II. OCULAR HISTORY AND PHYSICAL EXAMINATION FOR THE ALLERGIST
A. Ocular history
A detailed and accurate history is the most important element in distinguishing allergic from nonallergic causes of conjunctivitis as they commonly reveal recent exposure to individuals with conjunctivitis or upper respiratory tract
infections, sexual activity, association with animals that may cause various forms of infectious conjunctivitis, and systemic autoimmune disorders.
1. Age plays a role in the evaluating potential infectious causes. In preschool children, the conjunctivitis-otitis media syndrome occurring frequently is usually caused by nontypeable Haemophilus influenzae or Streptococcus pneumoniae. In teenagers and adults, a sexual history may suggest a chlamydial or a neisserial infection.
2. Direct questioning of the patient will often reveal the frequent use and abuse of over-the-counter (OTC) medications, such as vasoconstrictors or artificial tears, cosmetics, or contact lens wear, all capable of producing inflammation (conjunctivitis medicamentosa or toxic keratopathy).
3. Knowledge of systemic diseases such as rheumatoid arthritis will heighten the awareness of associated autoimmune-related ocular conditions such as keratoconjunctivitis sicca (KCS) or scleromalacia.
4. As with all allergies, environmental factors and time of onset of symptoms must be addressed, including seasonal variation and exposures (i.e., smoking, cleaning supplies, pets, air-conditioning, carpets, and other sources of irritants).
B. Ocular symptoms
Ocular symptoms are often nonspecific, such as tearing, irritation, stinging, burning, and photophobia as they involve the four classical signs of inflammation, calor (heat), dolor (pain), rubor (erythema), and tumor (swelling), in addition to tearing, irritation, stinging, burning, and photophobia.
Symptoms tend to improve with cool, rainy weather and are exacerbated by warm, dry weather.
1. Itching (pruritus) is the hallmark of allergic conjunctivitis that can be mild or prominent and may last from hours to days; it is often described as mild to severe. Burning and grittiness may signify other forms of pathology such as dry eye. A stringy or ropy discharge is characteristic of a persistent ocular allergy and may range from serous to purulent. A purulent discharge, morning crusting, and difficulty opening the lids are characteristics of bacterial infection, especially with gram-negative organisms (e.g., Neisseria and Haemophilus). Environmental allergens typically affect both eyes at once, although a unilateral reaction may result if one eye is inoculated with animal hair or dander.
2. Most environmental allergen exposures are associated with bilateral symptoms, whereas a unilateral conjunctival involvement suggests an infectious etiology that is commonly associated with a palpable, ipsilateral preauricular node.
3. Ocular pain is not a feature of acute seasonal or perennial allergic conjunctivitis but suggests either an extraocular process such as a corneal abrasion, scleritis, or foreign body or an intraocular process such as uveitis, commonly associated with photophobia. The pain is sharp and sometimes piercing in character. Retro-orbital dull pain is associated with ethmoidal sinusitis.
C. Ocular examination
The examination starts with inspection of the face and area surrounding the eye to a more focused exam of the conjunctiva. A horizontal nasal skin crease (“allergic salute”) suggests a diagnosis of allergic rhinitis. Scratches and scars on the face or eyelid suggest ocular injury. In addition, palpation of the sinuses and the preauricular, submandibular, and cervical chain lymph nodes are diagnostically important.
1. Eyelid, Periocular Tissue and Eyeball
a. Careful examination of periorbital tissue can demonstrate blepharitis, dermatitis, swelling, discoloration, ptosis, or blepharospasm. Eyelid or nasal vesicular eruptions are often seen in ophthalmic zoster but can also reflect recurrent bacterial infections, such as staphylococcal blepharoconjunctivitis secondary to constant rubbing of the eyelids. The subcutaneous layer contains loose areolar tissue and little subcutaneous fat, which allows the greatest potential for fluid accumulation leading to periorbital edema especially prominent around the lower lids due to the effects of gravity.
b. The normal eyelid just touches the iris (not the pupil). In exophthalmos, the eyelid does not touch the iris (note visible white of the sclera) with extension of the globe beyond the bony portion of the orbit. The ptotic eyelid covers most of the upper iris, approaching the pupil.
c. The junction point between the external and internal portion of the eyelid is the transition where the meibomian glands add the lipid component to the tear fluid. A rounded, plugged meibomian gland is consistent with a
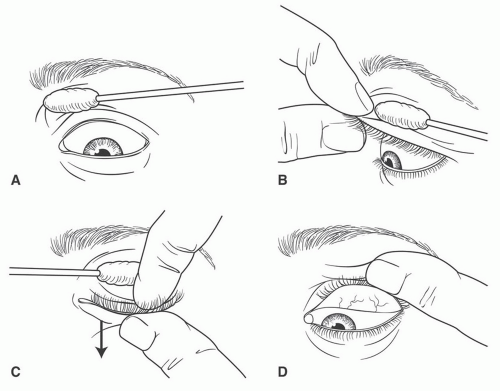
hordeolum (stye). Conjunctival involvement may present with chemosis, hyperemia, cicatrization, or papillae formation on the palpebral and bulbar membranes. The presence of increased or abnormal secretions should also be noted. Eversion of the upper eyelid requires experience to accomplish correctly (see III.B and
Figure 7-3).
d. “Allergic shiners” are ecchymotic-looking areas beneath the eyes and may be confused with the “raccoon sign” associated with head trauma.
e. Skin of lids and/or face may demonstrate evidence of acne rosacea, seborrhea, psoriasis, or other dermatoses.
f. Palpation of the eyeball can demonstrate a hard “golf ball” texture and is consistent with increased intraocular pressure, which with associated pain or blurring of vision requires an immediate referral to an ophthalmologist.
2. Conjunctiva
a. The conjunctiva is composed of two immunologically active layers: the epithelial and substantia propria separated by the epithelial
basement membrane. Mast cells (˜6,000/mm
3), lymphocytes, and other inflammatory cells normally are found in the substantia propria, just below the junction with the epithelium. Normal ocular epithelia do not contain any mast cells, eosinophils, and basophils but are found in chronic ocular allergic inflammatory disorders.
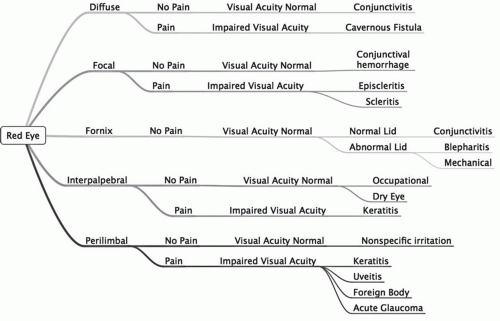
b. A velvety, beefy-red conjunctiva suggests a bacterial cause, while a milky appearance—the result of obscuration of blood vessels by conjunctival edema—is characteristic of allergy. The bulbar and tarsal conjunctivae are examined for the presence of hyperemia, follicles, cysts, chemosis, hemorrhage, abrasion, ulcers, foreign body, lacerations, and growths. The location of conjunctival redness is associated with specific disorders (
Fig. 7-2).
3. Tear film
a. The conjunctival surface is bathed with a thin layer of tear film, which is composed of an outer lipid layer, a middle aqueous layer, and an inner mucoprotein layer. This mixture decreases the evaporation rate of the aqueous portion. A defect in any of the three portions leads to a form of dry eye syndrome.
b. Ocular secretions that are “sticky” (causing “glued” eyelids) or the presence of morning crusting are associated with infection. A clear, white, stringy or ropy discharge is seen with allergic etiologies. Any secretion in the conjunctival fornix is abnormal. Mucous adhering to the corneal or conjunctival surfaces is considered pathologic.
c. The cornea is best examined with a slit lamp biomicroscope, although many important clinical features can be seen with the naked eye or with the use of an ophthalmoscope. The cornea should be perfectly smooth and transparent. The application of fluorescein reveals
corneal lesions with small spots indicating a form of keratitis, and a corneal defect suggests an erosion or an ulcer. The anterior chamber should be clear; clouding of the aqueous humor may be due to blood (hyphema) or the settling out of pus (hypopyon). An estimate of the anterior chamber depth can be made by illuminating it from the side with a penlight; if the iris creates a shadow, then there is a high index of suspicion for increased intraocular pressure (i.e., glaucoma) and an immediate referral to an ophthalmologist.
d. The limbus is the zone at the border of the cornea and the sclera and is the area that becomes intensely inflamed with a deep pink coloration in cases of anterior uveitis or iritis, the so-called ciliary flush. Discrete swellings with small white dots indicate degenerating cellular debris (Trantas’ dots or Horners’ points), commonly seen in vernal and atopic conjunctivitis.
e. Cataracts can be detected by funduscopic examination and are associated with atopic disorders and chronic corticosteroid use and/or intraocular inflammation. If detected, the patient should be referred to an ophthalmologist. The presence of a “red reflex” on funduscopic exam suggests normal light penetration to the posterior portion of the globe. In contrast, a dullness or grey appearance suggests the presence of cataracts. Homogenous posterior cataracts are common with chronic steroid use, while anterior cataracts are reported with AKC.
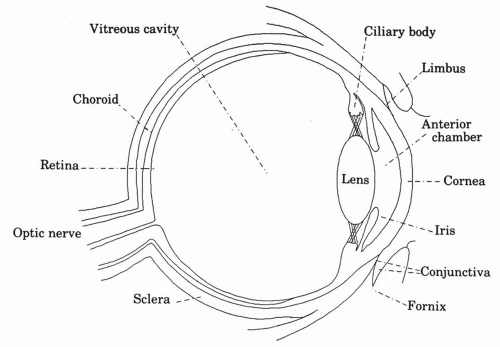
f. The uvea is the most immunologically active tissue within the eye. The uvea comprises a continuous layer of iris, ciliary body, and choroid and possesses a rich vascular architecture and pigment within the alymphatic globe of the eye. The ciliary body is the production site of a filtrate, the aqueous humor, and is similar to other structures that produce a filtrate, including the renal glomerulus (urine) and the choroid plexus (cerebrospinal fluid). In addition, disturbances in aqueous humor production or outflow obstructions can cause increased intraocular pressure (i.e., glaucoma). These filtration sites are involved in clinical disorders associated with circulating immune complexes. Although there is a paucity of mast cells within the uveal tissue, there is a notable increase in mast cell numbers in uveitis. However, the predominant inflammatory cell type in uveitis is the lymphocyte.
g. Immunologic involvement of the optic nerve is commonly associated with pain on movement in patients with optic neuritis while the ischemic events of temporal arteritis can be associated with painless loss of vision (“amaurosis fugax”).
III. PROCEDURES
A. Ophthalmoscopy
The direct (handheld) ophthalmoscope provides approximately 14× magnification. The ophthalmoscope lens settings of +8 will assist the physician in focusing on the anterior segment to reveal corneal opacities or changes in the iris or lens. Decreasing the power of the lens from +8 to −8 will increase the depth of focus so that the examiner can move from the anterior segment progressively through the structures including the vitreous and reach the retina.
The green light filter delineates small aneurysms and hemorrhages as black seen in autoimmune disorders (e.g., Systemic Lupus Erythematosus, vasculitis).
B. Eversion of the upper eyelid
Examination of the palpebral conjunctiva is performed in a stepwise fashion (
Fig. 7-3). Eversion of the lower lid is simply performed by having the patient look upward while the lower eyelid is drawn downward with examiner’s index finger applied to the orbital portion. This procedure is helpful when looking for papillary and follicular development in patients with more chronic forms of conjunctivitis.
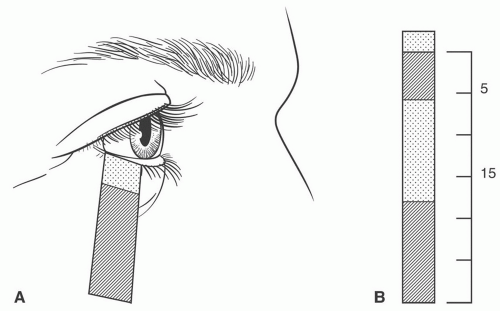
C. Dry eye tests
1. The Schirmer tear test with preprinted measures (Eagle Vision, 8500 Wolf Lake Drive, No. 110, Memphis, TN 38133, USA) is the most commonly used and easily performed test for the evaluation of dry eye (tear film dysfunction) (
Fig. 7-4).
2. The development and availability of new technology (TearLab; FDA 510(k) k083184) enables the clinician to collect and measure osmolarity in 50 nL sample with minimal disturbance of the tear film using a handheld device (TearLabs, www.tearlab.com).
D. Staining procedures
1. Fluorescein staining is the best clinical means of diagnosing the presence of corneal epithelial surface defects and can be used to examine the cornea,
conjunctiva, precorneal tear film, and tear breakup time. Fluorescein is applied (Fluor-I-Strip, Ayerst Laboratories, Inc., Philadelphia, PA) via strip or with a liquid dropper and examined using a cobalt blue filter to best appreciate the staining pattern of the conjunctiva and cornea. Of note, soft contact lenses must be removed prior to fluorescein instillation to prevent their permanent staining. It is important to wait at least 1 hour after completion of the examination before replacing the soft contact lenses.
2. Rose bengal (RoseGlo—Wilson Ophthalmic Corp, Mustang, OK), a derivative of fluorescein, stains only dead and degenerating (not denuded) epithelium of the conjunctiva and cornea. Rose bengal causes stinging and can stain facial skin and clothing quite easily. Both rose bengal and lissamine green stain dead or degenerating epithelial cells and mucous. Lissamine green has the advantage over rose bengal to fade relatively quickly and to be nonirritating.
E. Conjunctival cytodiagnosis
1. Tear cytology is rapid and easy to perform: A few microliters of tears collected from the external canthus with a glass capillary are immediately placed on a precolored slide. The presence of even one eosinophil is highly indicative of an allergic pathology, while their absence does not exclude an allergic diagnosis. Tear immunoglobulin E (IgE) tests are not yet available for office measurement.
2. Conjunctival scraping is performed by scraping the conjunctiva with a spatula and looking for the differentiation of intracytoplasmic inclusion
bodies. This procedure is performed when there is a suspicion of
Chlamydia or in combination with immunofluorescence when looking for viruses.
3. Conjunctival biopsy is required for histologic and immunohistochemical analyses necessary for diagnosis of autoimmune diseases such as ocular pemphigoid.
IV. SPECTRUM OF MAST-CELL MEDIATED DISORDERS OF THE EYE
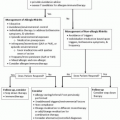
Ocular allergy includes several overlapping conditions that include seasonal (intermittent < 4 weeks of symptoms) and perennial (persistent > 4 weeks in duration) allergic conjunctivitis, vernal conjunctivitis, giant papillary conjunctivitis, and AKC, all of which appear to be part of a clinical spectrum ranging from acute non-sight-threatening to chronic sight-threatening disorders. This clinical spectrum can best be viewed from the perspective of immunologic changes that occur in the conjunctival surface. In
seasonal allergic conjunctivitis, the change is a visible increase in the type and number of cells provoking allergy symptoms at particular times of the year. These cells include mast cells, eosinophils, and other cells that interact and release a variety of allergic mediators including histamine, leukotrienes, and prostaglandins when exposed to various airborne allergens (aeroallergens). In contrast,
perennial allergic conjunctivitis is associated with a persistent increase in the number of these allergy-mediating cells throughout the year. In
vernal conjunctivitis, there is a seasonally recurrent increase in mast cells, eosinophils, and lymphocytes.
Giant papillary conjunctivitis has similar features but is directly related to the presence of objects irritating the eye, such as contact lenses. Finally, in
AKC, there is chronic invasion of the immune cells into the conjunctiva that is seen in middle-aged and older patients with extensive allergic disorders, specifically eczema and asthma. Although contact conjunctivitis is purely a lymphocytic-mediated type of reaction like other delayed type hypersensitivity reactions, it is also presented in this section as a common clinical hypersensitivity reaction seen by the allergist/clinical immunologist.
Table 7-2 provides an overview of the spectrum of ocular allergic disorders, their signs and symptoms, and their salient features.
Table 7-3 describes various inflammatory conditions that involve either the outside or the inside of the eye. The table focuses on the signs and symptoms of external causes of the red eye, which include the predominant cell type found in the conjunctival scraping, the presence or absence of chemosis, lymph node involvement, cobblestoning of the conjunctival surface, discharge, lid involvement, pruritus, gritty sensation, and seasonal variation.
A. Seasonal/intermittent and perennial/persistent
1. Basic mechanisms. Because of the direct exposure of the ocular mucosal surfaces to the environment, mast cell- and IgE-mediated reactions are the most common hypersensitivity responses of the eye. Approximately 50 million mast cells are in the ocular and adnexal tissue in each human eye. Conjunctival angioedema is frequently seen in hypersensitivity reactions, and conjunctival late-phase reactions can occur.
2. History, physical examination, laboratory findings, and differential diagnosis. Seasonal and perennial allergic conjunctivitis are the most prevalent forms of ocular allergy, with seasonal allergic conjunctivitis being more common. Grass pollen produce more ocular symptoms than other aeroallergens. Conjunctival symptoms include itching,
tearing, and burning as well as corneal symptoms of photophobia and blurring of vision. Clinical signs of allergic conjunctivitis include milky or pale pink conjunctivae with vascular congestion, which can progress to conjunctival swelling (
chemosis). A white exudate can form during the acute state, which becomes stringy in the chronic form. Tears can contain histamine and a small number of eosinophils.
B. Atopic keratoconjunctivitis
1. Basic mechanisms. AKC is mediated by a mixture of mast cell, IgE, and lymphocytic interactions along with infiltrations of basophils, eosinophils, plasma cells, and lymphocytes.
2. History, physical examination, laboratory findings, and differential diagnosis. A family history of atopy and its association with atopic dermatitis is common. Symptoms include itching, burning, and tearing. Signs found on physical exam include pale conjunctivae and limbal infiltration (Horners’ points or Trantas’ dots). Laboratory evaluation of the tears can demonstrate the presence of IgE, eosinophils, and mononuclear cells with a paucity of basophils and mast cells. Other abnormalities include increased basophil histamine release, peripheral eosinophilia, and an elevated serum IgE.
3. Complications (sight threatening). Corneal ulceration and scarring, retinal detachment, keratoconus, and cataract formation (8%) can occur in AKC patients. Cataracts are associated with this disease and predominantly involve the anterior portion of the lens and can evolve rapidly into complete opacification within 6 months. Many patients may develop secondary staphylococcal blepharitis.
4. Treatment usually requires a multidisciplinary approach in consultation with an ophthalmologist. Cool compresses are often of limited symptomatic benefit to the patient. Acute exacerbations may require topical and systemic steroids. Topical and sometimes systemic cyclosporine may be required for long-term control. Immunotherapy and mast cell stabilizers with antihistamine activity have been reported in studies to be an adjunctive treatment modality in patients clearly having a seasonal component. Immunotherapy has no apparent effect on the progression of the disease.