 |
| Bernardo et al, 2012 | 60 | 7 (1–37) | 27 d | NA | Treosulfan-based conditioning regimen | 7 | 9 | 84 | 93 |
| Choudhary et al, 2013 | 28 | 9.6 (2–18) | 75 | 39 | Treosulfan-based conditioning regimen | 21 | 7 | 71 | 79 |
| Anurathapan et al, 2013 | 18 | 14 (10–18) | 100 | NA | Preconditioning immunosuppression therapy with fludarabine and dexamethasone; 1 or 2 courses 1 to 2 mo before transplantation. Conditioning regimen of fludarabine with intravenous busulfan | 5 | 0 | 89 | 89 |
| Mathews et al, 2013 | 50 | 11 (2–21) | 100 | 48 | Treosulfan-based conditioning regimen with PBSC graft in 74% | 12 | 8 | 79 | 87 |
| Mathews et al, 2013 e | 24 | 12 (3–21) | 100 | 100 | Treosulfan-based conditioning regimen with PBSC graft in 74% | 13 | 8 | 78 | 87 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree