Chapter 17 AIDS, Secondary Immunodeficiency and Immunosuppression
• Nutrient deficiencies often lead to impaired immune responses. Malnutrition increases the risk of infant mortality from infection through reduction in cell-mediated immunity, including reduced numbers and function of CD4+ helper cells and a reduction in levels of secretory IgA. Trace elements, iron, selenium, copper, and zinc are also important in immunity. Lack of these elements can lead to diminished neutrophil killing of bacteria and fungi, susceptibility to viral infections, and diminished antibody responses. Vitamins A, B6, C, E, and folic acid are likewise important in overall resistance to infection. Proper diet and nutrition, therefore, reduce morbidity and mortality caused by infection.
• Some drugs selectively alter immune function. Immunomodulatory drugs can severely depress immune functions. These drugs are often necessary to treat solid organ transplant patients and those with an autoimmune disease. Although necessary in such settings, these drugs are often broad acting, thereby increasing patients’ susceptibility to a broad array of opportunistic infections caused by viruses, bacteria and fungi.
• HIV is a primary cause of immunodeficiency. Human immunodeficiency virus (HIV) is a retrovirus that predominantly targets CD4+ T cells. Acute infection depletes CD4 T cell subsets and transiently suppresses circulating CD4 T cell numbers before the immune system establishes partial control of the virus and the chronic phase of infection begins. Though patients can remain in the chronic phase for an average of 10 years, without anti-retroviral drug treatment, CD4 T cell levels gradually fall, resulting in loss of cell-mediated immunity and susceptibility to life-threatening opportunistic infections. This final stage, AIDS (acquired immunodeficiency syndrome), is marked by low CD4 T cell counts, high HIV plasma levels, reactivation of other latent infections, and often, virus-associated malignancies such as Kaposi’s sarcoma and non-Hodgkin’s lymphoma.
• Combination therapy for AIDS with inhibitors of HIV reverse transcriptase, protease, and entry are reasonably successful, but associated with long-term toxicities in almost 50% of persons. An effective vaccine remains an elusive goal, in part due to the rapid mutation rate of the virus during reverse transcription.
Overview
Nutrient deficiencies
Infection and malnutrition can exacerbate each other
• increasing metabolic demands;
• decreasing appetite, thereby lowering intake of nutrients; and
• with gastrointestinal infection, decreasing nutrient absorption.
Once this cycle begins, it is self-propagating as infection compromises immunity, which then leads to more infection and debility (Fig. 17.1). At a population level, this may lead to decreased productivity, further decreasing economic and food resources and, again, driving the malnutrition and immune deficiency loop.
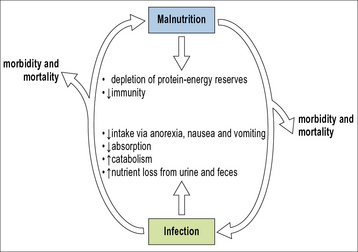
Fig. 17.1 Malnutrition and infection exacerbate each other in a vicious circle
Malnutrition and infection exacerbate each other in a vicious circle.
Protein–energy malnutrition and lymphocyte dysfunction
• the lobular architecture is ill defined;
• there is a loss of corticomedullary demarcation;
• there are fewer lymphoid cells; and
• Hassall’s corpuscles are enlarged and degenerate – some may be calcified.
Nutrition also affects innate mechanisms of immunity
Poor nutrition also causes deficits in innate immune defenses, for example,
• a larger number of bacteria bind to epithelial cells of malnourished subjects;
• the production of certain inflammatory cytokines, such as IL-2 and TNFα, is decreased;
• opsonization is decreased, largely because of a reduction in levels of various complement components – C3, C5, and factor B.
Deficiencies in trace elements impact immunity
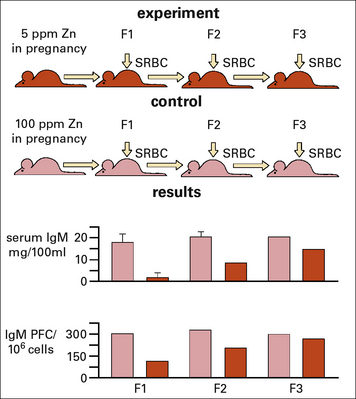
Zinc deficiency during pregnancy has also been shown to have an inter-generational effect on the levels of IgM and IgM producing B cells in the pups, and more surprisingly even in the 2nd generation (Fig. 17.w1).
Q. In what ways can neutrophils and macrophages restrict iron availability for microorganisms?
A. Soluble proteins such as lactoferrin produced by neutrophils reduce the availability of free iron in the phagolysosome. Macrophages have ion pumps (e.g. nRAMP) in their phagosomal membrane that remove iron from the phagosome (see Chapter 15).
Vitamin deficiencies and immune function
Q. NFATc1, a member of the NFAT transcription factor family, is required for development of the B-1 B cell subset. Recent experiments using mice have shown that vitamin A deficiency severely reduces NFAT-c1 expression resulting in loss of the B-1 population. Why might this contribute to defects in mucosal immunity?
Until the advent of antibiotics, cod liver oil and sunlight, both sources of vitamin D, were used as primary treatments for TB. Vitamin D deficiency can lead to increased infection rates and recent studies have begun to elucidate some of the molecular mechanisms behind the anti-infective role of vitamin D. Many cell types express the vitamin D receptor (VDR), and while vitamin D metabolites may modulate adaptive immune responses, they can also enhance innate immunity. Importantly, particularly for TB, signaling via the VDR may enhance both cathelicidin and defensin expression, thus boosting macrophage anti-microbial activity (Chapter 7).
Immunodeficiency secondary to drug therapies
Several classes of drugs suppress immune function, either intentionally for therapeutic effect, or as an unwanted side effect.. For example, patients receiving organ transplants usually receive a variety of immunosuppressants to prevent rejection of the donor tissue and to treat graft-versus-host disease (GvHD, discussed in Chapter 21). Likewise, patients presenting with severe inflammatory, allergic, or autoimmune reactions often require therapeutic immunosuppression (Chapter 20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree